Translate this page into:
A clinical evaluation of low-level laser therapy for pain reduction in early treatment stages: A pilot study

*Corresponding author: Giuseppe Minervini, Multidisciplinary Department of Medical-Surgical and Dental Specialties, University of Campania Luigi Vanvitelli, Naples, Italy. giuseppe.minervini@unicampania.it
-
Received: ,
Accepted: ,
How to cite this article: Akash LP, Kamble P, Agrawal JM, Vijapure S, Alansari RA, Uzunçıbuk H, et al. A Clinical evaluation of low-level laser therapy for pain reduction in early treatment stages: A pilot study. APOS Trends Orthod. 2025;15:166-72. doi: 10.25259/APOS_26_2024
Abstract
Objectives:
This study aimed to clinically evaluate the efficacy of low-level laser therapy (LLLT) in reducing pain associated with orthodontic movement during the early stages of treatment.
Material and Methods:
A randomized controlled trial was conducted with 20 participants undergoing non-extraction orthodontic treatment. The laser group (LG, n = 10) received LLLT (808 nm, 100 mW) immediately after appliance installation, while the control group (CG, n = 10) received no pain control intervention. Pain levels were assessed using a visual analog scale (VAS) at 6, 24, 48, and 72 h till 7 days with an interval of 24 h. Statistical analyses included Chi-square tests and Mann–Whitney tests.
Results:
The LG consistently demonstrated significantly lower pain scores during chewing and at rest compared to the CG. After 6 h post-treatment, the median pain score on chewing in the LG was markedly lower than the CG (P < 0.001), a trend observed at each subsequent interval till 7 days. The comparison of spontaneous pain also favored the LG at various time points. Lower median VAS scores for pain on chewing among the LG and CG were zero and two, respectively, with a significant difference. The maximum median VAS scores for pain on chewing among the LG and CG were five and seven, respectively, with a significant difference.
Conclusion:
This study provides robust evidence supporting the effectiveness of LLLT in reducing orthodontic pain during the early stages of treatment. The sustained and significant reduction in pain scores, coupled with rigorous statistical analyses, emphasizes the potential of LLLT as a valuable adjunctive therapy in orthodontic practice.
Keywords
Orthodontics
Low-level laser therapy
Pain management
Inflammatory response
Visual analog scale
INTRODUCTION
Orthodontic treatment, a common therapeutic intervention for correcting malocclusion and dental misalignment is often associated with discomfort and pain, especially in the initial stages. Pain during orthodontic treatment is primarily attributed to the inflammatory response triggered by the mechanical forces exerted on the teeth and surrounding tissues.[1,2] Patients commonly report soreness, tenderness, and pain, leading to a potential decrease in treatment adherence and overall patient satisfaction.[3–5] Consequently, efforts to alleviate orthodontic-related pain have garnered significant attention, and one emerging modality showing promise in this context is low-level laser therapy (LLLT).
Orthodontic pain arises due to the inflammatory mediators released during the remodeling processes that occur in response to orthodontic forces applied to the teeth. These forces lead to cellular and molecular changes in the periodontal ligament and surrounding tissues, resulting in the release of prostaglandins, histamines, and other inflammatory substances.[6–8] The subsequent inflammatory response activates pain receptors, contributing to the sensation of pain and discomfort.[9] Understanding the etiology of orthodontic pain is crucial for developing effective strategies to manage and mitigate its impact on patients.
LLLT, also known as photobiomodulation, involves the application of low-intensity lasers or light-emitting diodes (LEDs) to stimulate cellular processes and promote tissue healing.[10–12] LLLT has gained popularity in various medical and dental fields for its anti-inflammatory, analgesic, and biostimulatory effects. The mechanism of action involves the absorption of light energy by cellular chromophores, leading to physiological responses at the cellular and molecular levels. [13–15] In the context of orthodontics, LLLT has emerged as a potential adjunctive therapy to alleviate pain and accelerate the tissue healing process associated with orthodontic adjustments.[16–18]
The application of LLLT in orthodontics aligns with the growing trend of incorporating evidence-based and patient-centered approaches in dental care. Patient comfort and satisfaction are integral components of orthodontic treatment success, and strategies to minimize pain and discomfort contribute to a positive patient experience.[19,20] Considering the potential benefits of LLLT, its integration into orthodontic practice has the potential to enhance patient outcomes and treatment adherence.
Despite the accumulating evidence supporting the efficacy of LLLT in reducing orthodontic pain, variations in study designs, laser parameters, and outcome measures necessitate a comprehensive evaluation of the existing literature. A critical examination of the available evidence will contribute to a deeper understanding of the role of LLLT in orthodontic pain management and guide clinicians in optimizing its use within orthodontic protocols.
This study aims to clinically evaluate the effectiveness of LLLT in reducing pain caused by orthodontic movement in the early stages of treatment.
MATERIAL AND METHODS
The study was designed to clinically assess the effectiveness of LLLT in alleviating pain associated with orthodontic movement during the initial stages of treatment.
Ethical considerations were addressed by obtaining informed consent from all participants, and the study protocol received approval from the relevant ethics committee. The research was conducted in accordance with the Helsinki Declaration and Bharati Vidyapeeth (Deemed to be University) Dental College and Hospital approved the protocol (Protocol number: BV [DU] MC&Sangli/IEC/19–49/21, Date: 03/02/2021). The study adhered to rigorous ethical guidelines to ensure participant safety and confidentiality.
The study included 20 individuals who met specific inclusion criteria: requiring non-extraction orthodontic treatment using pre-adjusted fixed appliances with a 0.022″ slot; initiating the alignment and leveling phase with the 0.012″ thermoactivated nickel-titanium archwire (Libral Traders Pvt. Ltd. India); not taking medication that could impact the study results; maintaining good oral and general health; and providing signed informed consent, indicating their agreement with the research procedures.
Participants were randomly allocated to the laser group (LG) and control group (CG). The LG (n = 10) received low-level laser irradiation (808 nm, 100 mW) immediately after appliance installation, while the CG (n = 10) received no pain control intervention post-installation.
A power analysis was conducted to determine the appropriate sample size for this clinical study. The calculation was based on the expected effect size, significance level, and desired power of the statistical tests. Assuming an effect size of 0.8, a significance level (α) of 0.05, and a desired power (1-β) of 0.80, the estimated sample size was determined to be 20 participants, with 10 participants in each group (LG and CG). This sample size provides adequate statistical power to detect significant differences in pain scores between the two groups, ensuring the reliability and validity of the study findings.
The gallium-aluminum-arsenides infrared laser used in this study operated at a wavelength of 808 nm, with a cross-sectional beam diameter measuring 3 mm. This laser device, identified as Novolase Gold, Novolase Technologies, India, was configured to a power level of 100 mW.
The laser therapy was administered as a single session, promptly following the bonding of brackets and the installation of the initial orthodontic archwire (0.012″ thermoactivated nickel-titanium). Each session of irradiation lasted for an average duration of 19.5 min, focusing on the distal region of the first molar to the corresponding region on the opposite first molar. Specifically, three points situated between the roots and distal spaces of the first molar – cervical, middle, and apical – on both the buccal and lingual/palatal sides, where the orthodontic appliance was affixed, were subjected to 15 s of irradiation each. This equated to 1.5 J/cm2 of energy delivered per tooth, with a total of 12 irradiations administered to each tooth. The cumulative energy dosage per tooth amounted to 18 J.
Pain levels were assessed using a 100 mm horizontal visual analog scale (VAS), segmented into three points, each marked with descriptors (smiley expressions): 0 (zero) denoting no pain, 5 (five) indicating moderate pain, and 10 (ten) signifying severe pain. Patients were instructed to place a vertical mark on the scale corresponding to their pain level at 06, 24, 48, and 72 h up to 7 days at intervals of 24 h post-orthodontic appliance installation.
Participants completed a questionnaire, recording VAS scores at the specified intervals and detailing their pain perception concerning laser therapy, including the initiation, peak intensity, decline, and absence of pain. Patients indicated the day and time when they experienced these pain levels.
All participants were informed that taking painkillers was not prohibited. However, if they chose to use painkillers, they were required to disclose the specific medication in the questionnaire, and those who did so were excluded from the sample.
Statistical analysis
The obtained data were statistically analyzed with the Statistical Package for the Social Sciences version 21.0. The tests applied included Chi-square tests for intergroup comparability and Mann–Whitney tests for pain symptomatology and perception. P < 0.05 was considered as statistically significant.
RESULTS
The demographic details of the study participants are mentioned in [Table 1]. There were 11 male (mean age 19.36 ± 4.13 years) and 9 female subjects (mean age 18.67 ± 1.80 years). [Table 2 and Figure 1] present the comparison of pain on chewing (VAS score) among subjects treated with laser and without laser therapy. After 6 h post-treatment, the median pain score on chewing among subjects receiving laser therapy was significantly lower as compared to the median pain score on chewing among subjects who did not receive laser therapy (P < 0.001). Similarly, the median pain score on chewing among subjects receiving laser therapy was significantly lower as compared to the median pain score on chewing among subjects who did not receive laser therapy for up to 7 days (P < 0.001).
| Gender | n | Minimum age | Maximum age | Mean±SD |
|---|---|---|---|---|
| Male | 11 | 14 | 27 | 19.36±4.13 |
| Female | 9 | 16 | 21 | 18.67±1.80 |
SD: Standard deviation
| Time | With laser-on mastication |
Without laser-on mastication |
P-value | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 6 h | 4.5 | 1 | 7 | 0 | <0.001* |
| 1 day | 4 | 2 | 7 | 2 | <0.001* |
| 2 days | 3 | 1 | 5.5 | 1 | <0.001* |
| 3 days | 3 | 1 | 5 | 1 | <0.001* |
| 4 days | 1 | 0 | 5 | 2 | <0.001* |
| 5 days | 1 | 2 | 4 | 1 | <0.001* |
| 6 days | 0 | 1 | 2 | 1 | <0.001* |
| 7 days | 0 | 1 | 2 | 2 | <0.001* |
Mann Whitney test, *Indicates a significant difference at P≤0.05. IQR: Interquartile range, VAS: Visual analog scale
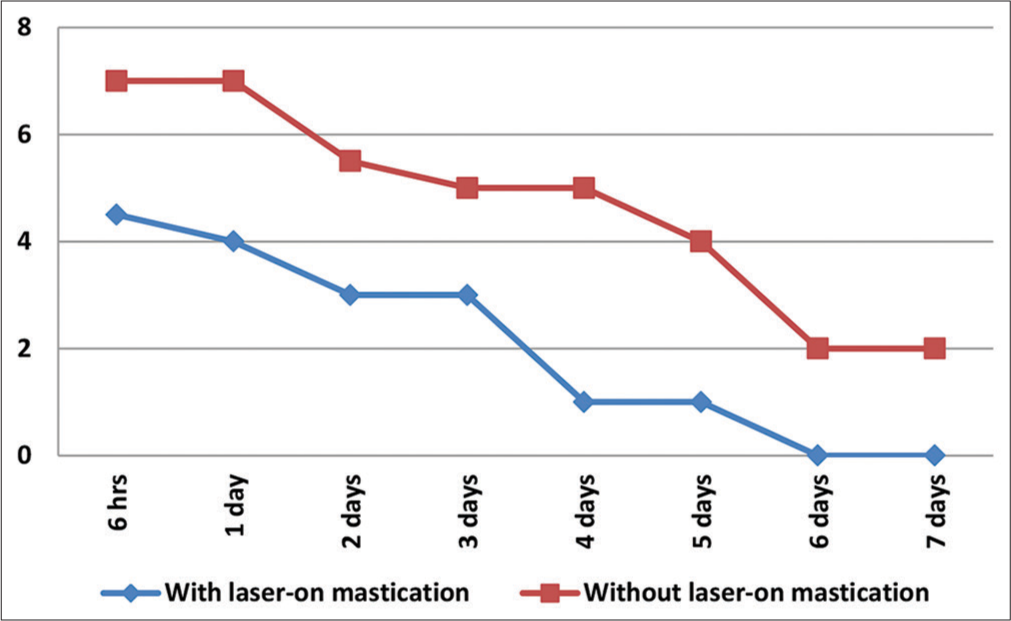
- Median pain on chewing VAS (visual analog scale score).
The comparison of spontaneous pain (VAS score) among the subjects treated with laser and without laser therapy is presented in [Table 3 and Figure 2]. After 6 h post-treatment, the median pain score among the subjects receiving laser therapy was significantly lower as compared to the median pain score on chewing among subjects who did not receive laser therapy (P < 0.001). Similarly, the median pain score among subjects receiving laser therapy was significantly lower as compared to the median pain score on chewing among subjects who did not receive laser therapy after 1 day and 2 days post-treatment. On post-treatment, 3rd day, and onward, the difference in spontaneous pain among the two groups were not statistically significant.
| Time | With laser | Without laser | P-value | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 6 h | 4 | 1 | 7 | 0 | <0.001* |
| 1 day | 3.5 | 2 | 7 | 1 | <0.001* |
| 2 days | 3 | 2 | 4 | 2 | 0.001* |
| 3 days | 2 | 1 | 2 | 2 | 0.093 |
| 4 days | 1 | 0 | 1 | 1 | 0.069 |
| 5 days | 1 | 1 | 1 | 2 | 0.673 |
| 6 days | 0 | 1 | 0 | 1 | 0.857 |
| 7 days | 0 | 1 | 0 | 1 | 0.522 |
Mann Whitney test, *Indicates a significant difference at P≤0.05. IQR: Interquartile range, VAS: Visual analog scale
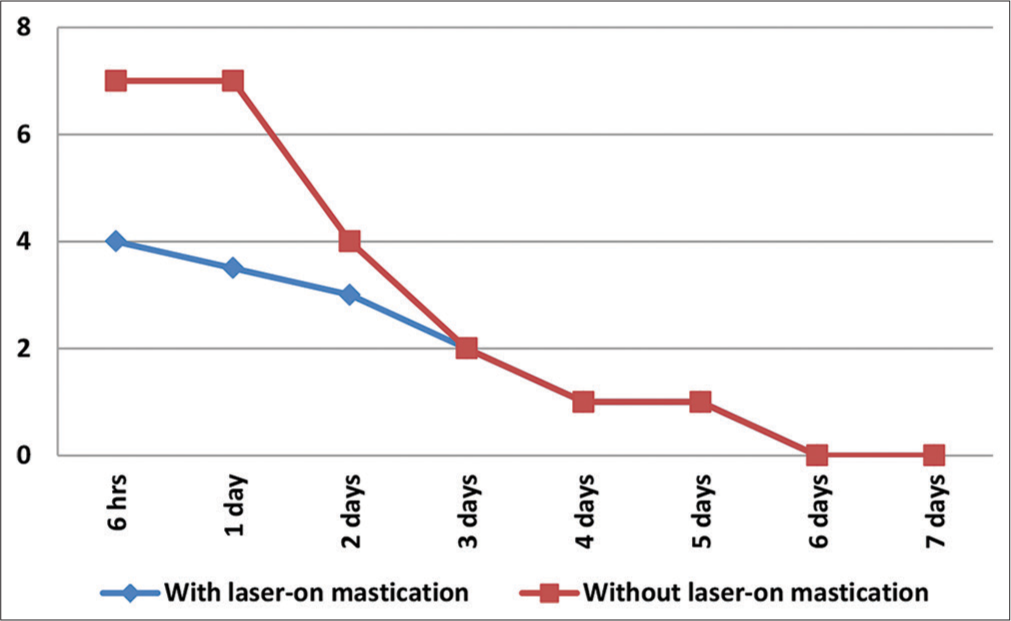
- Median spontaneous pain VAS (visual analog scale score).
Results showed that lower median VAS scores for pain on chewing among the subjects with and without laser therapy were zero and two, respectively, and there was a significant difference in the lowest median pain on chewing scores among the two groups. However, a comparison of the lowest spontaneous pain score among the two groups showed a non-significant difference [Table 4]. The maximum median VAS scores for pain on chewing among the subjects with and without laser therapy were five and seven, respectively, and there was a significant difference in the lowest median pain on chewing scores among the two groups. The maximum median VAS scores for spontaneous pain among the subjects with and without laser therapy were four and seven, respectively, and there was a significant difference in the maximum median spontaneous pain scores among the two groups [Table 5].
| Variable | Group | Median | IQR | P-value |
|---|---|---|---|---|
| Pain on chewing | With laser | 0 | 0.75 | <0.001* |
| W/o laser | 2 | 1 | ||
| Spontaneous pain | With laser | 0 | 1 | 0.268 |
| W/o laser | 0 | 0 |
Mann Whitney test, *Indicates a significant difference at P≤0.05. IQR: Interquartile range, VAS: Visual analog scale
| Variable | Group | Median | IQR | P-value |
|---|---|---|---|---|
| Pain on chewing | With laser | 5 | 1 | <0.001* |
| W/o laser | 7 | 1 | ||
| Spontaneous pain | With laser | 4 | 1.25 | <0.001* |
| W/o laser | 7 | 0 |
Mann–Whitney test, *Indicates a significant difference at P≤0.05. IQR: Interquartile range, VAS: Visual analog scale
[Table 6] compares the number of subjects with a complete absence of pain. There were 15 subjects in the LG who showed a complete absence of pain on chewing as compared to only three subjects who did not receive any laser therapy. This difference in the number of subjects with a complete absence of pain among the two groups was significant. There was a non-significant difference in the number of subjects who showed a complete absence of spontaneous pain among the two groups.
| Variable | Group | Yes (%) | No (%) | P-value |
|---|---|---|---|---|
| Pain on chewing | With laser | 15 (75) | 5 (25) | <0.001* |
| W/o laser | 3 (15) | 17 (85) | ||
| Spontaneous pain | With laser | 17 (77.3) | 5 (22.7) | 0.510 |
Chi-square test; *Indicates a significant difference at P≤0.05
DISCUSSION
Orthodontic pain is a common concern during treatment, impacting patient comfort and satisfaction. The inflammatory response triggered by mechanical forces plays a pivotal role in this discomfort.[9] While various strategies have been explored to alleviate orthodontic-related pain, LLLT has emerged as a promising modality with anti-inflammatory and analgesic effects.[21–23]
The etiology of orthodontic pain is rooted in the inflammatory mediators released during tissue remodeling in response to applied forces. Prostaglandins, histamines, and other inflammatory substances contribute to the activation of pain receptors, leading to discomfort and tenderness.[24] Traditional approaches to pain management involve the use of analgesics;[25,26] however, the quest for nonpharmacological interventions has led to the exploration of therapies like LLLT.
LLLT, also known as photobiomodulation, operates on the principle of applying low-intensity lasers or LEDs to stimulate cellular processes and enhance tissue healing.[27,28] The mechanism involves the absorption of light energy by cellular chromophores, initiating physiological responses at the cellular and molecular levels.[10] In orthodontics, LLLT’s potential lies in its ability to mitigate the inflammatory response associated with orthodontic adjustments, providing relief to patients.[29,30]
The study’s design adhered to ethical considerations, obtaining informed consent and approval from the relevant ethics committee. The use of a VAS for pain assessment at specified intervals up to 7 days post-treatment ensured a systematic evaluation of pain levels. The participants were selected based on specific criteria, including the absence of medications influencing results and good oral and general health, enhancing the study’s internal validity.
The comparison of pain on chewing (VAS score) among subjects treated with and without laser therapy demonstrated consistent and significant reductions in pain levels in the LG at various time intervals. These findings align with the previous studies highlighting the efficacy of LLLT in pain reduction during orthodontic treatment.[31-34]
Spontaneous pain, another crucial aspect of orthodontic discomfort, also exhibited a significant reduction in the LG, particularly during the initial post-treatment period. This aligns with the proposed anti-inflammatory effects of LLLT, mitigating the molecular and cellular changes that contribute to spontaneous pain.[35,36] However, it is noteworthy that the difference in spontaneous pain between the two groups diminished on the 3rd day post-treatment. This could be attributed to the transient nature of the analgesic effect of LLLT, suggesting that repeated sessions might be beneficial for sustained pain relief.
The analysis of the least and maximum VAS scores for pain on chewing and spontaneous pain provides valuable insights. The significantly lower minimum and maximum scores in the LG underscore LLLT’s potential to not only reduce overall pain but also limit its variability. This consistency in pain reduction is crucial for enhancing the predictability of patient experiences during orthodontic treatment.[37-39]
The number of subjects with complete absence of pain on chewing demonstrated a compelling advantage for the LG. A 75% rate of complete pain absence in the LG compared to 15% in the CG indicates a substantial clinical impact. This suggests that LLLT might not only reduce pain but also contribute to a more comfortable orthodontic experience for a significant proportion of patients.[19,40]
While the findings of this study are promising, it is essential to contextualize them within the broader landscape of existing literature. Previous research on LLLT in orthodontics has shown varying results, with some studies reporting significant pain reduction,[41,42] while others indicate LLLT is not effective in pain reduction following initial orthodontic archwire placement.[43–47] The variations could be attributed to differences in study designs, laser parameters, and outcome measures.
The duration and timing of LLLT application are critical factors influencing its efficacy. In the present study, LLLT was applied once, post-bracket bonding and archwire installation. This protocol aligns with some studies demonstrating positive effects with a single application.
The findings of this study hold significant clinical implications for orthodontic practice. The demonstrated effectiveness of LLLT in reducing orthodontic pain suggests its potential as a valuable adjunctive treatment during the early stages of orthodontic interventions. Orthodontists can consider integrating LLLT into their treatment protocols to enhance patient comfort and satisfaction. By alleviating pain associated with orthodontic adjustments, LLLT may contribute to improved treatment adherence, positively influencing overall patient experiences. This non-invasive and low-risk therapeutic modality could be particularly beneficial for patients who are more sensitive to pain or those with lower pain tolerance. In addition, the study’s exploration of different pain parameters, including pain on chewing and spontaneous pain, provides a nuanced understanding of LLLT’s effects, allowing clinicians to tailor its use based on specific patient needs. While further research is warranted, the positive outcomes of this study suggest that LLLT has the potential to become a valuable tool in the hands of orthodontic practitioners seeking to optimize patient care and treatment outcomes.
This study exhibits several strengths, contributing to the credibility and reliability of its findings. A key strength lies in the rigorous methodology employed, featuring a randomized controlled trial design. This robust approach enhances the study’s internal validity, providing a solid foundation for concluding the impact of LLLT on orthodontic pain. Pain assessment using a VAS at multiple time points, up to 7 days post-treatment, offers a detailed and nuanced understanding of the temporal dynamics of pain relief. By examining various aspects of pain, such as pain on chewing and spontaneous pain, and analyzing least and maximum VAS scores, the study provides a comprehensive evaluation of LLLT’s effects on different facets of orthodontic discomfort.
The study’s limitations include a relatively small sample size, which could potentially limit the generalizability of findings. In addition, the use of a single laser type and parameters might not capture the broader spectrum of LLLT modalities employed in clinical practice.
The promising outcomes of this study pave the way for intriguing future perspectives in the realm of orthodontic pain management. As the field of LLLT continues to evolve, future research could delve into optimizing laser parameters, such as wavelength, power, and duration, to establish standardized protocols that maximize efficacy. Exploring the long-term effects of LLLT on orthodontic pain and patient-reported outcomes could provide valuable insights into its sustained benefits over extended treatment periods. In addition, investigating the mechanisms behind LLLT’s impact on inflammatory processes in orthodontic tissues may unravel novel pathways for pain modulation. Comparative studies evaluating LLLT against other pain management modalities, such as analgesic medications or alternative physical therapies, could further inform evidence-based decision-making in orthodontic care. As technology advances, the development of portable or at-home LLLT devices may offer convenience to patients, potentially enhancing treatment compliance. Collaborative efforts between orthodontic practitioners and researchers can collectively contribute to refining and expanding the role of LLLT in orthodontic practice, ultimately shaping more patient-centered and effective approaches to orthodontic pain management.
CONCLUSION
This study provides valuable insights into the effectiveness of LLLT in reducing orthodontic pain during the early stages of treatment. The findings, coupled with a comprehensive analysis of existing literature, underscore the potential of LLLT as a valuable adjunctive therapy in orthodontic practice. While further research is warranted to refine protocols and address existing variations, the current evidence suggests that LLLT holds promise in enhancing patient comfort and satisfaction during orthodontic treatment.
Availability of data and materials
The data will be available upon reasonable request from the corresponding author.
Ethics approval
This study was approved by the Ethical Committee of Bharati Vidyapeeth (Deemed to be University) Dental College and Hospital and (Protocol Number: BV (DU) MC&Sangli/IEC/19-49/21 Date: 03/02/2021).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Adverse effects of orthodontic treatment: A clinical perspective. Saudi Dent J. 2011;23:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of pain levels on patients undergoing fixed orthodontic treatment with 2 different self-ligating bracket systems. Turk J Orthod. 2023;36:239-47.
- [CrossRef] [PubMed] [Google Scholar]
- Pain and discomfort perceived during the initial stage of active fixed orthodontic treatment. Saudi Dent J. 2015;27:81-7.
- [CrossRef] [PubMed] [Google Scholar]
- Computer-guided osteotomy with simultaneous implant placement and immediately loaded full-arch fixed restoration: A case report. Prosthesis. 2023;5:221-33.
- [CrossRef] [Google Scholar]
- Same-day digital dentistry restorative workflow for single immediate provisionalization of narrow-diameter implants: An exploratory prospective study. Prosthesis. 2023;5:197-207.
- [CrossRef] [Google Scholar]
- Is inflammation a friend or foe for orthodontic treatment?: Inflammation in orthodontically induced inflammatory root resorption and accelerating tooth movement. Int J Mol Sci. 2021;22:2388.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular diagnosis of osteoarticular implant-associated infection: Available techniques and how we can use them. Prosthesis. 2022;5:1-12.
- [CrossRef] [Google Scholar]
- Early treatment of class II division 1 malocclusions with prefabricated myofunctional appliances: A case report. Prosthesis. 2023;5:1049-59.
- [CrossRef] [Google Scholar]
- Current advances in orthodontic pain. Int J Oral Sci. 2016;8:67-75.
- [CrossRef] [PubMed] [Google Scholar]
- Photobiomodulation-underlying mechanism and clinical applications. J Clin Med. 2020;9:1724.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative treatment of temporomandibular joint condylar fractures: A systematic review conducted according to PRISMA guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. J Oral Rehabil. 2023;50:886-93.
- [CrossRef] [PubMed] [Google Scholar]
- Post-traumatic stress, prevalence of temporomandibular disorders in war veterans: Systematic review with meta-analysis. J Oral Rehabil. 2023;50:1101-9.
- [CrossRef] [Google Scholar]
- Aminoacyltransferase stimulation of protein synthesis by pig adrenal polysomes. Nature. 1967;214:91-2.
- [CrossRef] [PubMed] [Google Scholar]
- The association between parent education level, oral health, and oral-related sleep disturbance. An observational cross-sectional study. Eur J Paediatr Dent. 2023;24:218-23.
- [Google Scholar]
- Prevalence of temporomandibular disorders (TMD) in obesity patients: A systematic review and meta-analysis. J Oral Rehabil. 2023;50:1544-53.
- [CrossRef] [Google Scholar]
- The effects and mechanisms of PBM therapy in accelerating orthodontic tooth movement. Biomolecules. 2023;13:1140.
- [CrossRef] [PubMed] [Google Scholar]
- Contemporary orthodontic workflows: A panacea for efficiency? Semin Orthod. 2023;29:1-3.
- [CrossRef] [Google Scholar]
- What's “Trend”ing in orthodontic literature? APOS Trends Orthod. 2016;6:1-4.
- [CrossRef] [Google Scholar]
- The protocol of low-level laser therapy in orthodontic practice: A scoping review of literature. J Int Soc Prev Community Dent. 2022;12:267-86.
- [Google Scholar]
- Children oral health and parents education status: A cross sectional study. BMC Oral Health. 2023;23:787.
- [CrossRef] [PubMed] [Google Scholar]
- Does low level laser therapy relieve the pain caused by the placement of the orthodontic separators?-A meta-analysis. Head Face Med. 2015;11:28.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis in childhood cancer survivors: Physiopathology, prevention, therapy and future perspectives. Cancers (Basel). 2022;14:4349.
- [CrossRef] [PubMed] [Google Scholar]
- The safety of blinatumomab in pediatric patients with acute lymphoblastic leukemia: A systematic review and meta-analysis. Front Pediatr. 2022;10:929122.
- [CrossRef] [PubMed] [Google Scholar]
- Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 2006;129:469.e1-32.
- [CrossRef] [PubMed] [Google Scholar]
- The pain management in orthodontics. J Clin Diagn Res. 2013;7:1258-60.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 infection in children and infants: Current status on therapies and vaccines. Children (Basel). 2022;9:249.
- [CrossRef] [PubMed] [Google Scholar]
- Laser in dentistry: An innovative tool in modern dental practice. Natl J Maxillofac Surg. 2012;3:124.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontic treatment of an unerupted mandibular canine tooth in a patient with mixed dentition: A case report. J Med Case Rep. 2016;10:170.
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of low-level laser therapy in dentistry: A review. Cureus. 2022;14:e28799.
- [CrossRef] [Google Scholar]
- Digitalization era of dental education: A systematic review. Dent Med Probl. 2023;60:513-25.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci. 2014;29:559-64.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level laser therapy for treatment of pain associated with orthodontic elastomeric separator placement: A placebo-controlled randomized double-blind clinical trial. Photomed Laser Surg. 2013;31:10-6.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of a single versus double application of low-level laser therapy in pain reduction following orthodontic elastomeric separation: A randomized controlled trial. Dent Med Probl. 2020;57:45-52.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level laser therapy effects on pain perception related to the use of orthodontic elastomeric separators. Dental Press J Orthod. 2015;20:37-42.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials. 2005;26:3503-9.
- [CrossRef] [PubMed] [Google Scholar]
- The COVID-19 pandemic and its global effects on dental practice, An International survey. J Dent. 2021;114:103749.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of pain perception during orthodontic debonding of metallic brackets with four different techniques. J Appl Oral Sci. 2019;27:e20180003.
- [CrossRef] [PubMed] [Google Scholar]
- Tissue fluorescence imaging (VELscope) for quick non-invasive diagnosis in oral pathology. J Craniofac Surg. 2017;28:e112-5.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of dental students' knowledge, attitudes and behaviors regarding COVID-19 infection: A cross-sectional survey. Minerva Dent Oral Sci. 2023;72:144-53.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 is a new challenge for dental practitioners: Advice on patients' management from prevention of cross infections to telemedicine. Open Dent J. 2020;14:298-304.
- [CrossRef] [Google Scholar]
- Efficacy of low-level laser therapy in reducing pain in the initial stages of orthodontic treatment. Int J Dent. 2022;2022:3934900.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of a virtual prosthodontic project realized through a 2D and 3D photographic acquisition: An experimental study on the accuracy of different digital systems. Int J Environ Res Public Health. 2019;16:5139.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level laser therapy effectiveness in reducing initial orthodontic archwire placement pain in premolars extraction cases: A single-blind, placebo-controlled, randomized clinical trial. BMC Oral Health. 2020;20:209.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of low-level laser therapy during tooth movement: A randomized clinical trial. Materials (Basel). 2019;12:2187.
- [CrossRef] [PubMed] [Google Scholar]
- TIP, TORQUE & ROTATIONS: How accurately do digital superimposition software packages quantify tooth movement? Prog Orthod. 2022;23:8.
- [CrossRef] [PubMed] [Google Scholar]
- Customized adjuncts with clear aligner therapy: “The Golden Circle Model” explained! J World Fed Orthod. 2022;11:216-25.
- [CrossRef] [PubMed] [Google Scholar]
- Use of laser systems in orthodontics. Turk J Orthod. 2020;33:133-40.
- [CrossRef] [PubMed] [Google Scholar]







