Translate this page into:
Bimaxillary protrusion and gummy smile treated with clear aligners: Closing premolar extraction spaces with bone screw anchorage

*Corresponding author: Lexie Y. Lin, Beethoven Orthodontic Center, Hsinchu, Taiwan. lexielin2020@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Lin LY, Chang CH, Roberts WE. Bimaxillary protrusion and gummy smile treated with clear aligners: Closing premolar extraction spaces with bone screw anchorage. APOS Trends Orthod 2020;10(2):120-31.
Abstract
Inadequate posterior anchorage is a serious limitation for aligner treatment involving extraction of four first premolars. Inappropriate axial inclinations may compromise intermaxillary occlusion and stability. OrthoBoneScrew® (OBS) anchorage is designed to augment the Invisalign® clear aligner G6 solution to produce more predictable outcomes as illustrated by the current case report. An 18-year-old female presented with two chief complains: (1) Protrusive, incompetent lips, and (2) excessive gingival exposure when smiling (“gummy smile”). Clinical evaluation revealed bimaxillary protrusion, hypermentalis activity, anterior crowding, and excessive anterior axial inclinations, particularly of the lower incisors (116°). The American Board of Orthodontic (ABO) discrepancy index (DI) was 21. The treatment plan was extraction of all four first premolars, and clear aligner (Invisalign®) therapy anchored with four OBSs: Infra-zygomatic crest (IZC), and between the roots of the upper central and lateral incisors (Incisal) bilaterally. Eighteen months of initial treatment with 45 aligners retracted and intruded the anterior segments in both arches by closing the extraction spaces with supplemental anchorage provided by IZC and Incisal OBSs. The final series of 20 refinement aligners achieved an excellent outcome as evidenced by an ABO cast-radiograph evaluation (CRE) score of 10, and a pink and white (P&W) dental esthetic score of 3. Post-treatment analysis revealed multiple opportunities for improvement. The patient was well satisfied with the final outcome.
Keywords
Bimaxillary protrusion
Gummy smile
Premolar extraction
Clear aligner treatment
Invisalign G6
Infra-zygomatic crest
Incisal
Bone screws
Space closure
Anchorage
Torque control
INTRODUCTION
Modern aligner therapy has expanded the treatment perspective for managing complex malocclusions with removable appliances. The Invisalign® system (Align Technology, Inc., San Jose, CA, USA) is a leader in the applied technology. Over the years, clinical opinions of aligner therapy have progressed from doubtful[1] to reserved,[2] and they are now progressing to an evolving consensus that aligner therapy is an efficient solution for mild-to-moderate malocclusions.[3] Although some complex malocclusions have been treated with aligners,[4,5] the results are less accurate and predictable than treatment with fixed appliances.[6]
One of the more challenging clinical scenarios for aligners is the treatment of extraction cases. In particular, root paralleling after space closure is inconsistent.[7] Tipped teeth can be corrected with fixed appliances, but sequential treatment with two modalities may require more treatment time than with fixed appliances alone.[8,9]
To improve clinical outcomes particularly for extraction of first premolars, Align Technology released the G6 protocol along with SmartStage® in 2015.[10] The principle of differential moments (couples produced with coordinated sets of attachments) is used for Invisalign® G6 to provide anterior retraction with maximum posterior anchorage.[11] SmartStage® is engineered to optimize the progression of tooth movement based on algorithms developed with a massive data base.[12] The force system for G6 is indeterminate mechanics which are not intuitive. If a clinician accepts the G6 protocol with optimized attachments, the treatment plan cannot be changed.
The successful completion of treatment with the G6 protocol is followed at chairside.[13] However, a recent study conducted by Peking University reported that G6 showed molar anchorage loss that was similar to conventional attachments.[14] The retraction of incisors was less than predicted, and there were multiple side effects such as lingual tipping and extrusion.[14] The difference between the ClinCheck® prediction and the actual outcome was similar to loss of torque with fixed appliances due to the play between archwires and brackets slots.[15]
Clinicians who prescribe Invisalign® treatment still have much to learn regarding the biomechanics and efficacy of the system.[2] Clear aligner treatment can be enhanced with auxiliaries designed to improve the predictability of outcomes.[16] The aim for the present case report is to demonstrate the potential for OrthoBoneScrews® (OBSs) (iNewton Dental, Ltd., Hsinchu City, Taiwan) in supplementing anchorage. The authors feel this approach may evolve to be the “gold standard” for patients who demand inconspicuous aligner therapy for demanding malocclusions requiring extractions in all four quadrants.
The dental nomenclature for this report is the modified Palmer notation. Upper (U) and lower (L) arches, as well as the right (R) and left (L) sides, define the four oral quadrants: UR, UL, LR, and LL. Teeth are numbered 1–8 from the midline in each quadrant, for example, a lower right first molar is LR6.
DIAGNOSIS
An 18-year-old female presented with chief complaints of protrusive lips and a gummy smile tendency, which affected her confidence and productivity. The patient had no significant medical or dental history. Oral hygiene was acceptable, and her motivation for treatment was to improve smile esthetics with clear aligner treatment.
Pre-treatment facial photographs showed balanced facial proportions. A functional exam documented lip incompetence with hyperactive mentalis muscles to achieve lip closure [Figure 1]. The analysis of the pre-treatment diagnostic records revealed Class I molar and Class II canine relationships bilaterally [Figure 1]. Bimaxillary protrusion with an 5 mm overjet and 2 mm overbite was associated with ~3 mm of crowding in the upper arch, and an anterior Bolton ratio of 75.9%. The maxillary and mandibular midlines were deviated by 0.5 mm and 1.5 mm to the right, respectively. The panoramic radiograph showed four unerupted third molars, and cephalometric analysis revealed a normal skeletal relationship with flared incisors [Figure 2 and Table 1]. The American Board of Orthodontic discrepancy index (DI) was 21 as shown in the subsequent Worksheet 1.

- Pre-treatment extraoral and intraoral photographs.

- Pre-treatment panoramic radiograph (left) and lateral cephalometric radiograph (right).
| Cephalometric summary | |||
|---|---|---|---|
| Skeletal analysis | Pre-tx | Post-tx | Diff. |
| SNA° (82°) | 83.5° | 83.5° | 0° |
| SNB° (80°) | 80.5° | 81.5° | 1° |
| ANB° (2°) | 3° | 2° | 1° |
| SN-MP° (32°) | 27.5° | 26.5° | 1° |
| FMA° (25°) | 20.5° | 19.5° | 1° |
| Dental analysis | |||
| U1 TO NA mm (4 mm) | 10 | 3.5 | 6.5 |
| U1 TO SN° (104°) | 118° | 107° | 11° |
| L1 TO NB mm (4 mm) | 9.5 | 4 | 5.5 |
| L1 TO MP° (90°) | 115° | 96° | 19° |
| Facial analysis | |||
| E-LINE UL (‒1 mm) | 1 | ‒2 | 3 |
| E-LINE LL (0 mm) | 3 | ‒2 | 5 |
| %FH: Na-ANS-Gn (53%) | 56% | 55% | 1% |
| Convexity: G-Sn-Pg’ (13°) | 15° | 11° | 4° |
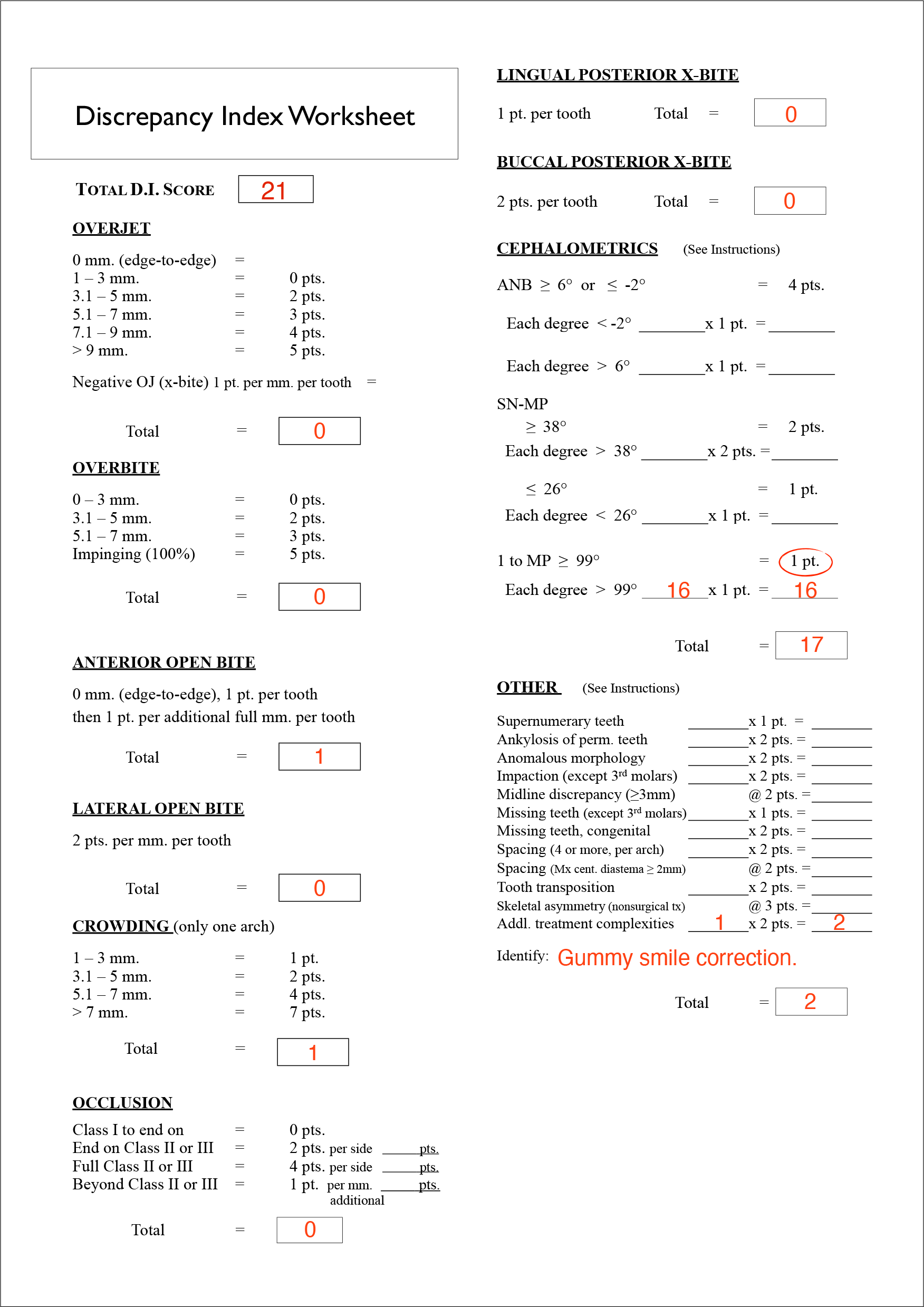
- Discrepancy Index (DI).
TREATMENT OBJECTIVES
The treatment objectives were to: (1) Reduce dental protrusion by improving lip profile; (2) achieve normal overjet and overbite; (3) maintain a bilateral Class I molar relationship; (4) obtain a bilateral Class I canine relationship; (5) coordinate midlines; and (6) align arches.
TREATMENT ALTERNATIVES
The focus of Invisalign® aligner treatment was correction of the lip protrusion and gummy smile [Figure 3]. A non- extraction treatment approach was considered: arch retraction of 3 mm in every quadrant, interproximal reduction (IPR) to relieve crowding, and rounding out the arch form.[17] Extraction of all the third molars was discussed because it would aid with arch retraction, but the patient declined the projected result for non-extraction treatment because it failed to adequately reduce dental protrusion and mentalis strain. The alternative treatment option was extraction of four first premolars, followed by Invisalign® treatment supplemented with OBS anchorage to retract and intrude the incisors. The patient accepted the extraction treatment plan which involved: (1) Two 2 mm × 12 mm OBSs installed bilaterally in the infra-zygomatic crest (IZC), (2) two additional 1.5 mm × 8 mm Incisal OBSs in the maxillary anterior inter-radicular (I-R) region between central and lateral incisors bilaterally, (3) elastics (Ormco Corporation, Brea, CA) hooked on the bone screws to retract and intrude the maxillary anterior segment, and (4) IPR to address a Bolton discrepancy between the arches.

- Pre-treatment extraoral photographs revealed patient’s gummy smile tendency. Note that the width of exposed gingiva is 4 mm superior to the U2s.
TREATMENT PROGRESS
iTero Element® intraoral scans (Align Technology, Inc., San Jose, CA, USA) provided a 3D dataset.[18] The ClinCheck® (Align Technology, Inc., San Jose, CA, USA) system was used to plan the treatment and project the outcome. Both optimized and conventional attachments were applied in sequential staging [Figure 4]. The treatment was conducted in two phases: initial and refinement. Oral hygiene and aligner fit were monitored at monthly intervals.
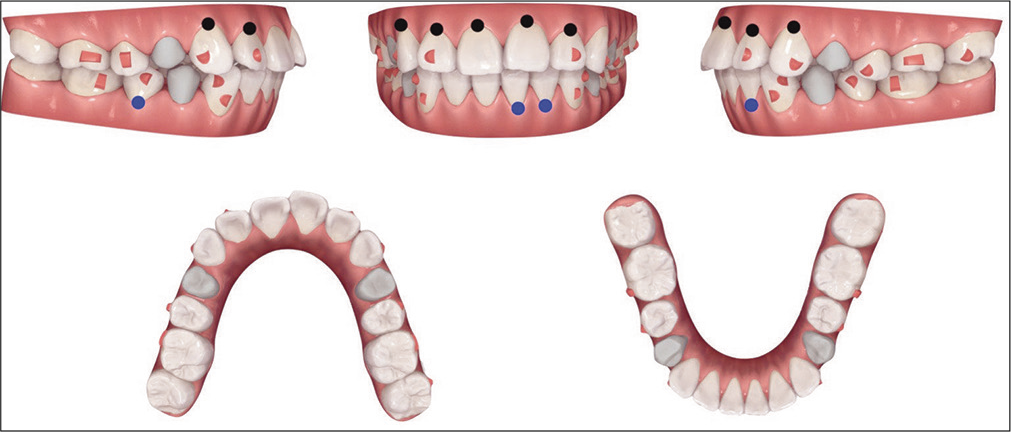
- ClinCheck® treatment plan and prescribed attachments are shown for the initial phase of treatment. Blue dots indicate variably predictable tooth movement (2.5–3 mm intrusion for lower incisors; 4–6 mm root movement for LR5). Black dots indicate less predictable tooth movement (>3 mm intrusion for upper incisors; >6 mm root movement for UR3).
INITIAL PHASE
The major goals of the initial treatment were to retract and the anterior segments as the arches were intruded [Figure 5]. A total of 45 sets of aligners were used over 13 months. According to the clinician’s instructions, the first set of 38 aligners was changed every 10 days, and then every 7 days for the last seven aligners. Optimized root control attachments were used on canines in combination with precision cuts. Optimized anchorage attachments were provided for the posterior teeth [Figure 6]. Half pontics were used for esthetic replacement of missing teeth. SmartStage® technology was used for the upper incisors to minimize unwanted tipping and anterior extrusion.[12]
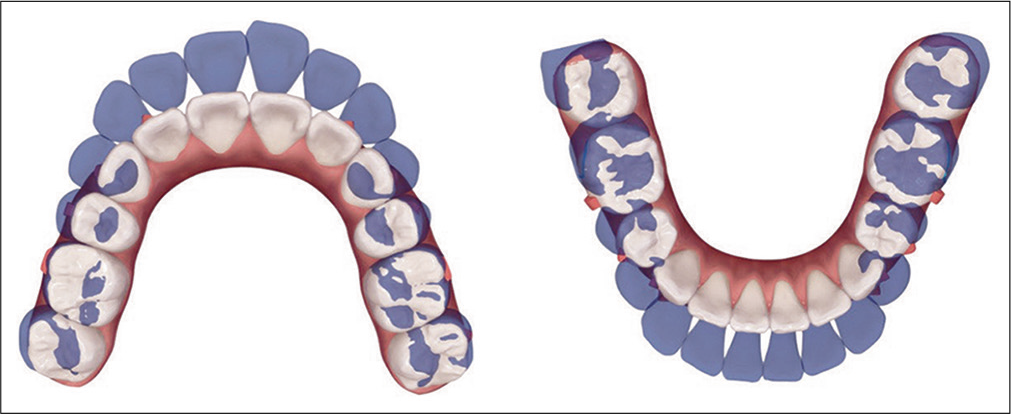
- ClinCheck® initial phase treatment is projected by superimposition (blue: original tooth position; white: simulation of final tooth position) on dental landmarks that are programmed to be stable. Maximum anchorage is planned in the upper arch, consistent with more moderate anchorage for the lower arch. The anchorage requirements in both arches are quite challenging, and require TAD anchorage.
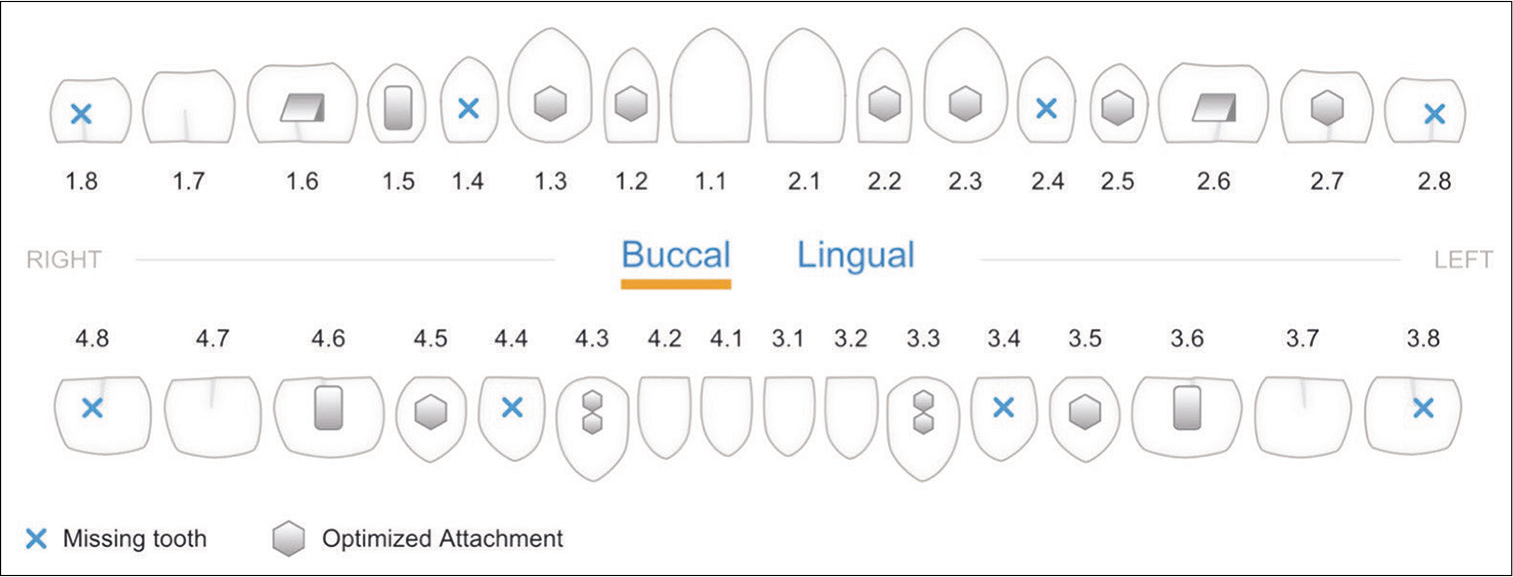
- The initial phase of Invisalign® treatment utilizes SmartForce® features (optimized attachments in hexagon) for the Invisalign G6 solution to provide maximal posterior anchorage for distal translation of canines.
Anterior and IZC OBSs were placed when the tenth aligner was delivered. Elastics (3.5oz) were worn full- time from the U3s to the IZC OBS and from the anterior segment of the aligner to the Incisal OBSs bilaterally [Figure 7]. Inwardly-inclined cuts were made chair side with dedicated cutting pliers for every aligner, and all elastics were preloaded. The patient was trained to hook the elastics intraorally from the aligner cuts to the OBSs. An overlapping two-elastic design in the maxillary anterior avoided irritating the labial frenum. OBS anchorage was essential for achieving the ClinCheck® simulations during treatment with the initial series of aligners [Figure 8]. The outcome at the conclusion of the initial phase of treatment was dependent on bone screw anchorage [Figure 9].
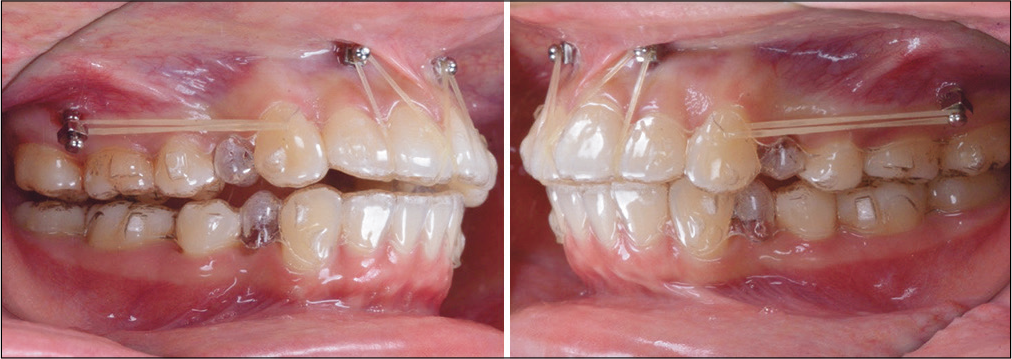
- Intraoral photographs show the mechanics after OrthoBoneScrew® placement and the application of 3.5oz elastics for retraction of buccal segments and intrusion of the maxillary anterior segment.
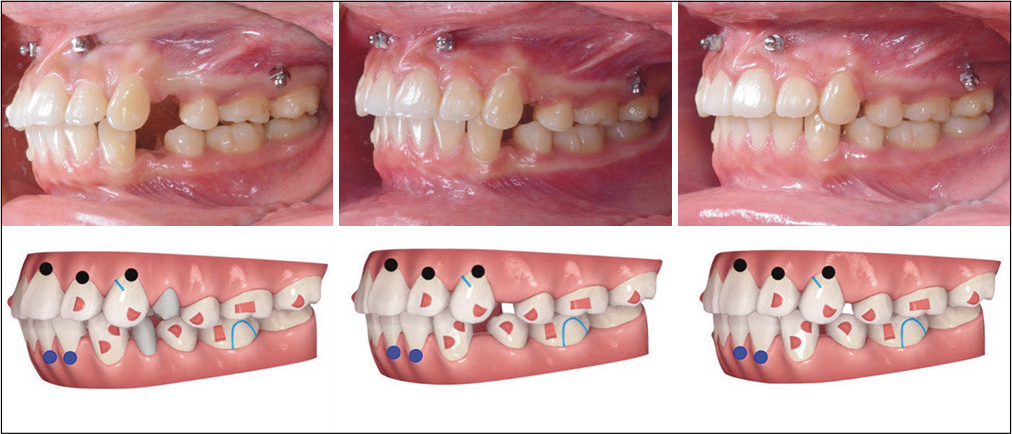
- A progressive series of left buccal intraoral photographs show the progress of treatment compared to ClinCheck® simulations: Left 3 months, 10/45 aligners; center 6 months, 21/45 aligners; right 10 months, 32/45 aligners. Note a modified G6 attachment is specified for the UL3 to accommodate a precision cut for an elastic anchored by the IZC OBS. For the colored markings in the simulations, see Figure 4 for details.

- Extraoral and intraoral photographs show the outcome for the initial phase of aligner treatment. A canine Class II window (interocclusal space) distal to the UR3 cusp is noted.
REFINEMENT PHASE
Refinement (finishing) with 20 additional aligners was conducted to correct the Class II relationship on the right side by retracting the UR quadrant 1 mm [Figure 10]. After all extraction spaces were closed, IPR was carried out to reduce black triangles and address the Bolton discrepancy [Figure 11]. In the finishing stage, the heavy occlusal contacts on posterior teeth were reduced. Subsequently, conventional attachments replaced the optimized attachments to provide predictable retention. Precision cuts were again prescribed for the finishing mechanics and retention. The patient continued to use all elastics bilaterally as prescribed.
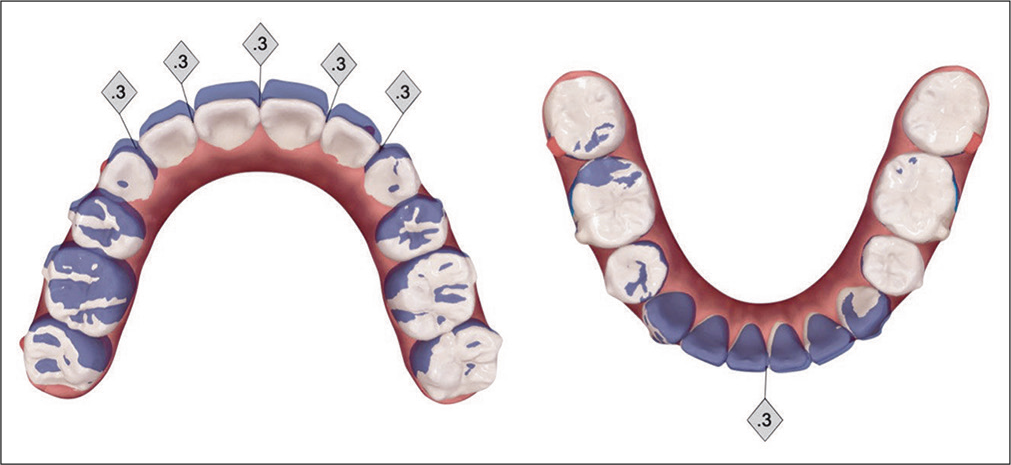
- Refinement phase of treatment is programmed into ClinCheck® to retract the UR quadrant 1 mm (blue: original tooth position; white: simulation of final tooth position). IPR of 0.3 mm is planned for five sites in the maxillary anterior segment, but for only one site in the lower arch, to correct a perceived Bolton discrepancy.

- Post-treatment extraoral and intraoral photographs. Gingivoplasty as well as labial frenectomy were performed with diode laser at the completion of the treatment. Note the buccal segments are slightly Class II, but there is no overjet suggesting than more refinement of IPR was indicated in programming the refinement stage on ClinCheck®.
RETENTION
Essix (Dentsply Sirona, Harrisburg PA) retainers were delivered for both arches. The patient was instructed to wear them full time for the first 6 months post-treatment and nights only thereafter. Instructions were provided for home care, as well as for maintenance of the retainers.
TREATMENT RESULTS
This case report describes the correction of a malocclusion with a DI of 21, which was treated to an excellent CRE of 10 and a P&W esthetic score of 3, as shown in the subsequent worksheets (Worksheets 2 and 3). The total treatment duration was 18 months with a total of 65 aligners (45 + 20). Post- treatment records document achievement of all treatment objectives relative to good dental alignment and dentofacial esthetics [Figure 11]. Ideal overbite and overjet were achieved. Most importantly, all extraction spaces were closed with good maintenance of root parallelism (axil inclination) [Figure 12]. Upper and lower incisors were retracted and uprighted, improving the patient’s lip profile and facial esthetics [Table 1 and Figure 13]. The intrusion of the entire maxillary dentition corrected the gummy smile, and produced a slight counterclockwise rotation of the mandible to close the vertical dimension of occlusion. Buccal segments were corrected to Class I bilaterally. Upper and lower midlines were coincident with the facial midline. The patient was highly motivated and compliant with aligner wear and elastics. She was extremely happy with the treatment results. Overall, a near ideal outcome was achieved. Arrangements will be made in the future for third molar extractions.
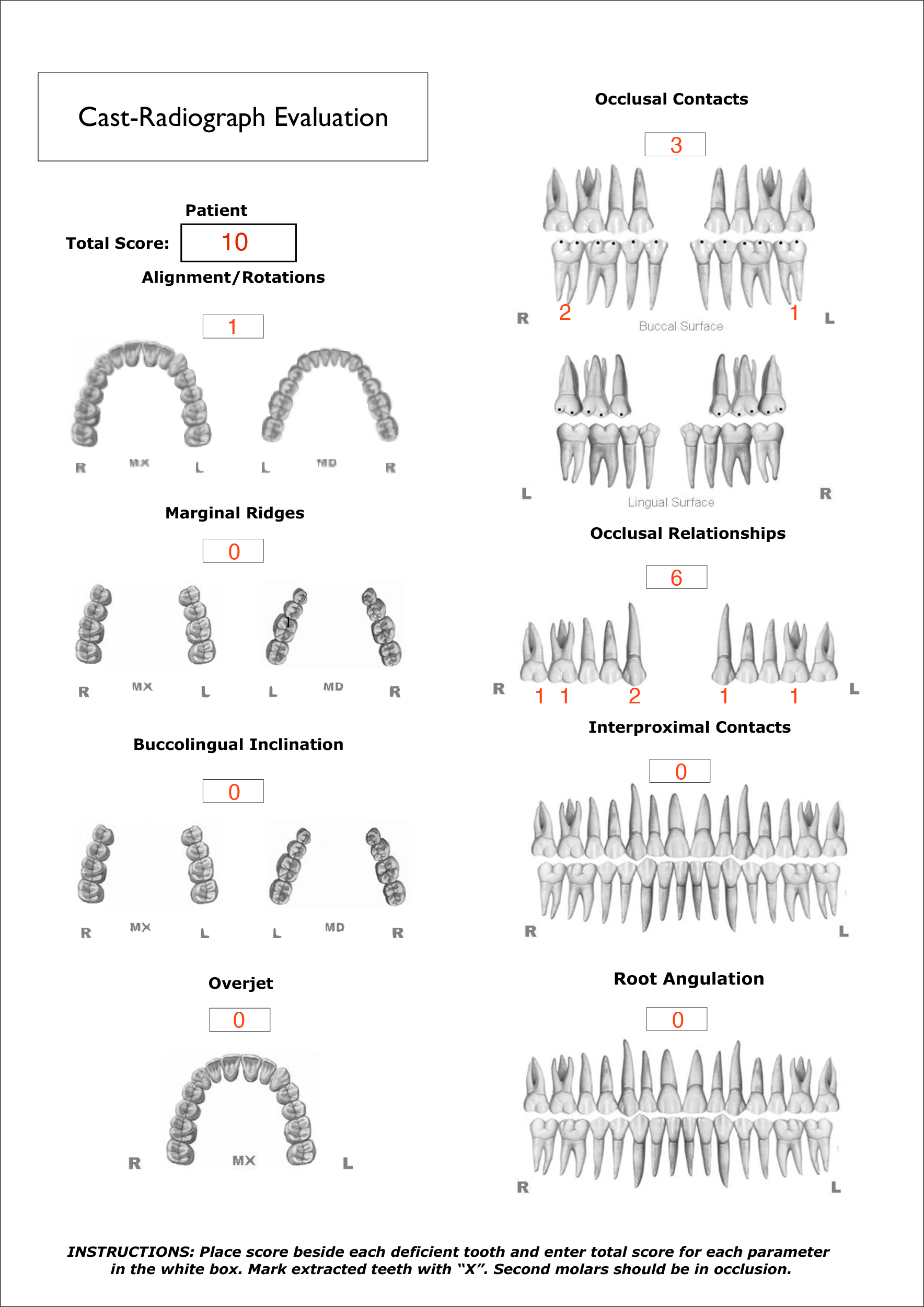
- Cast-Radiograph Evaluation (CRE).
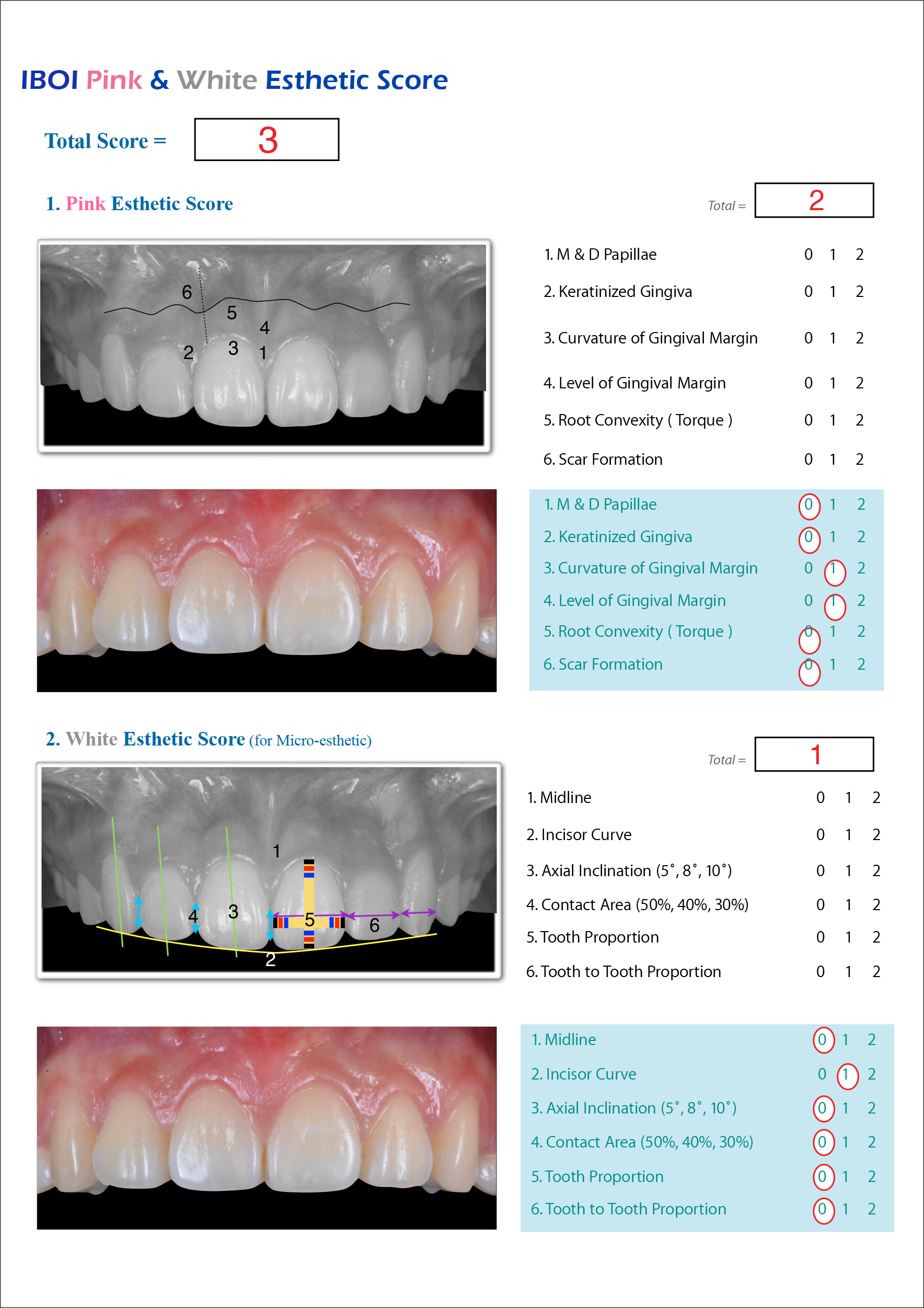
- Pink & White Esthetic Score (P&W)
![Post-treatment panoramic radiograph (left) and lateral cephalometric radiograph (right). Good root parallelism is noted in the maxillary buccal segments, but all the teeth are more upright than normal [Figure 3] which contributes to the Class II windows distal to the cusps of the U3s [Figure 11].](/content/9/2020/10/2/img/APOS-10-120-g012.png)
- Post-treatment panoramic radiograph (left) and lateral cephalometric radiograph (right). Good root parallelism is noted in the maxillary buccal segments, but all the teeth are more upright than normal [Figure 3] which contributes to the Class II windows distal to the cusps of the U3s [Figure 11].
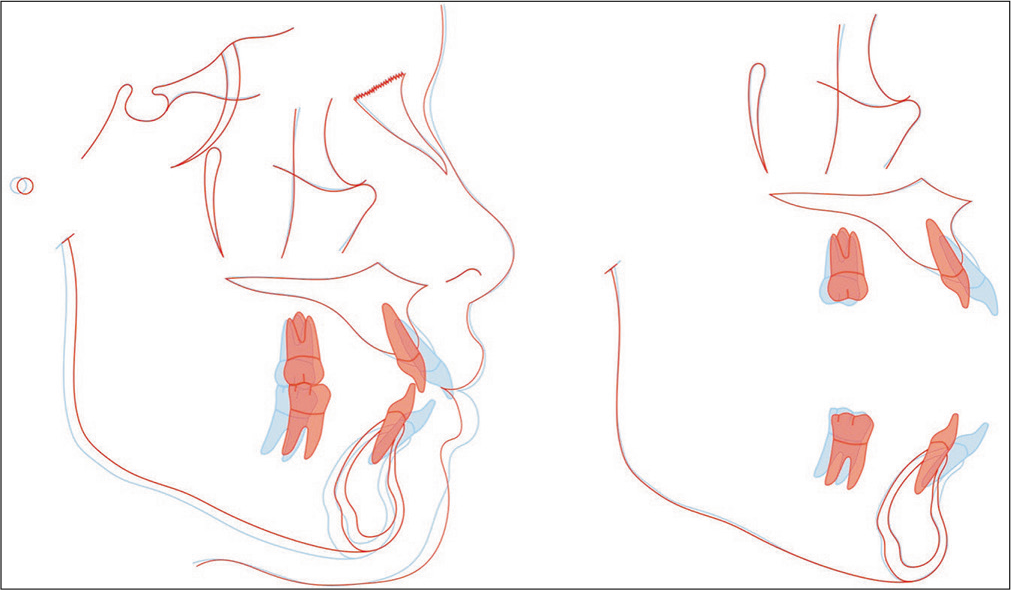
- Superimposed tracings of the pre-treatment (blue) and post-treatment (red) lateral cephalometric radiographs show that bimaxillary protrusion was resolved dramatically (U1 and L1 retracted 6.5 and 5.5 mm, respectively). The intrusion of entire upper dentition (U1 and U6 intruded 2.2 and 1.5 mm, respectively) was consistent with the counterclockwise rotation of the mandible.
DISCUSSION
Extraction of four first premolars is often indicated for Asians to correct typically Class I malocclusions with bimaxillary protrusion with or without crowding.[19,20] Initial crowding may contribute to anchorage loss with fixed appliances[21] and aligners.[14] However, with the current Invisalign® approach, crowding is directly related to predictable tooth movement with aligners. Thus, the overall tooth movement, as well as mesial tipping and translation of first molars, is close to the pretreatment prediction.[14] Because the current patient had minimal crowding but severe protrusion, firm posterior anchorage (OBSs) was indicated.
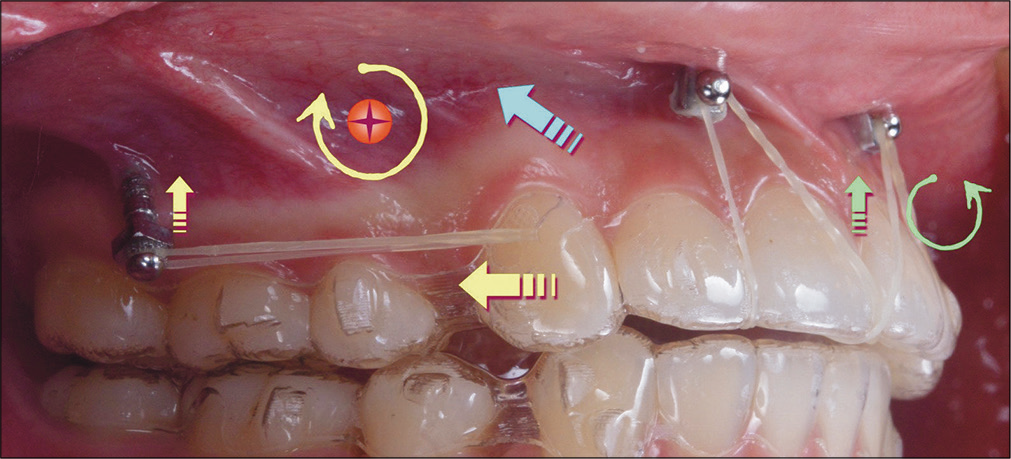
- The force system is diagrammed in 2D to explain the mechanics in the sagittal plane for an infra-zygomatic crest (IZC) and Incisal OrthoBoneScrews®. Based on the presumed center of resistance (CR, red circle with a cross) for the maxillary arch, the elastic force from the IZC screws to the cuspid precision cut has both distal and vertical components (straight yellow arrows) that produce a clockwise moment around the CR (curved yellow arrow). The anterior inter-radicular screws anchor an intrusive force (green arrow) that creates a counterclockwise moment (curved green arrow) tending to flare the maxillary incisors. The presumed resultant for overall applied loads is the blue arrow.

- The application of anterior inter-radicular screws to anchor elastics fitted into palatal cuts (blue curved lines) in the aligners is shown in the occlusal view (left) and the frontal view (right). The palatal cuts inclined to the mesial are good attachments for elastics attached the Incisal OrthoBoneScrews® bilaterally.
The ideal soft-tissue display when smiling is 1–2 mm of attached gingiva.[22] While orthodontists rate 2–3 mm of gingival exposure as unattractive, general dentists, and laypeople feel that >4 mm is required to rate a smile as unattractive [Figure 3].[23,24] A “gummy smile” may have both extra-oral and intra-oral dimensions.[25] The differential diagnosis for the current patient favored a dental origin because the morphology was not consistent with anterior dentoalveolar extrusion nor vertical maxillary excess. The patient’s lips were incompetent at rest, but did contact with hypermentalis activity, so it was important to control the vertical dimension of occlusion [Figure 1]. The use of the maxillary anterior mini-screws was originally proposed by Lin et al.[26]
Extraction cases with gummy smile are recognized as challenging malocclusions for clear aligner treatment.[1-3,9] Ideal ClinCheck® simulations are difficult to achieve. The “bowing” and/or “bite block” effect(s)[27] may enhance the gummy smile tendency or deepend the bite with conventional aligners, so mini-screws play a key role in expanding the scope for clear aligner treatment.[28] As shown in [Figure 14], an extra-alveolar (E-A) retracting force on the dentition anchored with IZC OBSs produced a favorable clockwise moment to deepen the plane of occlusion, but the position of the center of rotation (Crot) in 3D was unknown. The Crot for posterior rotation of the lower arch with mandibular buccal shelf OBS is actually an axis of rotation in 3D that has been calculated with finite element analysis (FEA) of cone-beam commuted tomography (CBCT) images.[29] The calculated Crot was far more anterior and occlusal than the previous 2D estimates. If the calculated Crot is similar for IZC anchorage in the upper arch, E-A posterior anchorage has less of an effect on steepening the maxillary plane of occlusion to produce incisor extrusion than is implied in 2D [Figure 14]. The scientific evolution of IZC OBS anchorage for aligner therapy requires 3D assessment of the Crot because a relatively simple change in the direction of the elastics force may eliminate the need for Incisal OBSs. Steepening the plane of the buccal elastic by screwing the OBS deeper into the buccal fold and attaching the elastic near the cusp tip of the canine may eliminate the need for the uncomfortable and unattractive Incisal mini-screws. Patients desiring aligner treatment prefer the most esthetic and least invasive approach, so eliminating Incisal mini-screws would be a very attractive option.
Realistic assessment of the 3D biomechanics relative to IZC anchorage for aligner treatment is not possible without FEA of CBCT images.[29] However, in the meantime 2D analysis is helpful for routine clinical applications [Figure 14]. When the buccal elastic force is parallel to the occlusal plane, clockwise rotation of the occlusal plane is expected to extrude the incisors. I-R OBSs in the incisal anchorage position between the central and lateral incisor roots are essential for reversing the extrusive component on the anterior segment. In addition, the anterior vertical force results in a slight flattening of the occlusal plane and net intrusion of the maxillary arch [Figure 15]. The combination of all four OBS fixtures (2 IZC and 2 Incisal) retracted and intruded the maxillary incisors [Figure 13]. In addition, the roots in the buccal segments were well aligned (parallel) at the end of treatment, but they were perpendicular to the occlusal plane rather than distally oriented [Figure 2]. One can view the impressive results [Figures 11-13] as achieving the full potential of aligners, but more properly OBS anchorage expanded the scope of aligner treatment.[30] However, there is room for improvement particularly in regard to root angulations in the maxillary posterior segments.
[Figure 15] demonstrates the application of anterior I-R bone screws with elastics attached to “inwardly inclined” cuts on the palatal surface of the central incisors. The cuts are made chairside for every aligner specified with a special cutting plier. The patient fits elastics into the slots before seating the aligner on the arch, and then stretches the elastics over the Incisal bone screws with finger pressure [Figure 15].
The overall failure rates for anterior I-R screws and IZC E-A screws are 7.2%[31] and 6.3%,[32] respectively. The failure rates for TADs anchoring aligners are unknown, but the hypothesis is the failure rate which will be lower because the applied force is lower and it is not applied full time. Further study is required to resolve this important issue.
All treatment objectives were met. Despite the patient’s compliance in wearing aligners and elastics, there was Class II “window” along the distal incline of the incisal edge of both maxillary canines which extended posteriorly for all the interproximal intercuspation in the buccal segment [Figure 11]. This problem could be more clearly assessed with articulated casts. There were several contributing factors for the occlusal irregularities: (1) slight Class II relationship of the U3s and U4s, (2) inadequate distal moment of the U3 roots, and (3) insufficient extrusion of the L4s. In retrospect, closer monitoring of the ClinCheck® setup to resolve the Class II buccal segments may have indicated less IPR in the maxillary anterior region [Figure 10] and more IPR of the lower anterior segment to create additional overjet to accommodate the Class II correction. In addition, distal root movement for all teeth in the maxillary buccal segments was needed. The roots were parallel [Figure 12] but they were too upright to achieve an ideal intercuspation relationship. Overall, the result was excellent (CRE 10), but there was potential for a more ideal outcome.
The compensatory mechanism in the setups for Invisalign® extraction cases with mini-screw anchorage is similar to treating gummy smile cases. Four screws can prevent unattractive bowing effects, and at the same time save dozens of additional aligners. Once realistic 3D biomechanics are calculated,[29] it will be possible to further refine aligner alignment with TAD anchorage to achieve even more ideal results. The goal is to be competitive with the high accuracy for non-extraction aligner treatment.[33]
CONCLUSIONS
Closure of extraction spaces with Invisalign® appliances alone can be challenging and frustrating. Clinicians should be prepared for anterior dumping and posterior torque loss. Prevention is better than cure. Aligners can be well integrated with TAD anchorage to execute a broad range of malocclusion corrections. Despite the excellent outcome for the current case, the treatment details should be carefully interpreted. 3D studies of the biomechanics are needed to formulate robust clinical recommendations.
Acknowledgments
The authors would like to thank Mr. Paul Head for proofreading this article.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The treatment effects of Invisalign orthodontic aligners: A systematic review. J Am Dent Assoc. 2005;136:1724-9.
- [CrossRef] [PubMed] [Google Scholar]
- How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;35:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- Efficiency, effectiveness and treatment stability of clear aligners: A systematic review and meta-analysis. Orthod Craniofac Res. 2017;20:127-33.
- [CrossRef] [PubMed] [Google Scholar]
- The invisalign? appliance today: A thinking person's orthodontic appliance. Semin Orthod. 2017;23:12-64.
- [CrossRef] [Google Scholar]
- A systematic review of the accuracy and efficiency of dental movements with invisalign? Korean J Orthod. 2019;49:140-9.
- [CrossRef] [PubMed] [Google Scholar]
- Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: Premolar extraction patients. Am J Orthod Dentofacial Orthop. 2008;133:837-45.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical effectiveness of invisalign? orthodontic treatment: A systematic review. Prog Orthod. 2018;19:37-60.
- [CrossRef] [PubMed] [Google Scholar]
- Align Technology. Invisalign G6. Available from: http://www.invisalign-g6.com/en-xa [Last accessed on 2020 Mar 16]
- [Google Scholar]
- Design of the Invisalign system performance. Semin Orthod. 2017;23:3-11.
- [CrossRef] [Google Scholar]
- Introduction to Invisalign? smart technology: Attachment design and re-call checks. J Digit Orthod. 2019;54:80-95.
- [Google Scholar]
- Treating bimaxillary protrusion and crowding with the Invisalign G6 first premolar extraction solution and Invisalign aligners. APOS Trends Orthod. 2018;8:219-24.
- [CrossRef] [Google Scholar]
- Comparison of achieved and predicted tooth movement of maxillary first molars and central incisors: First premolar extraction treatment with Invisalign. Angle Orthod. 2019;89:679-87.
- [CrossRef] [PubMed] [Google Scholar]
- Torque expression in stainless steel orthodontic brackets. A systematic review. Angle Orthod. 2010;80:201-10.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015;85:881-9.
- [CrossRef] [PubMed] [Google Scholar]
- The predictability of transverse changes with Invisalign. Angle Orthod. 2017;87:19-24.
- [CrossRef] [PubMed] [Google Scholar]
- Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am J Orthod Dentofacial Orthop. 2013;144:471-8.
- [CrossRef] [PubMed] [Google Scholar]
- Extraction decision and identification of treatment predictors in Class I malocclusions. Prog Orthod. 2013;14:47-54.
- [CrossRef] [PubMed] [Google Scholar]
- Current status of orthodontic professionals in the Asian pacific region. APOS Trends Orthod. 2016;6:58-77.
- [CrossRef] [Google Scholar]
- Excessive gingival display-etiology, diagnosis, and treatment modalities. Quintessence Int. 2009;40:809-18.
- [Google Scholar]
- Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11:311-24.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of dental professionals and laypersons to altered dental esthetics: Asymmetric and symmetric situations. Am J Orthod Dentofacial Orthop. 2006;130:141-51.
- [CrossRef] [PubMed] [Google Scholar]
- Checklist of esthetic features to consider in diagnosing and treating excessive gingival display (gummy smile) Dental Press J Orthod. 2011;16:131-57.
- [CrossRef] [Google Scholar]
- Simultaneous reduction in vertical dimension and gummy smile using miniscrew anchorage. J Clin Orthod. 2010;44:157-70.
- [Google Scholar]
- Cephalometric comparison of adult anterior open bite treatment using clear aligners and fixed appliances. Angle Orthod. 2019;89:3-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extra-alveolar bone screws for conservative correction of severe malocclusion without extractions or orthognathic surgery. Curr Osteoporos Rep. 2018;16:387-94.
- [CrossRef] [PubMed] [Google Scholar]
- Biology of biomechanics: Finite element analysis of a statically determinate system to rotate the occlusal plane for correction of a skeletal Class III open-bite malocclusion. Am J Orthod Dentofacial Orthop. 2015;148:943-55.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanics and clinical significance for mini-screws in four bicuspid extraction aligner cases. J Digit Orthod. 2020;58:94-8.
- [Google Scholar]
- Failure rates for SS and Ti-alloy Incisal anchorage screws: Single-center, double-blind, randomized clinical trial. J Digit Orthod. 2018;52:70-9.
- [Google Scholar]
- Comparison of the failure rate for infra-zygomatic bone screws placed in movable mucosa or attached gingiva. Int J Orthod Implantol. 2017;47:96-106.
- [Google Scholar]
- How accurate is Invisalign in nonextraction cases? Are predicted tooth positions achieved? Angle Orthod. 2017;87:809-15.
- [CrossRef] [PubMed] [Google Scholar]






