Translate this page into:
Clinical effect of low-level laser therapy on pain perception after placement of initial orthodontic archwires

*Corresponding author: Youssef Sedky, Department of Orthodontics, Misr International University, Cairo, Egypt. youssef.sedky@miuegypt.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: El Shahawy R, Sameeh HM, Sedky Y, El Nagar WR. Clinical effect of low-level laser therapy on pain perception after placement of initial orthodontic archwires. APOS Trends Orthod. 2025;15:158-65. doi: 10.25259/APOS_33_2024
Abstract
Objectives:
This study evaluated the clinical effect of low-level laser therapy (LLLT) on pain perception after placement of initial orthodontic archwires.
Material and Methods:
Forty-eight orthodontic patients were selected and randomly divided according to exposure to LLLT into two equal groups: Group 1 (Control group) Included 24 patients who were not subjected to any laser therapy, and Group 2 (Laser group), Included 24 patients who were subjected to LLLT. Pain perception was investigated for all patients after 6 h, 2nd day, 3rd day, and 7th day through a visual analog scale (VAS) with 0 indicating no pain and 10 indicating intolerable pain. All data were collected, tabulated, and statistically analyzed.
Results:
There was a statistically significant difference between the laser group and the control group. According to VAS readings, the laser group showed lower means of pain scores than the control group .
Conclusion:
From the present study, the following could be concluded: (1) Diode laser using 940 nm wavelength with the used parameters showed positive results in reducing pain severity in the early stages of orthodontic treatment. (2) LLLT can have better biomodulating outcomes in promoting long-lasting analgesic action during the period of greatest pain sensitivity.
Keywords
Initial orthodontic archwires
Pain perception
Diode laser
Low-level laser therapy
INTRODUCTION
Clinicians and patients are both very concerned about any pain or discomfort experienced during orthodontic treatment. It may discourage patients from starting or continuing treatment. Orthodontic pain often starts to manifest hours after the force is applied, peaking at 12–36 h, and then gradually decreases to the baseline value within 7 days.[1] Pain is induced as a result of compression pressures that result in ischemia, inflammation, and edema in the periodontal tissues, which occur particularly in the early phases during correction of malocclusion, which, in turn, restrains masticatory function.[2] It has been demonstrated the influence of fixed orthodontic treatment on dietary intake and behavior in adolescent patients is that a majority of patients prefer a soft diet due to the pain that they experience; this situation can be so disturbing that patients have to take medication.[3]
As a non-pharmacological method, low-level laser therapy (LLLT) has recently been used; it has analgesic properties and anti-inflammatory effects by increasing the local blood flow by reducing prostaglandin levels E2 and inhibiting of release of cycloxygenase-2 and the arachidonic acid; also, it induces the release of an endogenous opioid neuropeptide (beta-endorphin) that produces potent analgesic effects. Some researchers have pointed out that the use of LLLT reduced the risk of incidence of pain compared to other conventional methods. However, standardization of the type and use of LLLT needs to be established, and thus, clinical results and efficacy of LLLT in reducing orthodontic pain are directly related to the type of laser, wavelength, energy density (J/cm2), time of application per point, and frequency. The energy output of LLLT is low enough so as not to raise the temperature of the treated tissues above 36.5°C or normal body temperature.[4-6]
In the field of orthodontics, researchers hypothesized that LLLT would be beneficial for controlling orthodontic pain and promoting bone deposition in the midpalatal suture during rapid maxillary expansion.[7]
From the introduction mentioned above, it can be seen that not enough studies have evaluated the effect of LLLT using a 940 nm wavelength on decreasing pain perception after placing the initial orthodontic archwire. Therefore, the present study will be conducted with LLLT using a 940 nm wavelength.
MATERIAL AND METHODS
Sample size calculation
Based on previously treated trial cases[8] (The mean pressure pain threshold), we conducted a power analysis (G power version 3.1 statistical software, Franz Faul, Universität Kiel Germany). An a priori analysis was performed to compute the required sample size given α, power, and effect size. The input parameters were α error probability of 0.05, an effect size of 0.74, a power of 0.80, and a number of groups was 2. The findings indicated a minimum sample size of n = 48 patients (24 patients for each group).
Study design and settings
After the approval of the Research Ethical Committee (REC) of the Faculty of Dentistry Suez Canal University, with approval no. #460/2022, this randomized controlled clinical trial study was carried out on 48 patients aged 18–30. The patients were selected from orthodontic patients receiving treatment in the outpatient clinics of the Faculty of Dentistry, Suez Canal University.
Sample selection
Criteria of patient selection
Inclusion criteria
Patients included in this study were between 18 and 30 years old, both genders were included, and had 5–7 mm maxillary crowding (class I crowding).
Exclusion criteria
Medically compromised patients, chronic use of analgesic drugs, poor oral hygiene, and using trans palatal arch, mini-screw, and headgear as a component of treatment were excluded from the study.
Allocation and randomization
Computer-generated randomization for the sequence was held at the 1st visit. Randomization was performed through computer software (www.randomizer. org [Copyright© 1997– 2021 by Geoffery C. Urbaniak and Scott Plous]).
The number corresponding to each treatment procedure was recorded on cards kept inside sequentially numbered, opaque, and sealed envelopes.
Blinding
This trial was single-blinded, as only the outcome assessors were blinded. The participants and principal investigator were not blinded due to the use of an obviously different method: LLLT.
Sample grouping
All patients were randomly divided into two equal groups:
Group 1 (control): Included 24 patients who were subjected to routine orthodontic treatment without application of any laser therapy
Group 2: Included 24 patients who were subjected to LLLT after orthodontic treatment.
General orthodontic procedures
Each patient was assessed for eligibility, the procedures were explained, and the consent form was signed.
Bonding procedure
Etching of enamel was performed using 35% phosphoric acid gel (Grengloo Etching solution, Ormco Corporation, California, USA) for 15 s, rinsed for 15 s with water, and gently air dried with water-free/oil-free air for 5 s. A single layer of universal adhesive (Ortho solo Bond Enhancing primer, Ormco Corporation, California, USA) was applied using a disposable applicator brush and was rubbed for 20 s. Solvent dryness and air thinning were achieved by a gentle stream of air over the adhesive for about 5 s until it no longer moved and the solvent had evaporated completely, then light-cured using light-emitting diodes light curing unit (Elipar™ S10, 3M ESPE, USA) according to the manufacturer’s instructions.
A pre-adjusted edgewise appliance with slot dimensions of 0.022 × 0.025 inches and Roth prescription (Aria Ortho Organizers® Inc.) was placed on the maxillary arch from the left first molar to the right first molar and bonded using resin composite (Grengloo, Ormco Corporation, California, USA) to the treated enamel surfaces following the manufacturer’s instructions.
A 0.014-inch round nickel-titanium archwire (Ortho Organizers® Inc.) was fully engaged with elastomeric ties and cut at the end of the first molar tube.
Intervention application
Group 1 (control): There was no additional implementation in the control group aside from the routine orthodontic procedure.
Group 2: LLLT application was carried out immediately after placement of the fixed orthodontic appliances. An InGaAsP diode laser with a wavelength of 940 nm (Epic X™; Biolase company, USA) was used, as shown in [Figure 1]. It was irradiated perpendicular to the upper arch, which was divided into three quadrants from right first molar to right first premolar and from right canine to left canine and from left first premolar to left first molar; then, application was performed on buccal mucosa covering the root, using bleaching hand piece as shown in [Figure 2] with power output 100 mW, spot size 2.8 cm2 (35 × 8 mm), energy 13.5J, energy density 4.8 J/cm2, and mode of operation is continuous mode with duration 135 s per quadrant in a contact mode.[9]
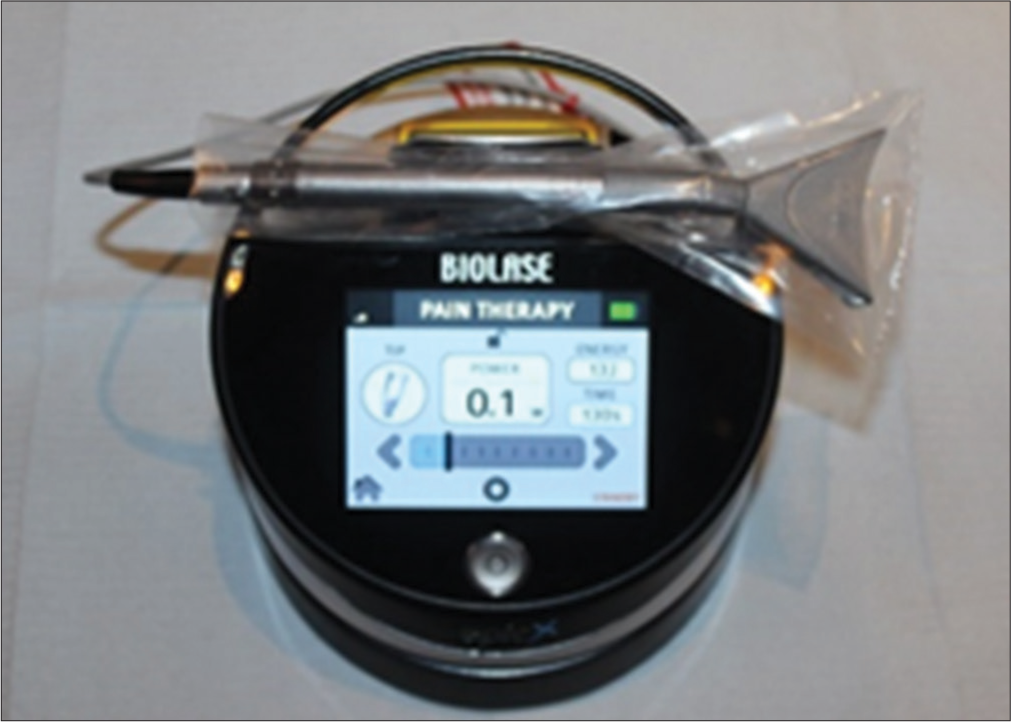
- Diode laser Epic X™.

- Diode laser application using bleaching handpiece.
Post-operative instructions and follow-up
Patients received post-operative instructions and oral hygiene guidelines that should be followed and were asked to refrain from taking analgesics.
Pain perception evaluation
On completing the intervention, pain perception was measured using a 10-cm visual analog scale (VAS). Participants were instructed to complete a VAS diary containing 4 forms for 4 different times: 6th h, 2nd day, 3rd day, and 7th day after starting the fixed orthodontic treatment, with 0 indicating no pain and 10 indicating intolerable pain.
Statistical analysis
All pain perception data were collected, tabulated, checked for normality, and statistically analyzed to evaluate the performance of LLLT using a Diode laser after placement of initial archwires during orthodontic treatment.
Statistical analysis was performed using the computer program SPSS software for Windows version 26.0 (the Statistical Package for the Social Sciences, Armonk, NY: IBM Corp) at P < 0.5.
Descriptive data: Descriptive statistics will be calculated in the form of mean ± standard deviation, range (Max-Min), median, and coefficient of variance (C. V%).
Independent T-test or Mann–Whitney (U) test (according to types of data) will be used for pair-wise comparisons (groups A and B). The significance level will be set at P ≤ 0.05.
RESULTS
Laser group
The results in [Table 1 and Figure 3] showed that there is a statistically significant difference between the pain rating scale with different times using the chi-square test at P < 0.005 (χ2 = 48.34, P ≤ 0.0001).
| Pain rating scale | 1st day | 2nd day | 3rd day | 7th day | Chi-square | -value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| 0 | 10 | 41.7 | 12 | 50.0 | 24 | 100.0 | 24 | 100.0 | 48.34 | <0.0001** | |
| 1 | 8 | 33.3 | 6 | 25.0 | |||||||
| 2 | 2 | 8.3 | 6 | 25.0 | |||||||
| 3 | 4 | 16.7 | |||||||||
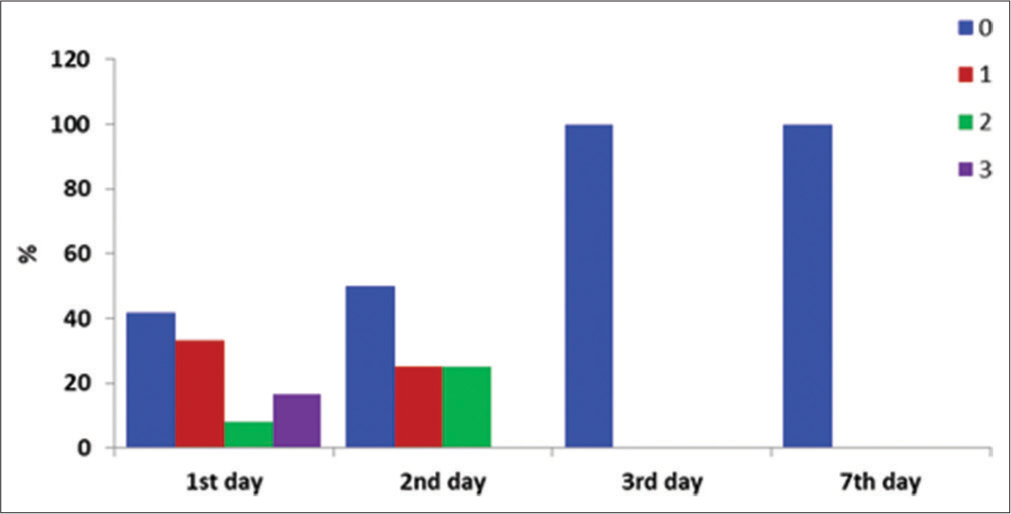
- A bar chart showing laser group.
On the 1st day, about 41.7% of patients had a pain rating scale (0), 33.3% had a score (1), 8.3% had a pain rating scale (2), and 16.7% had a pain rating scale (3).
On the 2nd day, 50.0% of patients had a pain rating scale (0), 25% had a score (1), and 25% had a pain rating scale (2).
On the 3rd day, All the patients (100%) had a pain rating scale (0) with no pain.
Control group
The results in [Table 2 and Figure 4] showed that there is a statistically significant difference between the pain rating scale with different times using the Chi-square test at P < 0.005 (χ2 = 82.19, P ≤ 0.0001).
| Pain rating scale | 1st day | 2nd day | 3rd day | 7th day | Chi-square | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| 0 | - | - | 2 | 8.3 | 8 | 33.3 | 14 | 58.3 | 82.19 | <0.0001** |
| 1 | 2 | 8.3 | 2 | 8.3 | 6 | 25.0 | 6 | 25.0 | ||
| 2 | 2 | 8.3 | 2 | 8.3 | 6 | 25.0 | 2 | 8.3 | ||
| 3 | 2 | 8.3 | 8 | 33.3 | 2 | 8.3 | 2 | 8.3 | ||
| 4 | 8 | 33.3 | 4 | 16.7 | 2 | 8.3 | - | - | ||
| 5 | 8 | 33.3 | 2 | 8.3 | - | - | - | - | ||
| 6 | - | - | 2 | 8.3 | - | - | - | - | ||
| 7 | 2 | 8.3 | - | - | - | - | - | - | ||
| 10 | - | - | 2 | 8.3 | - | - | - | - | 10 | |
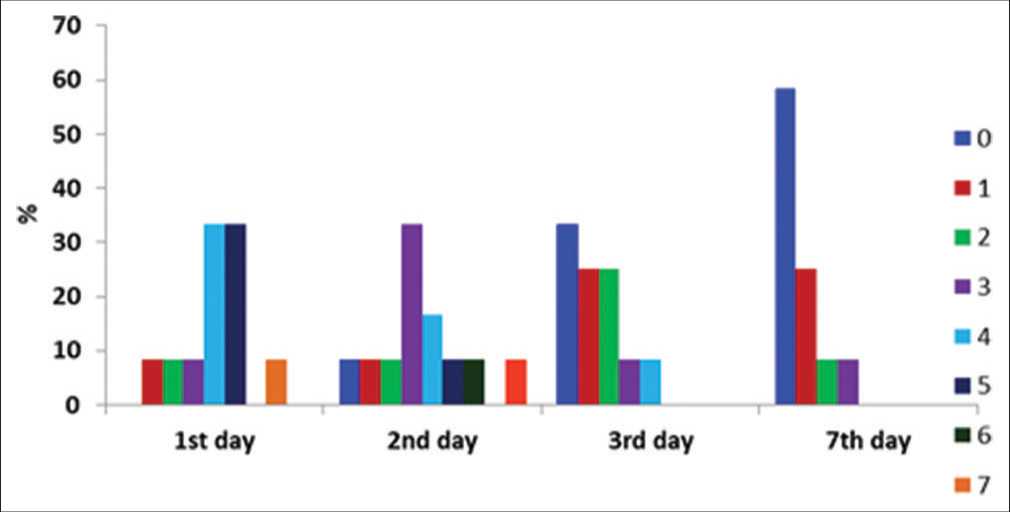
- A bar chart showing the control group.
On the 1st day, no patient had a pain rating scale (0), 33.2% of patients had pain rating scales (1), (2), (3), and (7) (8.3% each), and 66.6% had scores (4) and (5) (33.3% each).
On the 2nd day, 49.8% of the patients had pain rating scales (0), (1), (2), (5), (6), and (10) (8.3 % each). About 33.3% had a score (3), and 16.7% had a pain rating scale (4).
On the 3rd day, 33.3% of the patients had a pain rating scale (0), 50% had a pain rating scale (1) and (2) (25% each), and about 16.7% had a pain rating scale (3) and (4).
After 7 days, 58.3% of the patients had a pain rating scale (0), 25% had a pain rating scale (1), and about 16.7% had pain rating scales (2) and (3).
Comparison between laser and control group
The results in [Table 3 and Figure 5] showed a significant difference between the laser and control group using the Chi-square test at P < 0.005 on different days.
| Pain rating scale | 1st day | 2nd day | 3rd day | 7th day | |||||
|---|---|---|---|---|---|---|---|---|---|
| Laser | Control | Laser | Control | Laser | Control | Laser | Control | ||
| 0 | 10 (41.7) | - | 12 (50.0) | 2 (8.3) | 24 (100.0) | 8 (33.3) | 24 (100.0) | 14 (58.3) | |
| 1 | 8 (33.3) | 2 (8.3) | 6 (25.0) | 2 (8.3) | - | 6 (25.0) | - | 6 (25.0) | |
| 2 | 2 (8.3) | 2 (8.3) | 6 (25.0) | 2 (8.3) | - | 6 (25.0) | - | 2 (8.3) | |
| 3 | 4 (16.7) | 2 (8.3) | - | 8 (33.3) | - | 2 (8.3) | - | 2 (8.3) | |
| 4 | - | 8 (33.3) | - | 4 (16.7) | - | 2 (8.3) | - | - | |
| 5 | - | 8 (33.3) | - | 2 (8.3) | - | - | - | - | |
| 6 | - | - | - | 2 (8.3) | - | - | - | - | |
| 7 | - | 2 (8.3) | - | - | - | - | - | - | |
| 10 | - | - | - | 2 (8.3) | - | - | - | - | |
| Chi-square χ2 | 31.87 | 29.143 | 24.1 | 12.63 | |||||
| P-value | 0.00001724** | 0.000136** | 0.0000798** | 0.00550** | |||||

- A bar chart showing the comparison between laser and control group.
On the 1st day, the results showed that there was a significant difference between the laser and control groups (χ2 = 31.87, P = 0.00001724). In the laser group, 41.7% of patients had no pain, 33.3% had a pain rating scale of 1, 8.3% had a scale of 2, and 16.7% had a score of 16.7. On the other side, in the control group, no patient had a scale of 0, and pain rating scale 1, 2, 4, 5, and 6 was recorded with about 8.3% each; about 33.3% of patients had a scale of 3 and 5 (33.3% each).
On 2nd day, the results showed that there was a significant difference between the laser and control groups (χ2 = 29.143., P = 0.000136). In the laser group, about 50% of patients had no pain, and about 50% had pain rating scales 1 and 2. On the other side, in the control group, 8.3% of patients had a scale of 0, pain rating scale 1, 2, 5, and 9 was recorded with about 8.3% each, and about 33.3% of patients had a scale of 3 and 16.4% had scale 4.
On the 3rd day, the results showed a significant difference between the laser and control groups (χ2 = 24.1, P = 0.0000798). For the laser group, all the patients (100%) had no pain, but only 33.3% had no pain, and the other patients had scales 1, 2, 3, and 4.
On the 7th day, the results showed a significant difference between the laser and control groups (χ2 = 12.63, P = 0.0055). For the control group, about 58.3% of the patients did not suffer from pain, and about 41.7% still suffer from some mild pain ranging between 1 and 3 on pain rating scales.
DISCUSSION
Pain is considered to be a sophisticated experience that includes sensations evoked by and in reaction to noxious stimuli.[10] In addition, it is a major concern for patients and clinicians during orthodontic treatment. Since during the various phases of orthodontic treatment, pain develops in response to the tension and pressure zones generated in the periodontal ligament following the application of force.[11]
This leads to the secretion of inflammatory mediators such as histamine, serotonin, dopamine, glycine, cytokines, leukotrienes, prostaglandins, and substance P, which stimulate free nerve endings, resulting in the perception of pain.[11]
To control pain, conventional methods were used, such as analgesics or anti-inflammatory drugs, which block prostaglandin synthesis by inhibiting cyclooxygenase activity.[12] However, prescribing these drugs is still controversial due to their potential influence on teeth movement and their adverse systemic side effects.[11]
Applications of laser have been widely spread in all fields of dentistry, enhancing dental treatment outcomes. Recently, it has been reported that the usage of LLLT is an efficient means of alleviating orthodontic pain without apparent side effects.[13] LLLT is thought to reduce pain by increasing local blood flow, inhibiting inflammatory substance secretion, inducing neurotransmitter release, altering the conduction and excitation of peripheral nerves, and stimulating endorphin release.[11]
These effects have been attributed to photochemical reactions (biostimulation) at the cellular level in which the light is absorbed by the cellular photoreceptors and converted into adenosine triphosphate by mitochondria. This subsequently increases cellular activities such as DNA, RNA, and protein synthesis. Furthermore, some energy increases the local tissue temperature causing vasodilatation, eventually inducing cellular proliferation, differentiation, and tissue healing.[14]
Thus, the present study was carried out to evaluate the clinical effect of LLLT on pain perception after the placement of initial orthodontic archwires.
This study was a randomized controlled clinical trial with a sample size of 48 patients, who were divided into two groups, each consisting of 24 patients.
The study population in the present study was randomly divided into two equal groups after being eligible for the inclusion and exclusion criteria. The inclusion criteria were based on previously published studies’ eligibility criteria. Patients were considered eligible with ages ranging from 18 to 30, 5–7 mm maxillary dental crowding, and good oral hygiene; this was supported by Celebi et al., 2019.[8]
The patients that were excluded from the study were medically compromised, showing chronic use of analgesic drugs, unerupted teeth, using transpalatal arch, mini-screw, and headgear as a component of treatment; this was also supported by Celebi et al., 2019.[8]
The method of randomization of the present study was performed through computed software, according to Abdel Hamid et al., 2022.[15]
Choosing the control and intervention groups was supported by previously published studies, as they have shown that LLLT may increase the blood supply and promote the healing and recovery of dental tissue.[1] Furthermore, several studies have stated that LLLT reduces orthodontic pain.[14]
In this study, we used the parameters for reducing pain, which can also impact tooth movement. The rate of tooth movement has not been evaluated in this study. However, the researchers in this study published an earlier article regarding this research topic.
The method of assessment in the present study was using the visual analog scale (VAS) to evaluate the intensity of orthodontic pain, and this was the only assessment method used in this trial. It is considered one of the most used methods for subjective evaluation of pain in most of the previous studies due to its reliability in scoring pain scores at different time points when a big difference among participants is expected, as reported by Celebi et al., 2019.[8]
Results of the present study regarding pain perception have shown that there is a statistically significant difference between the pain rating scales with different time intervals (6 h, 2nd day, 3rd day, and 7th day) where the pain has greatly reduced in the laser group at all-time intervals. Hence, significant differences were found between the LLLT and control groups, such that the LLLT group presented lower means of pain scores over almost the entire period in all reported situations. This was in accordance with the previous studies claiming that this could be attributed to its ability to increase blood circulation, reduction in the production of inflammatory factors, and the release of inflammatory neurotransmitters, which will, in turn, lead to a reduction in pain.[16]
Our findings in this study also confirmed the previous clinical trials that also observed the effectiveness of the application of LLLT to control pain in orthodontic treatment. Turhani et al. observed that LLLT immediately after leveling archwire placement reduced the prevalence of pain perception at 6 and 30 h in a single-blinded study with 71 patients[1], and Tortamano et al. concluded that LLLT efficiently controlled pain caused by the first archwire in a double-blinded study with 60 orthodontic patients.[17]
The maximum pain experienced after orthodontic treatment occurs on day 2 after the placement.[18] LLLT has been suggested as a method of controlling this pain.[19] Some studies compared the effect of LLLT and pain killers to reduce pain caused by orthodontic applications.[19] These studies showed that LLLT decreased the pain similarly to painkillers,[19] whether it was applied as a single dose or as a double dose before and after treatment.[20]
However, other studies with randomized clinical evaluation did not detect the positive effects of laser therapy on reducing pain in orthodontic treatment.[8] There are conflicting results in the literature regarding the efficacy of LLLT for orthodontic pain.[8,21] AlSayed Hasan et al.[22] evaluated laser therapy’s effects on reducing orthodontic pain in a randomized controlled trial, and the results from both groups found no effects in pain reduction. However, this contradiction may be due to the difference in the sample size of individuals in the experimental groups between studies and different energy laser irradiation values. Since different protocols and parameters were used, including application protocols and sample sizes, a variety of results was expected.
For the control group, there was an early onset of pain that gradually subsided with time, which was similar to other studies.[21,23] There were statistically significant differences between the VAS scores of the laser group and the control group at all-time intervals. Since it is known that pain intensity is generally more prevalent in the inflammatory phase, during the 1st h and days after the forces caused by orthodontic treatment that is considered to be a tissue injury and, in most cases, pain decreases as tissue repair processes occur.[24]
To control the pain caused by the activation of the orthodontic appliance, painkillers, and analgesics are recommended for daily doses to maintain their effect and also to maintain their effective therapeutic levels in the body. Bernhardt et al.,[25] Bradley et al.,[26] and Steen Law et al.,[27] when investigating the effectiveness of some non-steroidal anti-inflammatory drugs (NSAIDs), found that a percentage of patients used additional doses, as the doses administered were not sufficient to maintain the analgesic action and control the pain caused by the orthodontic procedure. In addition, using such therapeutic drugs could negatively affect the health condition of the patients.
Thus, the application of laser technology as an adjunctive therapy to control pain is recommended to overcome these drawbacks. According to our study, laser therapy demonstrated that only one irradiation provided statistically significantly lower pain levels than the control group at all intervals. LLLT was able to provide a long-lasting analgesic action, with lower pain levels than the control group throughout the study period, which is in line with the results of Eslamian et al.[28] and Fujiyama et al.[29] who found statistically lower values during the first 3 and 4 days; that is, the effect of LLLT reduced the severity and the incidence of painful symptoms during the period of greater discomfort for patients.
Since the first three days are the most common days to encounter pain during orthodontic wires, pain control is paramount for patient pain relief, and avoid the usage of NSAIDs that will prevent cytokines responsible for cyclic movement.
Regarding cost-effectiveness, we just emphasize the clinical application of diode laser for low-level pain therapy, among other clinical applications such as bleaching, oral surgeries, root canal disinfection, periodontal treatment, and other dental procedures.
Even though the pain levels were lower, a considerable portion of the sample experienced some discomfort during the initial phase of treatment. The forces applied to produce tooth movement can generate high levels of pain since it is subjective and related to each patient’s experiences.
Thus, according to the findings of this study, it is recommended that with every patient visit for changing orthodontic wires, photobiomodulation should be performed for pain relief. However, further clinical trials are still needed to evaluate the impact of LLLT on pain perception following the placement of orthodontic archwires.
CONCLUSION
From the present study, the following could be concluded:
Diode laser using 940 nm wavelength with the used parameters showed positive results in reducing pain severity in the early stages of orthodontic treatment
LLLT can have better biomodulating outcomes in promoting long-lasting analgesic action during the period of greatest pain sensitivity.
Ethics approval
This in vivo study was conducted at the Faculty of Dentistry, Suez Canal University. All procedures were in accordance with the ethical standards of Suez Canal University, approved by the Institutional Review Board and REC of the Faculty of Dentistry, Suez Canal University, Ismailia, Egypt (number 460/2022).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006;130:371-7.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of low-level laser therapy during orthodontic movement: A preliminary study. Lasers Med Sci. 2008;23:27-33.
- [CrossRef] [PubMed] [Google Scholar]
- A qualitative study of the early effects of fixed orthodontic treatment on dietary intake and behaviour in adolescent patients. Eur J Orthod. 2012;34:432-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of low-power laser irradiation (LPLI) at different wavelengths and doses on oxidative stress and fibrogenesis parameters in an animal model of wound healing. Lasers Med Sci. 2011;26:125-31.
- [CrossRef] [PubMed] [Google Scholar]
- Aspirin, acetaminophen, and ibuprofen: Their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:364-70.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of low intensity laser on pain sensitivity during orthodontic movement. Dental Press J Orthod. 2011;16:95-102.
- [CrossRef] [Google Scholar]
- Effect of a single dose of low-level laser therapy on spontaneous and chewing pain caused by elastomeric separators. Am J Orthod Dentofacial Orthop. 2016;149:62-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of low-level laser therapy and mechanical vibration on orthodontic pain caused by initial archwire. Am J Orthod Dentofacial Orthop. 2019;156:87-93.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between the effect of low-level laser therapy and corticotomy-facilitated orthodontics on RANKL release during orthodontic tooth movement: A randomized controlled trial. Laser Dent Sci. 2019;3:99-109.
- [CrossRef] [Google Scholar]
- Orthodontic pain: From causes to management-a review. Eur J Orthod. 2007;29:170-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of low level laser therapy on pain perception following orthodontic elastomeric separation. J Clin Diagn Res. 2016;10:23-8.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of lidocaine/prilocaine topical anesthetic on pain and discomfort associated with orthodontic elastomeric seperator placement. Prog Orthod. 2017;18:1.
- [CrossRef] [PubMed] [Google Scholar]
- Photobiomodulation in orthodontics: Unveiling the paradox. Laser Dent Sci. 2022;6:233-5.
- [CrossRef] [Google Scholar]
- The effectiveness of low-level laser therapy on orthodontic tooth movement: A systematic review. Laser Dent Sci. 2023;7:129-37.
- [CrossRef] [Google Scholar]
- Clinical and radiographic evaluation of diode laser and chemical disinfection in comparison to selective caries removal in management of patients with deep carious lesions. Laser Dent Sci. 2022;6:219-31.
- [CrossRef] [Google Scholar]
- Evaluating low-level laser therapy effect on reducing orthodontic pain using two laser energy values: A split-mouth randomized placebo-controlled trial. Eur J Orthod. 2018;40:23-8.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level laser therapy for pain caused by placement of the first orthodontic archwire: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136:662-7.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of functional and esthetic expectations on orthodontic pain. J Orofac Orthop. 2023;84:141-6.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of low-level laser therapy versus paracetamol-caffeine in controlling orthodontic separation pain and changes in the oral-health-related quality of life in Class I malocclusions: A 3-arm, randomized, placebo-controlled clinical trial. J World Fed Orthod. 2022;11:75-82.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of a single versus double application of low-level laser therapy in pain reduction following orthodontic elastomeric separation: A randomized controlled trial. Dent Med Probl. 2020;57:45-52.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79-85.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level laser therapy effectiveness in reducing initial orthodontic archwire placement pain in premolars extraction cases: A single-blind, placebo-controlled, randomized clinical trial. BMC Oral Health. 2020;20:209.
- [CrossRef] [PubMed] [Google Scholar]
- Analgesic effect of a low-level laser therapy (830 nm) in early orthodontic treatment. Lasers Med Sci. 2013;28:335-41.
- [CrossRef] [PubMed] [Google Scholar]
- Efficiency of low-level laser therapy in reducing pain induced by orthodontic forces. Photomed Laser Surg. 2012;30:460-5.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop. 2001;120:20-7.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized clinical trial comparing the efficacy of ibuprofen and paracetamol in the control of orthodontic pain. Am J Orthod Dentofacial Orthop. 2007;132:511-7.
- [CrossRef] [PubMed] [Google Scholar]
- An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofacial Orthop. 2000;118:629-35.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci. 2014;29:559-64.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical effect of CO2 laser in reducing pain in orthodontics. Angle Orthod. 2008;78:299-303.
- [CrossRef] [PubMed] [Google Scholar]







