Translate this page into:
Comparison of skeletal and dentoalveolar changes between pure bone-borne and hybrid tooth-borne and bone-borne maxillary rapid palatal expanders using cone-beam computed tomography

*Corresponding author: Ghaddy AlSaty, Department of Orthodontics, West Virginia University, Morgantown, West Virginia, United States. ghadysaty@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sarraj M, Akyalcin S, He H, Xiang J, AlSaty G, Celenk-Koca T, et al. Comparison of skeletal and dentoalveolar changes between pure bone-borne and hybrid tooth-borne and bone-borne maxillary rapid palatal expanders using cone-beam computed tomography. APOS Trends Orthod 2021;11(1):32-40.
Abstract
Objectives:
The objectives of the study were to compare the skeletal, dentoalveolar, and periodontal changes between two types of microimplant-assisted rapid maxillary expansion appliances: The bone-anchored maxillary expanders (BAME) and the tooth-bone-anchored maxillary skeletal expander (MSE).
Materials and Methods:
Thirty-four patients with a transverse maxillary deficiency were divided into two groups; the first group (16 patients, average age 14.9 years) was treated with the MSE appliance, and the second group (18 patients, average age 13.8 years) was treated with the BAME appliance. Cone-beam computed tomography scans were taken at pre-treatment (T1) and immediately post-expansion (T2) to measure the changes in midpalatal suture opening, total expansion (TE), alveolar bone bending, dental tipping (DT), and buccal bone thickness. Data were analyzed using paired t-test and two-sample t-test.
Results:
Midpalatal suture separation was found in 100% of the patients in both groups. The TE at the first molar was 5.9 mm in the MSE group and 4.7 mm in the BAME group. The skeletal contributions were 56% and 83% of TE for the MSE and BAME groups, respectively. Significantly less dental buccal tipping and buccal bone loss were found with the BAME group. The midpalatal suture in both groups exhibited a parallel opening pattern in the axial plane.
Conclusion:
The use of BAME appliance resulted in greater skeletal effects, less dental tipping, and less buccal bone reduction compared to MSE appliance (immediately after maxillary expansion).
Keywords
Cone-beam computed tomography
Bone-borne maxillary expanders
Microimplant-assisted rapid maxillary expansion
INTRODUCTION
Maxillary transverse deficiency (MTD) is a problem that is commonly found in patients who seek orthodontic care. It has been reported that 9.4% of the population and nearly 30% of adult orthodontic patients have MTD related to a posterior crossbite.[1] Orthopedic maxillary expansion is used to correct skeletal MTD, posterior dental crossbites, or increase dental arch perimeter.[2,3] The primary goal of maxillary expansion is to maximize the orthopedic effect, while minimizing the movement of teeth. In tooth-borne expanders, the expansion forces are transmitted through the teeth to the bony structures, thus decreasing the amount of force transmitted to the bony structures and resulted in undesirable tooth movement.[4] This led to the introduction of the first bone-borne appliance (distractor) in 1999. Bone-anchored maxillary expansion appliances transmitted forces directly to the skeletal components, resulting in more skeletal movement.[1,5-9] Subsequently, there are various designs of bone-anchored expander available in the market. One form of microimplant-assisted rapid maxillary expansion (MARPE) is the hybrid tooth-borne and bone-borne maxillary skeletal expander (MSE) which uses mini-implants (bone anchor) and maxillary teeth (tooth anchor) for anchorage. The other form is the pure bone-borne maxillary expanders (BAME), which uses only mini-implants as anchorage. It was proven that MARPE has increased the rate of success in separation of the midpalatal suture in young adults with approximately 84–87% success rate, but it is clear that there exists some cases of failure of separation of the midpalatal suture and incidents of asymmetric expansion because of unilateral separation of the frontomaxillary suture.[10] Although many studies have evaluated the skeletal and dental response with these two types of expanders, treatment effects still remain controversial . However, many studies have shown that the extent of skeletal changes and the nature of dental archform widening are different.[11,12] The purpose of this study was to compare and to gain a better understanding of the skeletal, dentoalveolar, and periodontal changes including the changes in midpalatal suture opening (MSO), total expansion (TE), alveolar bone bending (ABB), dental tipping (DT), and buccal bone thickness (BBT) between the MSE and the BAME appliances using cone-beam computed tomography (CBCT). The null hypothesis is that there is no difference in skeletal and dental changes with the two types of maxillary expansion appliances.
MATERIALS AND METHODS
This study has been approved and exempted by the Institutional Review Board at West Virginia University (Ref#: 1909722030). Permission to use patient data was obtained from the Tufts University School of Dentistry and Wuhan University School of Stomatology.
A total of 52 patients were recruited for the study who received treatment with either the MSE or the BAME appliance between 2017 and 2019. The patients were selected by one investigator of each department according to the inclusion and exclusion criteria. The inclusion criteria included (1) individuals presenting with well-balanced facial ratios and normal growth pattern; (2) patients in the permanent dentition with moderate maxillary transverse discrepancy with an intermolar width (IMW) <36 mm; (3) patients completed treatment with either the MSE or the BAME appliances; and (4) patients who have CBCT scans of diagnostic quality captured before and immediately after expansion. Patients with incomplete records, craniofacial anomalies, compliance problems, need for surgically assisted expansion, and previous orthodontic treatment history were excluded from the study. The sample size, which was 52 subjects, was calculated using G*Power (Faul, Erdfelder, Lang and Buchner, 2007) for the two independent sample t-test to detect large effect (d = 0.80) with statistical power at 0.80 and α = 0.05 significance level. Thirty-six patients met the inclusion and exclusion criteria. Two additional patients were further excluded due to insufficient field of view on the CBCT scans giving a total of 34 subjects in the final sample. Sixteen patients (10 females and 6 males) with an average age of 14.9 years were from the archive of the Department of Orthodontics in Wuhan University treated with the MSE appliances. This sample was compared to 18 patients (16 females and 2 males) with an average age of 13.8 years from the archive of the Department of Orthodontics at Tufts University treated with the BAME appliances.
Pre-expansion (T1) and immediate post-expansion (T2) CBCT scans were collected from Wuhan University School of Stomatology with the NewTom VGi9 3D CBCT unit (Imola, Italy) and Tufts University School of Dentistry with the Kodak CS 9000 3D CBCT unit (CareStream Health, Inc., Rochester, NY, USA). The images were calibrated using the same parameters: Exposure of 10 mA for 32.5 s, power of 70 kVp, and 76 μm voxel size with volume dimensions of 8 cm × 8 cm. All CBCT scans taken with the Frankfort plane parallel to the floor and clenching on intercuspal position. The DICOM files were assessed using the dolphin imaging software (version 11.95, Dolphin Imaging and Management Solutions, Chatsworth, CA).
Appliance design
[Figures 1a and b] shows the design of MSE appliance (BioMaterials Korea, Inc.). The appliance consists of a central expansion jackscrew and two or four attached arms soldered to orthodontic bands. The jet screws were connected to the maxillary first molars (M1) as recommended by the manufacturer. In a few cases (two out of 16 cases), the jet screws were connected to the premolars in addition to the M1 either for additional anchorage or for Class III maxillary protraction cases. Four minis-screws were always placed in the palate with either the 2- or 4-armed appliance. The two anterior mini-screws were inserted bilaterally between the roots of the first premolars (PM1) and second premolars (PM2), and the other two posterior mini-screws were inserted between the roots of the PM2 and M1, 6–8 mm palatal to the gingival margin of the teeth with a perpendicular insertion into the alveolar bone between the roots. Welded to the central expansion screw are four tubes that serve as guides for the placement of the microimplants. The microimplants allow for fixation of the expander flushed to the palate and are 1.5–1.8 mm in diameter and 11 mm in length. The microimplant length allows for bicortical engagement of the palatal and nasal floor [Figure 2], while the diameter allows for a secure fit within the tubes, reducing the magnitude of lateral force transfer to anchored teeth during appliance activation.
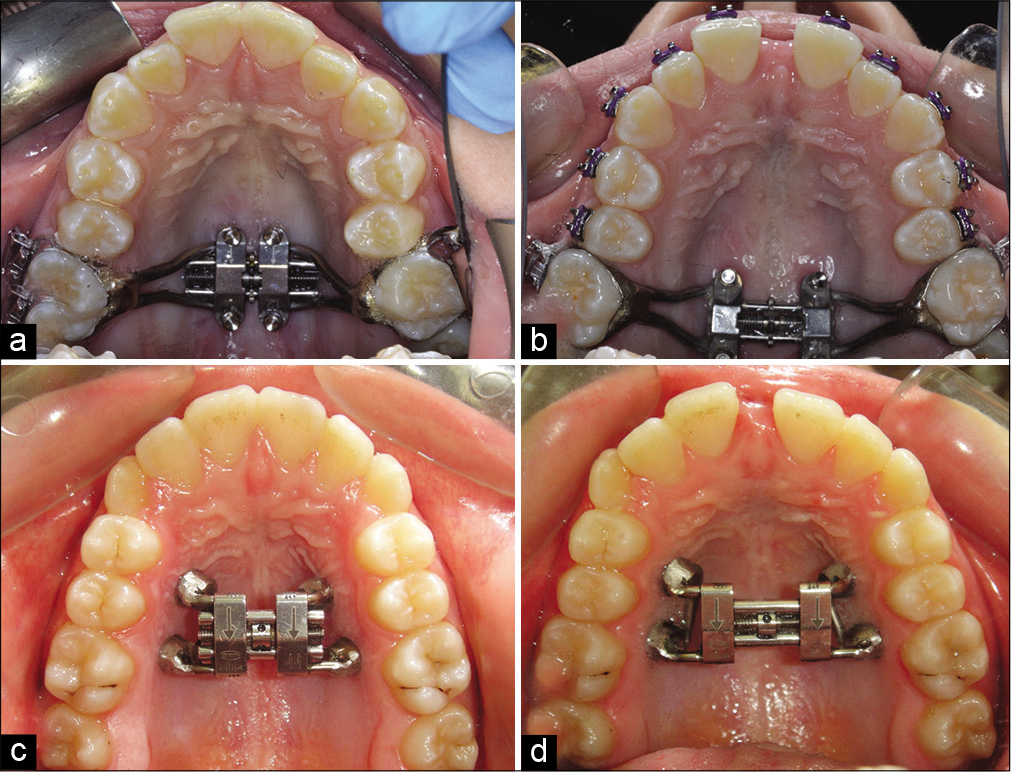
- Pre- (a) and post-expansion (b) occlusal photographs of a patient from the maxillary skeletal expander group. Pre- (c) and post-expansion (d) occlusal photographs of a patient from the bone-anchored maxillary expanders group.
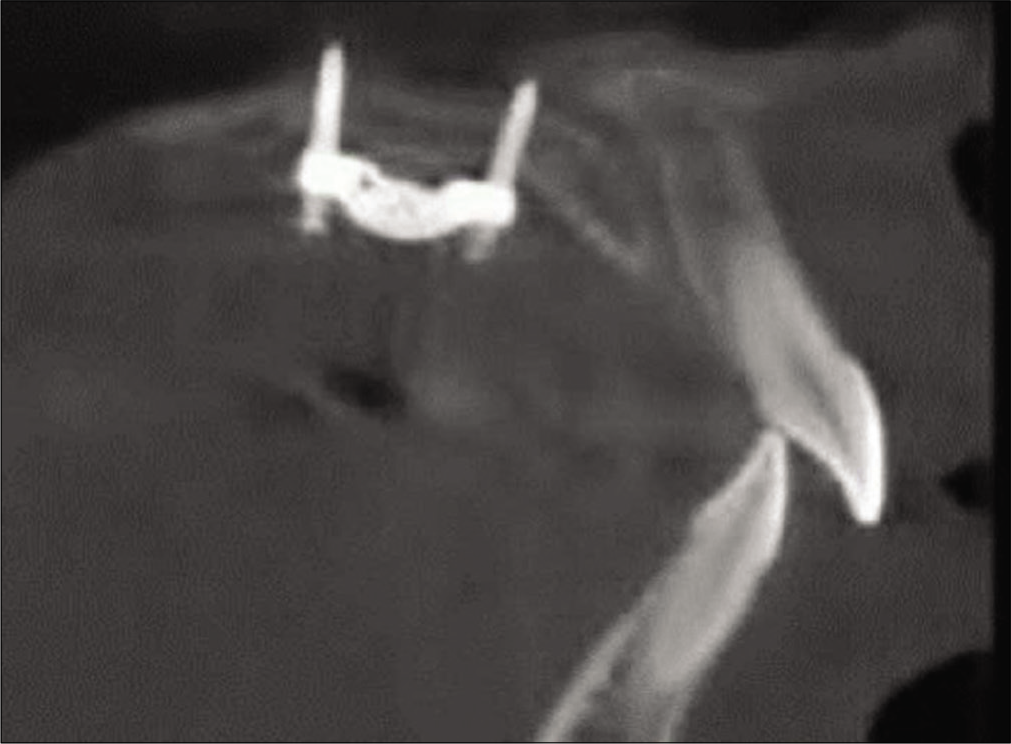
- Bicortical engagement in palatal and nasal floor.
[Figures 1c and d] shows the design of the BAME appliance (Orlus, Ortholution Co., Seoul, Korea) which consists of a central expansion jackscrew and four extension arms that were fitted, and laser welded on the copings in the laboratory. The microimplants are 1.8 mm × 9 mm and were placed 6–8 mm palatal to the gingival margin of the teeth with a perpendicular insertion into the alveolar bone between the roots using a contra-angle driver (Unitek REF 504-315, 3M Unitek, Monrovia, CA). Anterior implants were placed bilaterally between the roots of the first and PM2, and posterior implants were placed between the roots of the PM2 and M1. The amount of appliance activation each patient received varied with the magnitude of transverse discrepancy between the upper and lower jaw. For both groups, the activation protocol consisted of two turns daily until the outcome was achieved.
Measurements analysis
All CBCT volumes were oriented in three planes of space to standardize for image analysis [Figure 3]. The image volume reorientation process and CBCT analysis were adopted from the method by Ngan et al.[13]
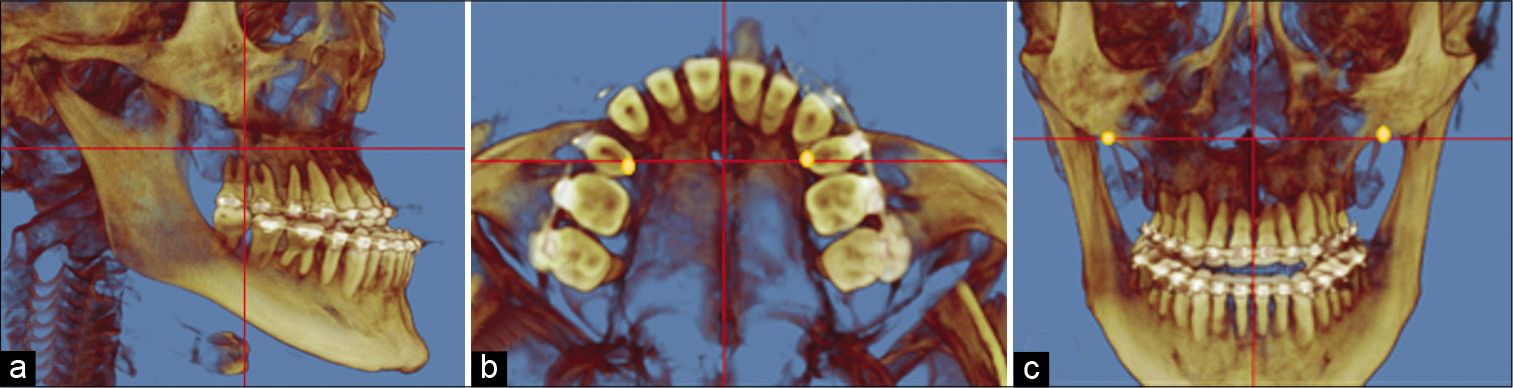
- Cone-beam computed tomography head orientation in three planes of space; (a) sagittal, (b) axial, and (c) coronal.
The sagittal view was oriented parallel to the software’s horizontal indicator line that transverses the middle of the palatal plane (ANS-PNS). The axial view was oriented parallel to the software’s horizontal line that connected the left and right lingual cusps of the upper PM1. The coronal view was oriented parallel to software’s horizontal position indicator line that connected the left and right intersection of lateral contour of the maxillary alveolar process and the lower contour of the maxillozygomatic process of the maxilla (jugal point).
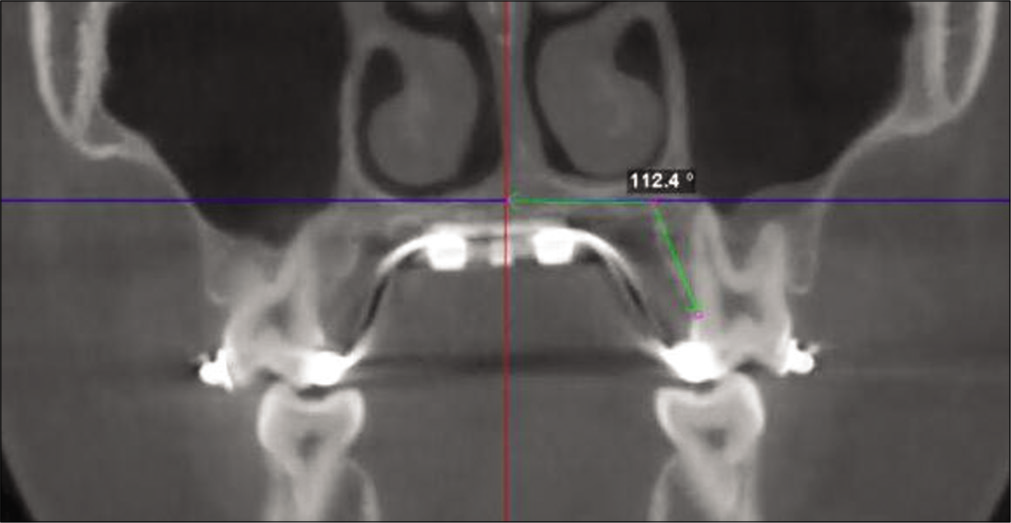
TE achieved with the MARPE appliance includes the direct separation of the maxillary halves at the midpalatal suture (skeletal expansion) along with ABB and DT (dentoalveolar expansion). TE at the M1 was defined as the change in IMW between the palatal cusp tip of the right and left M1 through the center of M1. TE at the PM1 was defined as the change between (T2-T1) in the interpremolar width, the distance between the palatal cusp tip of the right and left PM1 measured through the center of PM1 [Figure 4].
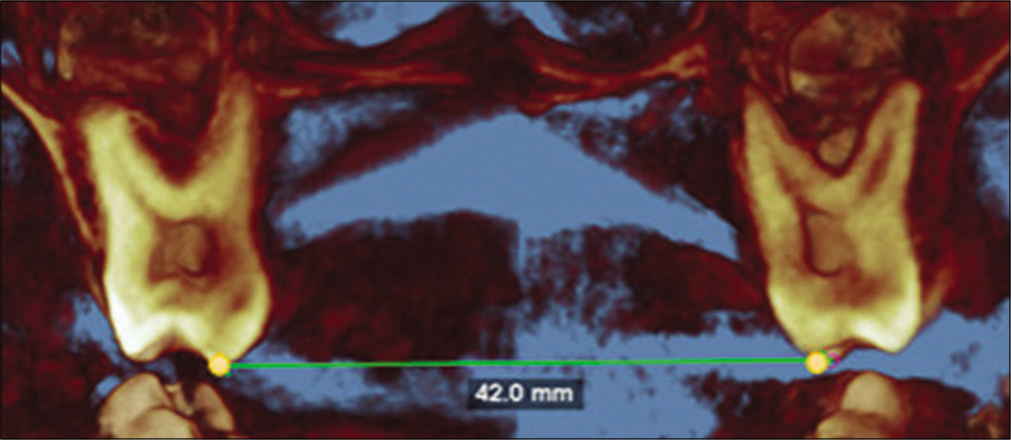
- Measurement of intermolar width on a coronal cross-sectional slice.
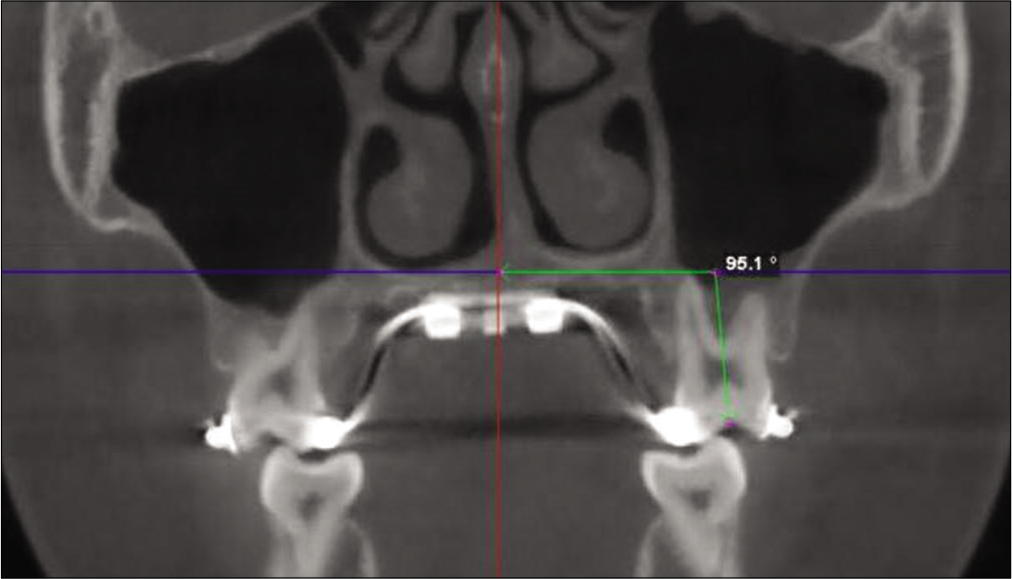
ABB angle was defined as the difference between the palatal alveolar bone angles measured for the anchored teeth PM1, M1, or both, on a coronal cross-sectional slice through the mid-portion of the teeth [Figure 5].
- Measurement of alveolar bone bending angle for first molar by measuring the intersecting angle formed by a best fit line through the palatal cortical plate and the software’s horizontal indicator line that transverse the middle of the palate.
DT angle (DTA) was defined as the degree difference between the DTA measured for the anchored teeth, PM1, M1, or both, on a coronal cross-sectional slice through the mid-portion of the teeth. [Figure 6] shows the DTA value obtained for M1 by measuring the intersecting angle formed by a best fit line through the long axis of the tooth and the software’s horizontal indicator line that transverses the middle of the palate. A positive change in DT indicates DT toward the buccal direction, while a negative change indicates DT toward palatal direction.
- Measurement of dental tipping angle for first molar (M1) by measuring the intersecting angle formed by a best fit line through the long axis of M1 and the software’s horizontal indicator line that transverse the middle of the palate.
BBT was defined as the perpendicular distance between the most facial surface of the tested tooth and the external aspect of the maxillary buccal cortical plate. It was measured for PM1, and the mesiobuccal root of M1 when PM1, M1, or both were used for appliance anchorage through the furcation of M1 [Figure 7].
- Measurement of buccal bone thickness for first pre-molar and mesiobuccal root of first molar.
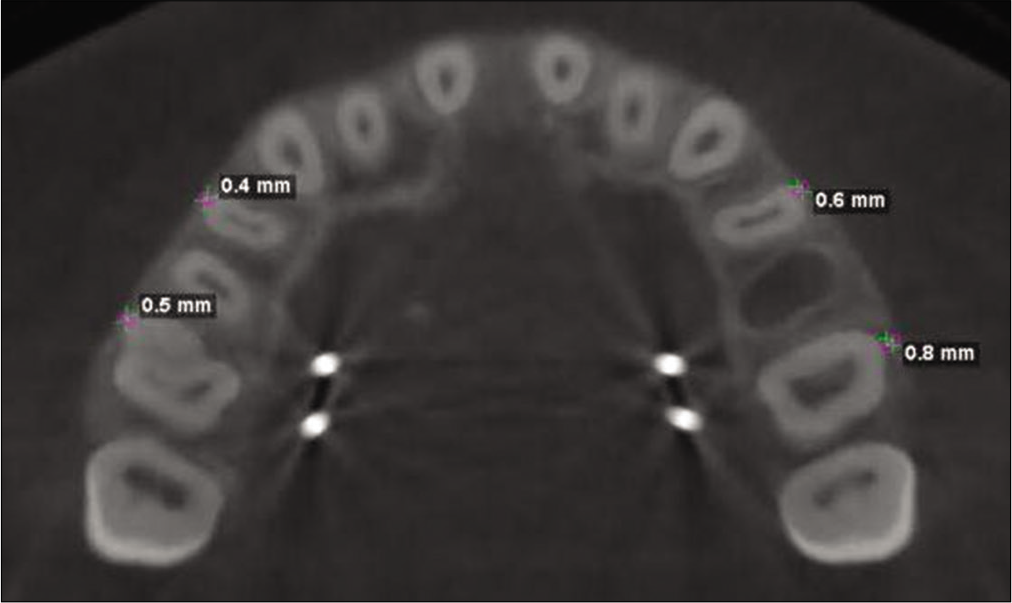
MSO was recorded at the canine (C), PM1, PM2, and M1. Suture width opening was measured between the right and left external edges of the suture on an axial cross-sectional slice through the center of the palate [Figure 8].
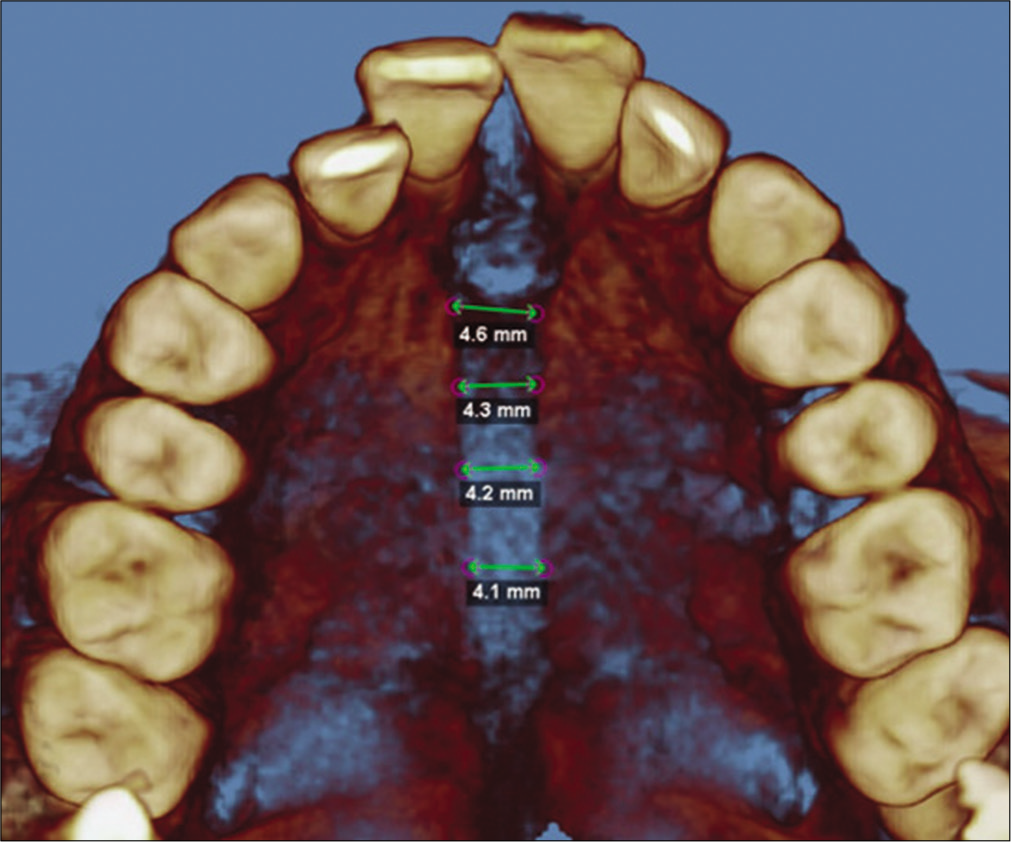
- Measurement of sutural expansion on an axial cross-sectional slice through the midpalate at the canine, first pre-molar, second pre-molar, and first molar.
Midpalatal suture expansion pattern was defined as successful midpalatal suture separation and was measured at the C, PM1, PM2, and M1 [Figure 8].
Statistical analysis
All statistical analyses were conducted using SAS (version 9.4, 2013, SAS Institute Inc., Cary, NC). Paired t-test was utilized to evaluate skeletal, dentoalveolar and periodontal changes after maxillary expansion using MSE and BAME. To compare the difference between MSE and BAME groups, two independent sample t-tests were conducted. Intraclass correlation coefficients (ICCs) were calculated to evaluate the reliability of the measurements. All statistical tests were two-sided and P < 0.05 was considered statistically significant.
RESULTS
For error measurements, 10 subjects were measured by the same researcher a 2nd time with a 2 weeks interval in between. The reliability coefficient was found to determine the repeatability of the measures made for the variables in this study. ICCs of all measurements except two (>0.80) were higher than 0.90, indicating a high level of agreement between the two measurements [Table 1].
| Variables | Intraclass correlation coefficient |
|---|---|
| IMW pre | 0.994 |
| IMW post | 0.994 |
| IPMW pre | 0.997 |
| IPMW post | 0.991 |
| ABB right pre (M1) | 0.979 |
| ABB right post (M1) | 0.987 |
| ABB left pre (M1) | 0.897 |
| ABB left post (M1) | 0.969 |
| ABB right pre (PM1) | 0.987 |
| ABB right post (PM1) | 0.992 |
| ABB left pre (PM1) | 0.941 |
| ABB left post (PM1) | 0.993 |
| DT right pre (M1) | 0.959 |
| DT right post (M1) | 0.984 |
| DT left pre (M1) | 0.948 |
| DT left post (M1) | 0.980 |
| DT right pre (PM1) | 0.981 |
| DT right post (PM1) | 0.997 |
| DT left pre (PM1) | 0.989 |
| DT left post (PM1) | 0.996 |
| BBT right pre (M1) | 0.985 |
| BBT right post (M1) | 0.988 |
| BBT left pre (M1) | 0.975 |
| BBT left post (M1) | 0.960 |
| BBT right pre (PM1) | 0.933 |
| BBT right post (PM1) | 0.811 |
| BBT left pre (PM1) | 0.973 |
| BBT left post (PM1) | 0.954 |
| Midpalatal suture post (C) | 0.996 |
| Midpalatal suture post (PM1) | 0.997 |
| Midpalatal suture post (PM2) | 0.997 |
| Midpalatal suture post (M1) | 0.919 |
IMW: Intramolar width, IPMW: Intrapremolar width, ABB: Alveolar bone bending, DT: Dental tipping, BBT: Buccal bone thickness, M1: First molar, PM2: Second pre-molar, PM1: First pre-molar, C: Canine.
TE
The TE achieved with MSE treatment was 5.9 ± 1.6 mm at the M1. The percentage of skeletal expansion was 56% determined by the mean midpalatal suture expansion of 3.3 ± 1.4 mm. The remaining 44% was attributed to dentoalveolar expansion [Table 2]. The TE achieved with BAME treatment was 4.7 ± 1.8 mm. The percentage of skeletal expansion was 83% and the dentoalveolar expansion was 17% [Table 3].
| Pre-expansion (T1) | Post-expansion (T2) | Change (T2-T1) | t (df=15)a | Pb | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| IMW | 40.9 | 3.6 | 46.8 | 3.4 | 5.9 | 1.6 | 14.7 | <0.0001*** |
| PMW | 30.2 | 2.7 | 34.3 | 3.1 | 4.1 | 2.1 | 7.6 | <0.0001*** |
| ABB right (M1) | 110.4 | 8.6 | 116.7 | 8.8 | 6.4 | 4.9 | 5.2 | 0.0001*** |
| ABB left (M1) | 108.0 | 9.3 | 112.2 | 9.1 | 4.1 | 4.0 | 4.2 | 0.0009*** |
| ABB right (PM1) | 121.9 | 11.1 | 126.7 | 10.2 | 4.8 | 5.0 | 3.6 | 0.003** |
| ABB left (PM1) | 121.3 | 12.0 | 126.8 | 11.2 | 5.5 | 6.0 | 3.5 | 0.004** |
| DT right (M1) | 96.6 | 4.6 | 100.7 | 5.4 | 4.0 | 2.3 | 6.9 | <0.0001*** |
| DT left (M1) | 96.7 | 5.8 | 99.5 | 6.8 | 2.8 | 2.5 | 4.4 | 0.0005*** |
| DT right (PM1) | 90.3 | 13.9 | 91.9 | 15.0 | 1.5 | 2.5 | 2.3 | 0.04* |
| DT left (PM1) | 92.4 | 6.3 | 94.2 | 8.0 | 2.2 | 4.7 | 1.7 | 0.11 |
| BBT left (M1) | 1.6 | 0.8 | 1.1 | 0.7 | –0.5 | 0.2 | –8.1 | <0.0001*** |
| BBT right (PM1) | 0.9 | 0.5 | 0.5 | 0.5 | –0.4 | 0.3 | –4.3 | 0.0009*** |
| BBT right (M1) | 1.8 | 0.7 | 1.1 | 0.6 | –0.7 | 0.4 | –6.0 | <0.0001*** |
| BBT left (PM) | 0.8 | 0.4 | 0.4 | 0.3 | –0.3 | 0.2 | –8.3 | <0.0001*** |
| MSO (C) | 0 | 0 | 4.1 | 1.8 | 4.1 | 1.8 | 9.2 | <0.0001*** |
| MSO (PM1) | 0 | 0 | 3.8 | 1.8 | 3.8 | 1.8 | 8.2 | <0.0001*** |
| MSO (PM2 ) | 0 | 0 | 3.5 | 1.6 | 3.5 | 1.6 | 8.5 | <.0001*** |
| MSO (M1) | 0 | 0 | 3.3 | 1.4 | 3.3 | 1.4 | 8.7 | <0.0001*** |
MSE: Maxillary skeletal expander, IMW: Intramolar width, IPMW: Intrapremolar width, ABB: Alveolar bone bending, DT: Dental tipping, BBT: Buccal bone thickness, MSO: Mid-palatal suture opening, M1: First molar, PM2: Second pre-molar, PM1: First pre-molar, C: Canine. at-value from paired t test. df: Degree of freedom. bP-value from paired t-test. *P<0.05, **P<0.01, ***P<0.001
| Measurements | Pre-expansion (T1) | Post-expansion (T2) | Change (T2-T1) | t (df=17)a | Pb | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| IMW | 36.5 | 4.1 | 41.2 | 3.3 | 4.7 | 1.8 | 11.4 | <0.0001*** |
| PMW | 25.7 | 2.2 | 30.4 | 2.4 | 4.7 | 1.4 | 14.5 | <0.0001*** |
| ABB right (M1) | 103.6 | 5.9 | 107.4 | 6.6 | 3.9 | 4.5 | 3.6 | 0.002** |
| ABB left (M1) | 103.6 | 5.9 | 108.9 | 7.3 | 5.3 | 5.5 | 4.1 | 0.0008*** |
| ABB right (PM1) | 120.8 | 12.6 | 125.2 | 11.7 | 4.4 | 4.9 | 3.8 | 0.002** |
| ABB left (PM1) | 118.6 | 10.8 | 123.0 | 13.2 | 4.1 | 6.3 | 2.7 | 0.02* |
| DT right (M1) | 94.3 | 6.0 | 94.8 | 4.3 | 0.4 | 3.5 | 0.5 | 0.60 |
| DT left (M1) | 96.5 | 6.9 | 97.0 | 5.2 | 0.5 | 3.0 | 0.7 | 0.50 |
| DT right (PM1) | 91.2 | 4.2 | 89.8 | 4.5 | –1.4 | 2.6 | –2.3 | 0.04* |
| DT left (PM1) | 90.7 | 3.9 | 90.0 | 3.8 | –0.7 | 2.4 | –1.2 | 0.27 |
| BBT right (M1) | 1.2 | 0.5 | 0.9 | 0.5 | –0.2 | 0.3 | –3.6 | 0.002** |
| BBT left (M1) | 1.0 | 0.5 | 0.9 | 0.6 | –0.1 | 0.3 | –1.7 | 0.12 |
| BBT right (PM1) | 0.6 | 0.3 | 0.5 | 0.3 | –0.1 | 0.1 | –2.9 | 0.009** |
| BBT left (PM) | 0.6 | 0.3 | 0.5 | 0.3 | –0.1 | 0.2 | –2.9 | 0.009** |
| MSO (C) | 0 | 0 | 4.8 | 1.3 | 4.8 | 1.3 | 15.8 | <0.0001*** |
| MSO (PM1) | 0 | 0 | 4.4 | 1.2 | 4.4 | 1.2 | 15.5 | <0.0001 |
| MSO (PM2 ) | 0 | 0 | 4.2 | 2.3 | 4.2 | 1.2 | 15.0 | <0.0001*** |
| MSO (M1) | 0 | 0 | 3.9 | 1.2 | 3.9 | 1.2 | 12.9 | <0.0001*** |
BAME: Bone-anchored maxillary expanders, IMW: Intramolar width, IPMW: Intrapremolar width, ABB: Alveolar bone bending, DT: Dental tipping, BBT: Buccal bone thickness, MSO: Midpalatal suture opening, M1: First molar, PM2: Second pre-molar, PM1: First pre-molar, C: Canine. at-value from paired t-test. df: Degree of freedom. bP-value from paired t-test. *P<0.05, **P<0.01, ***P<0.001
ABB angle
Significant increase in ABB angle at M1 and PM1 was found on both the right and left sides between T2 and T1 by mean of 6.4°, 4.1°, 4.8°, and 5.5°, respectively, in the MSE group [Table 2]. In the BAME group, the increase was 3.9°, 5.3°, 4.4°, and 4.1°, respectively [Table 3]. No significant differences were found in the ABB between the two groups [Table 4].
| MSE (n=16) | BAME (n=18) | T (df=32)a | Pb | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| IMW | 5.9 | 1.6 | 4.7 | 1.8 | 2.0 | 0.06 |
| PMW | 4.1 | 2.1 | 4.7 | 1.4 | –1.1 | 0.29 |
| ABB right (M1) | 6.4 | 4.9 | 3.9 | 4.5 | 1.5 | 0.13 |
| ABB left (M1) | 4.1 | 4.0 | 5.3 | 5.5 | –0.7 | 0.49 |
| ABB right (PM1) | 4.8 | 5.0 | 4.4 | 4.9 | 0.3 | 0.80 |
| ABB left (PM1) | 5.5 | 6.0 | 4.1 | 6.1 | 0.7 | 0.52 |
| DT right (M1) | 4.0 | 2.3 | 0.4 | 3.5 | 3.5 | 0.002** |
| DT left (M1) | 2.8 | 2.5 | 0.5 | 3.0 | 2.4 | 0.02* |
| DT right (PM1) | 1.5 | 2.5 | –1.4 | 2.6 | 3.2 | 0.003** |
| DT left (PM1) | 2.2 | 4.7 | –0.7 | 2.4 | 2.0 | 0.06 |
| BBT right (M1) | –0.7 | 0.4 | –0.2 | 0.3 | –3.4 | 0.002** |
| BBT left (M1) | –0.5 | 0.2 | –0.1 | 0.3 | –4.4 | 0.0001*** |
| BBT right (PM1) | –0.4 | 0.3 | –0.1 | 0.1 | –2.9 | 0.009** |
| BBT left (PM) | –0.3 | 0.2 | –0.1 | 0.2 | –3.0 | 0.006** |
| MSO (C) | 4.1 | 1.8 | 4.8 | 1.3 | –1.3 | 0.20 |
| MSO (PM1) | 3.8 | 1.8 | 4.4 | 1.2 | –1.2 | 0.25 |
| MSO (PM2 ) | 3.5 | 1.6 | 4.2 | 1.2 | –1.4 | 0.17 |
| MSO (M1) | 3.3 | 1.4 | 3.9 | 1.2 | –1.2 | 0.25 |
BAME: Bone-anchored maxillary expanders, MSE: Maxillary skeletal expander, IMW: Intramolar width, IPMW: Intrapremolar width, ABB: Alveolar bone bending, DT: Dental tipping, BBT: Buccal bone thickness, MSO: Midpalatal suture opening, M1: First molar, PM2: Second pre-molar, PM1: First pre-molar, C: Canine. at-value from paired t-test. df: Degree of freedom. bP-value from paired t-test. *P<0.05, **P<0.01, ***P<0.001
DTA
In the MSE group, significant increase in DTA was found toward the buccal at M1 on both right (4°) and left (2.8°) sides, and also at PM1 on the right side (1.5°) only. However, no significant increase was found toward the buccal at PM1 on the left side [Table 2]. In the BAME group, no significant increase was found toward the buccal side at the M1 on both the right and left sides. A significant decrease was found toward the palate at the PM1 which was found on the right side (−1.4°) [Table 3].
BBT
In the MSE group, a significant decrease was found at the M1 and PM1 on both the right and left sides with mean measurements of −0.7 mm, −0.5 mm, −0.4 mm, and −0.3 mm [Table 2]. In the BAME group, a significant decrease was found at the M1 on the right side by means of 0.2 and PM1 on both sides by mean of 0.1 mm and 0.1 mm, respectively. However, there was no significant decrease on the left side for M1 [Table 3].
MSO
In the MSE group, mean MSO (mm) at the C, PM1, PM2, and M1 ranged from 1.3 to 7.3, 1.3 to 6.6, 1.4 to 6.1, and 1.8 to 6.1, respectively. In the BAME group, the mean MSO for these sites ranged from 1.3 to 6.7, 1.8 to 6.5, 2.3 to 6.1, and 1.6 to 5.6, respectively. These results indicate a more parallel expansion along the length of the midpalatal suture in both groups [Table 4].
Both study groups showed a decrease in BBT at the M1 and PM1. However, the results [Table 4] from the two sample t-tests showed that the BAME group experienced significantly less buccal bone loss than the MSE group for both the M1 and PM1 (P < 0.05). Molar root inclination measurements from the MSE group demonstrated a mean buccal crown tipping of 3.4°, whereas the BAME group produced 0.45° of buccal crown tipping. Premolar root angulation changes revealed 1.85° buccal and −1.05° of lingual crown tipping in MSE and BAME groups, respectively. The differences between the two groups were significant (P < 0.05).
DISCUSSION
The results of this study show that both types of MARPE appliances are effective in achieving sutural separation in young adolescent patients. This finding agrees with the results published by several previous studies.[14-17] Most of the subjects demonstrated successful maxillary expansion, evident by the opening of the midpalatal suture. The total amount of expansion varied from study to study due to the type of appliance, duration of treatment, and the rate of screw activations. In the literature, the range of expansion varied from 4.2 mm to 8.0 mm.[17]
In this study, the TE at the M1 ranged from 2.9 mm to 7.9 mm in the MSE group, and 1.8 mm to 8.6 mm in the BAME group. The skeletal contribution was 56% in the MSE group and 83% in the BAME group. This is in agreement with the study by Oh et al. reported 73% in the MSE group and 81% in the BAME group.[12] The skeletal gain in the BAME sample in this study was higher than 50% reported by Proffit; 40% by Kartalian,[18] and 55% reported by Garrett[19] that used conventional RPE in younger patients. Zong et al.[11] reported 59% skeletal contribution with MSE and Celenk-Koca et al.[15] reported 68% with BAME. The most probable reason the nature of the design of the appliance as bicortical engagement with longer implants offering greater skeletal anchorage by the MSE appliance.[14]
The pattern of midpalatal suture separation observed with both types of MARPE appliances in this study was found to be parallel in the axial view. The amount of suture opening at the C, PM1, PM2, and M1 differed from each other by no more than 0.5 mm. These results indicate that sutural expansion at the level of the palate was rather uniform anteroposteriorly, which agrees with the findings by the previous authors.[12,13,20] However, Lin et al.[21] demonstrated that MSO occurred in a triangular pattern superoinferiorly, with the least increase at the nasal floor and the greatest increase at the hard palate. These contrasting findings may be due to appliance activation, anteroposterior position of miniscrews placement in the maxilla, or ineffective expansion near zygomaxillary and nasomaxillary sutures.[11]
Buccal rotation or bending of the segments occurs throughout the arch. The amount is greater from posterior to anterior.[19] This rotation is most likely due to DT even with the BAME appliance which may also explain the angulation changes of the M1 and PM1.[9] This buccal rolling phenomenon had been expressed by the decrease of the external inclination angle of the M1 and PM1. This might be related to the force application away from the center of resistance of the anchoring units and to the outward rotational movement of the two palatal shelves.[4] There was no significant difference in the ABB between both MARPE groups. These findings coincided with those of Garib et al.[22] and Mosleh et al.[4]
Despite the fact that both types of MARPE appliances were skeletally anchored, buccal DT at the M1 and PM1 was found in both groups. The crown tipping can be due to the play between the miniscrew and the insertion slot of the miniscrew as reported by Carlson et al.[20] In other words, this might be related to the force application away from the center of resistance of the anchoring units and to the outward rotational movement of the two palatal shelves.[4] In the current study, tipping of posterior teeth in BAME group was significantly reduced compared with the MSE group which was consistent with previous MARPE studies.[4,12,14,15] Uprighting of the M1 and PM1 could be explained by the absence of a buccal force acting on the crowns and increased apical separation of the maxillary suture in the BAME group, leading to a more upright crown inclination relative to the nasal floor. Moreover, heavy stainless steel wires used in the final stages of comprehensive orthodontic treatment could introduce negative torque to the posterior teeth, restoring the ideal buccolingual inclinations of the teeth and possibly decreasing the amount of expansion previously gained by tipping of the posterior teeth buccally.[23]
Decreased BBT and bony dehiscence have been reported as a result of teeth moving through the buccal plate after expansion[15] ranging from 0.2 mm to 1.25 mm.[24,25] In the current study, the buccal bone reduction was significantly less in the BAME compared to the MSE group. Lee et al.[26] suggested that BAME may be better indicated for growing children whose palatal bones may exhibit less resistance than those in adults, technically eliminating the need for banding and additional laboratory work. To prevent these side effects on permanent teeth, miniscrew-supported appliances or appliances anchored to deciduous teeth were proposed as valid alternative protocols for rapid maxillary expansion.[25] However, a 6-month retention period was enough for the recovery of the buccal and lingual bone plates thickness.[17]
In addition, several finite element method (FEM) studies were performed on stress distribution with maxillary expanders suggested that a potential benefit for a clinician to use MARPE appliances could be in alleviating stress distribution on the buccal bone, parallel split of the palatine suture, and minimized tipping of the teeth.[27] Another FEM study found that the BAME did not show any possible side effects on the buccal plate, but the force transduction was very limited even within the midpalatal sutural area. By combining the conventional RPE and four miniscrews, in view of the displacement pattern, the MSE secured significant expansion of the anchor teeth to the buccal side with reduced tipping, compared to the conventional RPE. The teeth displacement was not remarkable with BAME. Conclusively, incorporation of four miniscrews was considered reasonable for even dissipation of the pressure along the suture and for the reduction of pressure on the buccal plate.[26]
The findings from this study suggest that the use of BAME resulted in greater skeletal effects and less dentoalveolar side effects including less DT and less buccal bone reduction compared to the use of MSE. Both types of MARPE can be a clinically acceptable, non-surgical treatment option for correcting mild-to-moderate maxillary transverse discrepancies in growing patients.
The current study was limited by the small sample size and the lack of short- and long-term follow-up. In addition, other treatment-related variabilities such as the expansion appliance design, activation protocol, methods of evaluating expansion effects, and biological variability may influence patient response to appliance therapy. Future studies should include a larger sample size and standardized treatment-related variability. Long-term follow-up evaluations of the sample should be conducted to gain an understanding of the stability of the skeletal, dentoalveolar, and periodontal effects for both types of MARPE.
CONCLUSION
Midpalatal suture separation can be obtained with both types of MARPE appliances in 100% of subjects in young adolescent patients
The pattern of midpalatal suture opening with MARPE appliances was parallel in the axial view
The attribution to TE with MSE appliances was 56% skeletal and 44% dentoalveolar, while with BAME group was 83% skeletal and 17% dentoalveolar
The DT was greater in the MSE compared to the BAME group 5. The buccal bone loss was greater in the MSE compared to BAME group.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137:830-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arch perimeter changes on rapid palatal expansion. Am J Orthod Dentofacial Orthop. 1990;97:194-9.
- [CrossRef] [Google Scholar]
- Editor's summary, Q and A, reviewer's critique In: Am J Orthod Dentofacial Orthop. Vol 134. 2008. p. :8-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of transverse changes during maxillary expansion with 4-point bone-borne and tooth-borne maxillary expanders. Am J Orthod Dentofacial Orthop. 2015;148:599-607.
- [CrossRef] [PubMed] [Google Scholar]
- Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Angle Orthod. 2006;76:156-63.
- [Google Scholar]
- Direct bone placement of the hyrax fixation screw for surgically assisted rapid palatal expansion (SARPE) J Oral Maxillofac Surg. 2006;64:1313-7.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional evaluation of surgically assisted implant bone-borne rapid maxillary expansion: A pilot study. Am J Orthod Dentofacial Orthop. 2007;131(Suppl 4):S92-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137:304.e1-12. discussion 304-5
- [CrossRef] [PubMed] [Google Scholar]
- Miniscrew-assisted rapid palatal expansion: A review of recent reports. J World Fed Orthod. 2020;9:S54-8.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal and dentoalveolar changes in the transverse dimension using microimplant-assisted rapid palatal expansion (MARPE) appliances. Semin Orthod. 2019;25:46-59.
- [CrossRef] [Google Scholar]
- Comparison of traditional RPE with two types of micro-implant assisted RPE: CBCT study. Semin Orthod. 2019;25:60-8.
- [CrossRef] [Google Scholar]
- Skeletal, dentoalveolar, and periodontal changes of skeletally matured patients with maxillary deficiency treated with microimplant-assisted rapid palatal expansion appliances: A pilot study. APOS Trends Orthod. 2018;8:71.
- [CrossRef] [Google Scholar]
- Skeletal and dentoalveolar changes after skeletal anchorage-assisted rapid palatal expansion in young adults: A Cone beam computed tomography study. APOS Trends Orthod. 2017;7:113-9.
- [CrossRef] [Google Scholar]
- Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: A prospective randomized clinical trial. Angle Orthod. 2018;88:702-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:53-62.
- [CrossRef] [PubMed] [Google Scholar]
- Bone-borne versus tooth-borne rapid palatal expansion (RPE) treatment in mixed dentition; literature review. Mod Res Dent. 2018;2:1-9.
- [CrossRef] [Google Scholar]
- Cone-beam computerized tomography evaluation of the maxillary dentoskeletal complex after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2010;138:486-92.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8-9.
- [CrossRef] [PubMed] [Google Scholar]
- Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am J Orthod Dentofacial Orthop. 2016;149:716-28.
- [CrossRef] [PubMed] [Google Scholar]
- Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253-62.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid maxillary expansion-tooth tissue-borne versus tooth-borne expanders: A computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548-57.
- [Google Scholar]
- A cone-beam computed tomography evaluation of buccal bone thickness following maxillary expansion. Imaging Sci Dent. 2013;43:85-90.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate and post-retention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod. 2008;79:24-9.
- [CrossRef] [PubMed] [Google Scholar]
- Buccal bone plate thickness after rapid maxillary expansion in mixed and permanent dentitions. Am J Orthod Dentofacial Orthop. 2019;155:198-206.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary transverse expansion in adults: Rationale, appliance design, and treatment outcomes. Semin Orthod. 2018;24:52-65.
- [CrossRef] [Google Scholar]
- The difference of stress distribution of maxillary expansion using rapid maxillary expander (RME) and maxillary skeletal expander (MSE)-a finite element analysis. Prog Orthod. 2018;19:33.
- [CrossRef] [PubMed] [Google Scholar]






