Translate this page into:
Comparison of twin block appliance and Forsus Fatigue Resistant Device therapies on uvulo-glossopharyngeal dimensions: A retrospective study

*Corresponding author: Mehmet Ali Yavan, Department of Orthodontics, Adiyaman University, Adiyaman, Turkey. yavanmehmetali@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yavan MA, Aycan M, Aksoyler D, Essiz A. Comparison of twin block appliance and Forsus Fatigue Resistant Device therapies on uvulo-glossopharyngeal dimensions: A retrospective study. APOS Trends Orthod 2021;11(1):23-31.
Abstract
Objectives:
The aim of this study was to compare the effects of two different functional appliances on skeletal, dental, and uvulo-glossopharyngeal dimensions.
Materials and Methods:
Pre- and post-treatment lateral cephalograms of 50 adolescent Class II patients with a retrognathic mandible were obtained from an archive and divided into two groups according to functional therapy. Twenty-five patients (14 females, 11 males, mean age: 13.5 ± 2.8) who were treated with Forsus Fatigue Resistant Device (FFRD) and 25 patients (17 females, eight males, mean age: 12.5 ± 0.4) who had received functional therapy through the twin block (TWB) were enrolled. Skeletal, dentoalveolar, tongue, uvula, hyoid position, and oropharyngeal airway parameters were measured using the Dolphin software, and uvulo-glossopharyngeal area measurements were performed with the AutoCAD software.
Results:
The TWB group exhibited remarkable mandibular advancement compared to the FFRD group (P < 0.05). Both of the treatments proclined mandibular incisors, and tongue dimensions increased significantly in both groups (P < 0.05). While the hyoid point moved forward and the oropharyngeal area increased significantly in the TWB group, no significant changes were observed in the FFRD group. The comparison of the TWB and FFRD groups with regard to uvulo-glossopharyngeal dimensions showed no significant differences between the groups (P > 0.05).
Conclusion:
Changes in uvulo-glossopharyngeal dimensions did not significantly vary between the two different functional therapies.
Keywords
Airway
Class II malocclusion
Forsus
Twin block
INTRODUCTION
Craniofacial anomalies, such as mandibular retrognathism, may cause diminution of the upper airway passage and narrower anteroposterior pharyngeal dimensions compared to healthy subjects.[1,2] This reduction in distance between the mandibular corpus and the cervical column may stimulate the posterior positioning of the tongue and uvula. Changes in these structures may cause obstructive sleep apnea (OSA).[3]
Numerous removable functional appliances were designed to correct this malocclusion by stimulating the growth of the mandible.[4,5] Studies that have investigated the effects of removable functional treatments on the pharyngeal airway passage (PAP) have reported significant increases in the dimensions of the upper airway in growing patients with Class II malocclusion.[6-9] However, there is no consensus on the effects of fixed functional appliances on upper airway dimensions. While some studies[10-12] have shown significant increases, Ozdemir et al.[13] report no significant changes in pharyngeal dimensions. Studies that have compared the effects of removable and fixed functional devices on airway dimensions have suggested that removable appliances are more efficient than fixed appliances in increasing pharyngeal airway dimensions.[8,14]
To the best of our knowledge, no comparison of the effects of the twin block (TWB, removable) and Forsus Fatigue Resistant Device (FFRD, fixed) functional therapies on hyoid, tongue, and uvula dimensions has yet been described. The aim of this retrospective study was to compare the effects of these appliances on skeletal, dental, and uvuloglossopharyngeal dimensions.
MATERIALS AND METHODS
Study design
This was a retrospective study conducted at the Department of Orthodontics, Faculty of Dentistry, Adiyaman University, Turkey; ethical approval for this study was received from the Adiyaman University Ethics Committee (Ethics Approval Number: 2019/8-6). The data consisted of pre- and post-treatment cephalometric radiographs of patients treated with FFRD and TWB.
Patients treated with FFRD and TWB in our clinic between 2012 and 2019 were identified, and those with the following criteria were included in the study; peak pubertal growth stage of 3–4 according to the cervical vertebrae maturational indicators (CVMI),[15] Skeletal Class II with mandibular retrognathia (SNB < 80), overjet ≥ 5 mm, Class II molar and canine relationship, no craniofacial deformities nor history of OSA or snoring, presence of good-quality lateral cephalograms, and in addition to the above criteria, the TWB group had the additional criterion of minimal or no crowding.
The sample size was calculated using GPOWER statistical software (Ver. 3.1 Franz Faul, Universität Kiel, Kiel, Germany), considering α = 0.05, power = 0.80, an effect size of 0.75 considering the mean treatment difference in middle airway space was 2.12 ± 1.81 mm in the removable functional appliance group and 0.85 ± 1.56 mm in the fixed functional appliance group derived from Jena et al.[14] The resultant sample size was 23 in each group thus 25 patients were enrolled in each group, which summed to a total of 50 patients.
Subjects treated with the same appliance [Figure 1] and the same protocol was included in the TWB group. A standard TWB appliance, as described by Clark,[16] was made, and the patients were told to use the appliances for 22 h. The construction of the device was the same for all individuals. A wax construction bite was created, through which the mandible was advanced in single step, forming a 2–4 mm vertical opening at the incisors and an edge-to-edge incisor position. Patient follow-up occurred monthly during the active treatment. The appliance was removed and the second cephalogram was taken when a Class 1 canine relationship was obtained and the cervical vertebral maturation index was CMVI Stage 5. The TWB group consisted of 25 patients (17 females, eight males, mean age: 12.5 ± 3.4), and the mean duration of treatment was 11 months.
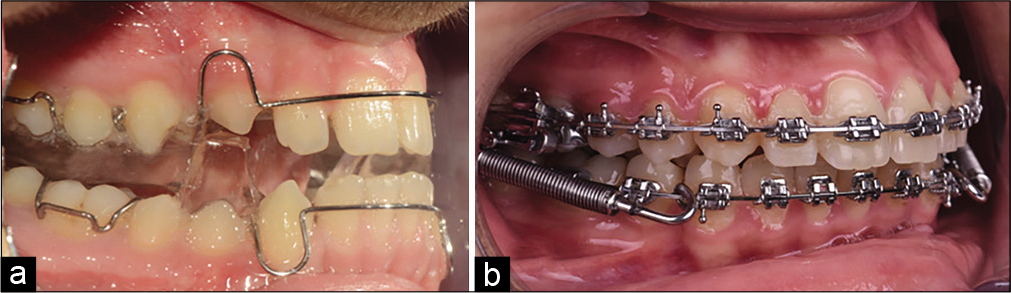
- Application of twin block (a) and Forsus Fatigue Resistant Device (b) appliances.
Individuals treated with the same procedure were included in the FFRD group [Figure 1]. Fixed appliances (MBT, 3M Unitek, St. Paul, MN, USA) with a 0.022 in slot were bonded to the upper and lower arches. Alignment continued until 0.019 × 0.025 inch stainless-steel arch wires were inserted passively. The FFRD was applied according to the manufacturer’s instructions (3M Unitek). Patient follow-up occurred monthly during the active treatment. The active phase proceeded until an edge-to-edge incisal relationship was achieved. On completion of the treatment period, a second cephalogram was obtained for each participant. The FRD group consisted of 25 patients (14 females, 11 males, mean age: 13.5 ± 2.8), and the mean duration of treatment was 8 months.
All cephalometric radiographs were taken with the same instrument under standard conditions (Planmeca EC Proline PM 2002), in centric occlusion according to the natural head position and after a usual swallow by the same technician. The distance between the film source and the beam source was 150 cm. The machine used has a power of 68–74 kW and 12 mA, and it is irradiated for 0.4–0.5 s. The magnification rate on radiographs is 1.1.
[Table 1] presents that the landmarks and planes were used. Six skeletal, four dental, and 12 uvulo-glossopharyngeal measurements [Figures 2 and 3] were digitized in the Dolphin Imagining 11.0 Software (Dolphin Imaging and Management Solutions, Chatsworth, Calif), and cross-sectional oropharyngeal, uvula and tongue areas [Figure 4] were measured with the AutoCAD 2012 software (AutoCAD, Autodesk, Inc, San Rafael, Calif).
| Variables | Definition |
|---|---|
| Landmarks | |
| S | The center of the sella turcica. |
| N | The nasion, the most anterosuperior point of the sutura nasofrontalis on the sagittal plane. |
| A | Point A, the deepest point of the concaveness of bone tissue, which is below the anterior nasal spina. |
| B | Point B, the deepest point of the concaveness of the mandibular alveolus. |
| ANS | Anterior nasal spina, the most anterior point of the spina nasalis anterior. |
| PNS | Posterior nasal spina, the most posterior point of the spina nasalis anterior. |
| U1 | The incisal edge of the maxillary incisor. |
| L1 | The incisal edge of the mandibular incisor. |
| Gn | The gnathion, the junction of the lover edge and the most anterior point of the mandible. |
| Me | The menton, the lowest point of the symphysis region on the sagittal plane. |
| Go | The gonion, the junction point of the outer borders of the ramus and the corpus of the mandible. |
| Co | The condylion, the most superior point of the condyler head. |
| E | The base of the epiglottis. |
| T | The tip of the tongue. |
| U | The tip of the uvula. |
| H | The most superior and anterior points on the body of the hyoid bone. |
| C3 | The antero-inferior limit of the third cervical vertebra. |
| Rgn | The most posterior point of the symphysis. |
| Planes | |
| Maxillary plane | A line joining the ANS and PNS points. |
| Mandibular plane | A line joining the Go and Gn points. |
| U1 plane | The axial inclination of the maxillary incisor. |
| L1 plane | The axial inclination of the mandibular incisor. |
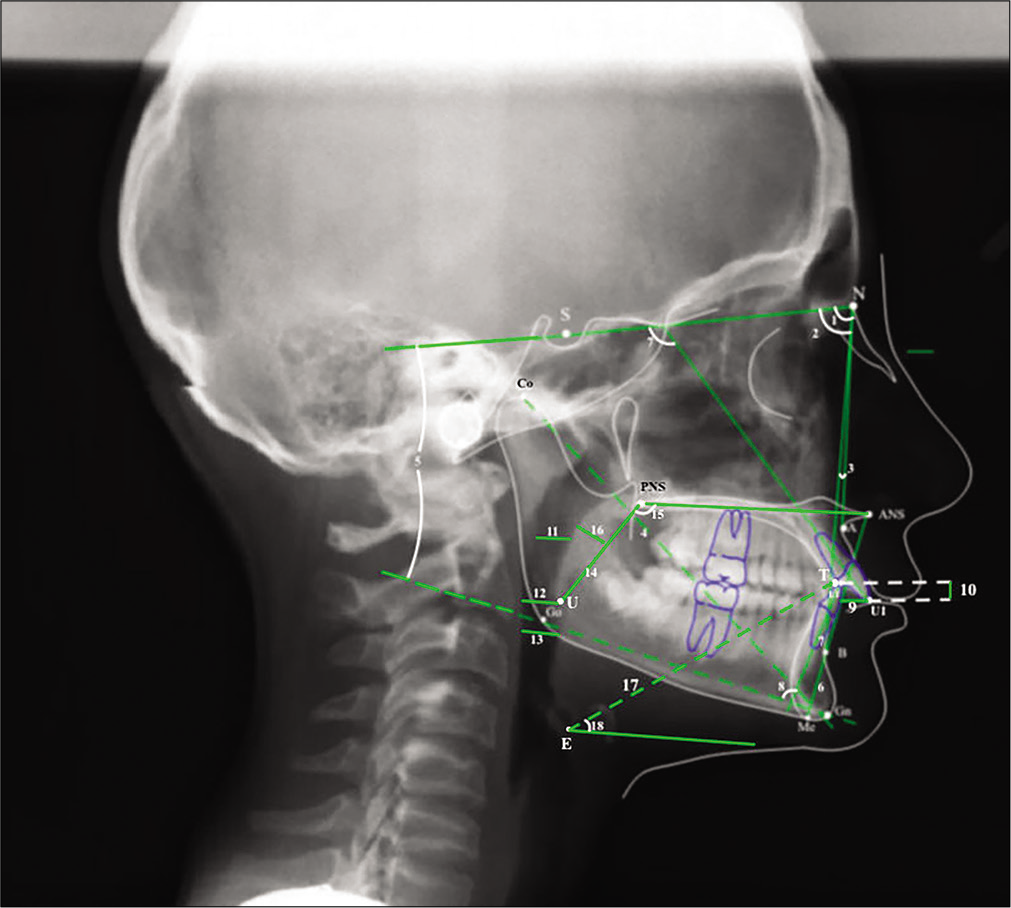
- Cephalometric angular and linear measurements used in the study. (1) SNA (°), angle formed by S-N and N-A planes, (2) SNB (°), angle formed by S-N and N-B planes, (3) ANB (°), angle formed by N-A and N-B planes, (4) Co-Gn (mm), the distance between Co and Gn points, (5) SN/GoGn (°), angle formed by S-N and Go-Gn planes, (6) ANS-Me (mm), the distance between ANS and Me points, (7) U1/ SN (°), angle formed by U1 plane and S-N planes, (8) IMPA (°), angle formed by L1 plane and Mandibular plane, (9) Overjet (mm), the horizontal distance between the buccal surface of the mandibular central incisor and the incisal tips of the maxillary central incisor, (10) Overbite (mm), the vertical distance between the incisal tips of the maxillary and mandibular central incisor, (11) SAS (Superior airway space) (mm), the distance of the midpoint of the line from PNS point to tip of uvula to the horizontal counterpart on the posterior pharyngeal wall along the parallel line to maxillar plane, (12) MAS (Middle airway space) (mm), the distance between U point and the horizontal counterpart on the posterior pharyngeal wall along the parallel line to maxillary plane, (13) IAS (Inferior airway space) (mm), the distance between intersection of mandible and tongue and the horizontal counterpart on the posterior pharyngeal wall along the parallel line to maxillary plane, (14) Uvula length (mm), the distance between PNS and U points, (15) Uvula angle (°), angle formed by maxillary plane and PNS-U plane, (16) Uvula thickness (mm), maximum thickness of the uvula, (17) Tongue length (°), the distance between E and T points, (18) Tongue angle (°), angle formed by E-T plane and the parallel line to maxillary plane.
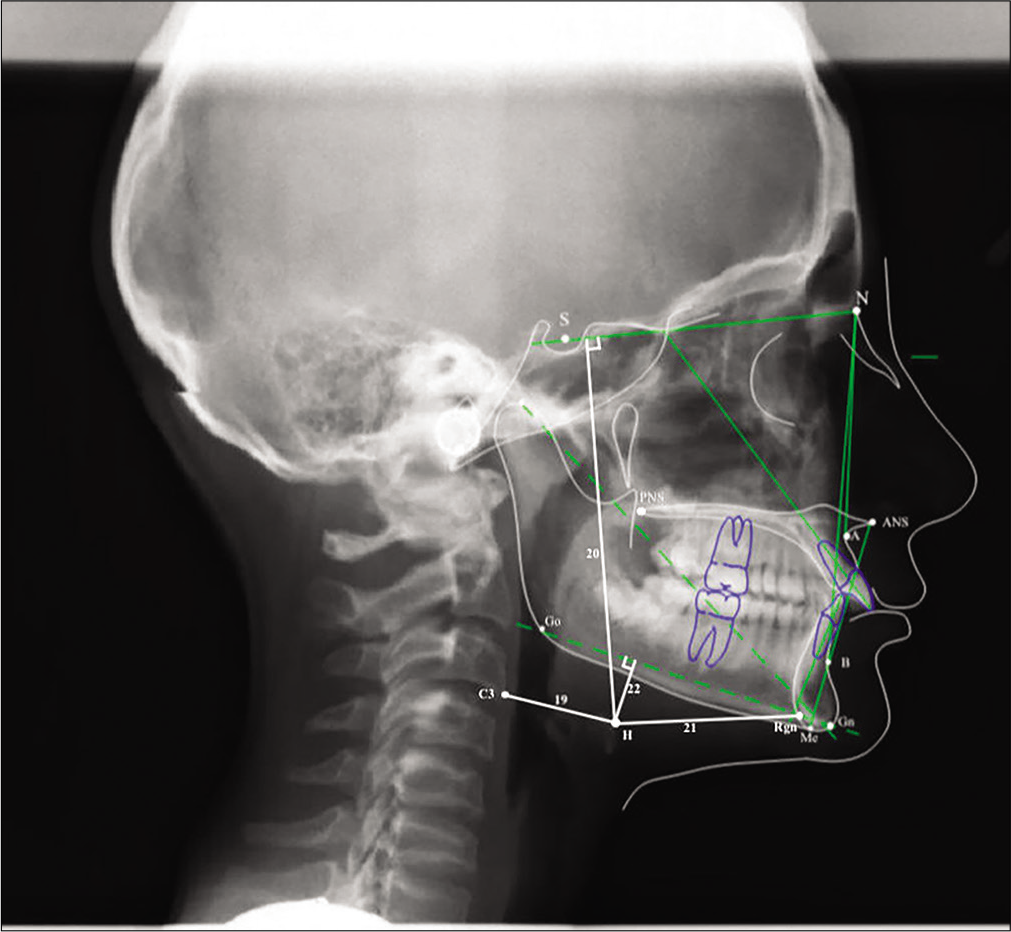
- Cephalometric angular and linear measurements used in the study (Continued): 19: H-C3 (mm), the distance between H and C3 points; 20: H-SN (mm), the perpendicular distance from H point to SN plane; 21: H-Rgn (mm), the distance between H and Rgn points, 22: H-MP (mm), the perpendicular distance from MP to H point.
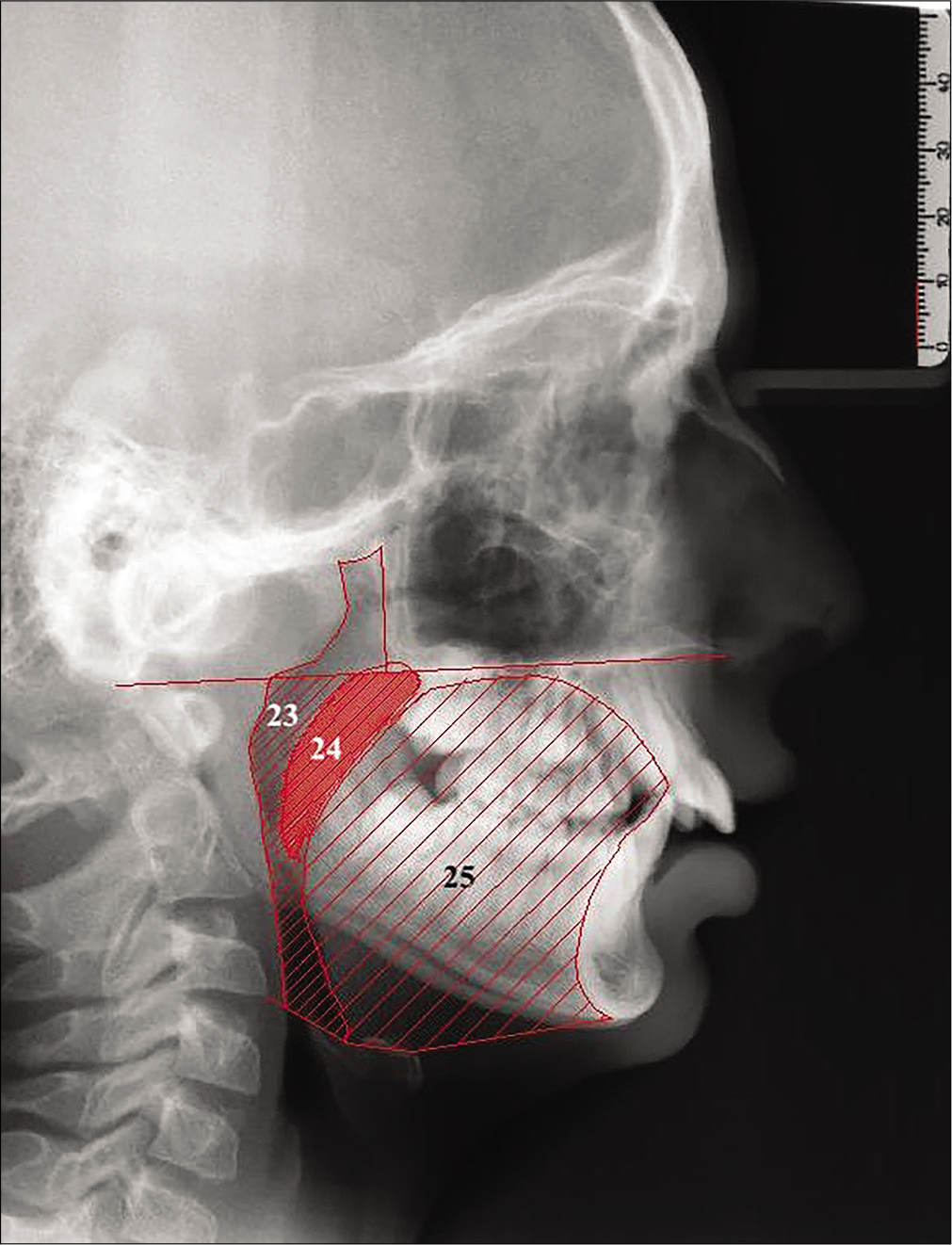
- Area measurements of the study: 23: Oropharyngeal area (mm2), an area limited superiorly by a backward extension of the maxillary plane and inferiorly by a line joining E and C3 points; 24: Uvula area (mm2), an area formed by outer boundaries of uvula and limited superiorly by maxillary plane, 25: Tongue area (mm2), an area surrounded posteriorly by the oropharynx and uvula, superiorly by the maxillary plane, anteriorly by the lingual aspects of the anterior teeth and lingual mandibular symphyseal contour and inferiorly by the line extending from the point E to the point H and the line joining H and Me points.
Twenty randomly selected cephalometric radiographs were redigitized and redrawn, and cephalometric and area measurements were repeated after 10 days. Method error coefficients were calculated and found to be within acceptable limits (range, 0.95–0.99).
Statistics
The normality of the distribution of continuous variables was tested using the Shapiro-Wilk test. A paired t-test was used to compare the cephalometric variable at baseline and to compare the changes within the groups with normal distribution, but the Wilcoxon test was preferred when the distribution was not normal. The mean differences among the groups were compared by Student t-test. Descriptive statistic parameters were presented as mean ± standard deviation (mean ± SD). Statistical analysis was performed with SPSS (SPSS version 22.0, SPSS, IBM, Armonk, NY, USA) and P < 0.05 was accepted as statistically significant.
RESULTS
There was no significant difference in the pre-treatment variables between the two groups [Table 2]. Comparisons of the changes within each group and comparisons of the mean differences between the groups are presented in [Table 3].
| TWB group | FFRD group | Overall P value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (years) | 12.40 | 1.51 | 13.47 | 1.84 | 0.187 |
| Skeletal measurements | |||||
| 1. SNA (°) | 81.55 | 3.38 | 81.66 | 4.75 | 0.347 |
| 2. SNB (°) | 74.55 | 3.30 | 76.36 | 3.90 | 0.970 |
| 3. ANB (°) | 6.99 | 2.26 | 5.30 | 2.03 | 0.846 |
| 4. Co-Gn (mm) | 102.64 | 5.85 | 102.76 | 7.29 | 0.242 |
| 5. SN/GoGn(°) | 32.22 | 6.15 | 31.33 | 5.99 | 0.975 |
| 6. ANS-Me (mm) | 56.42 | 4.56 | 55.92 | 5.42 | 0.606 |
| Dental measurements | |||||
| 7. U1/SN (°) | 103.36 | 5.66 | 103.86 | 7.03 | 0.234 |
| 8. IMPA (°) | 96.05 | 6.88 | 91.20 | 7.30 | 0.747 |
| 9. Overjet (mm) | 6.40 | 2.14 | 6.03 | 1.84 | 0.429 |
| 10. Overbite (mm) | 3.07 | 2.22 | 3.16 | 2.16 | 0.996 |
| Pharyngeal airway measurements | |||||
| 11. SAS (mm) | 11.12 | 3.26 | 10.69 | 3.57 | 0.441 |
| 12. MAS (mm) | 0.60 | 0.37 | 1.76 | 3.80 | 0.921 |
| 13. IAS (mm) | 9.58 | 2.15 | 8.41 | 2.82 | 0.163 |
| Uvula Measurements | |||||
| 14. Uvula length (mm) | 30.54 | 3.89 | 31.10 | 4.03 | 0.618 |
| 15. Uvula angle (°) | 130.82 | 7.01 | 127.66 | 6.60 | 0.367 |
| 16. Uvula thickness (mm) | 7.84 | 1.52 | 8.05 | 1.11 | 0.135 |
| Tongue measurements | |||||
| 17. Tongue length (mm) | 63.68 | 5.88 | 64.00 | 4.74 | 0.410 |
| 18. Tongue angle (°) | 27.61 | 5.93 | 29.45 | 5.40 | 0.090 |
| Hyoid measurements | |||||
| 19. H-C3 (mm) | 29.01 | 4.44 | 30.88 | 5.39 | 0.139 |
| 20. H-SN (mm) | 92.66 | 8.28 | 98.30 | 10.26 | 0.897 |
| 21. H-RGN (mm) | 30.76 | 5.27 | 32.59 | 7.06 | 0.420 |
| 22. H-MP (mm) | 12.63 | 5.25 | 16.78 | 6.57 | 0.289 |
| Area measurements | |||||
| 23. Oropharynx (mm2) | 5.08 | 1.47 | 4.82 | 1.25 | 0.352 |
| 24. Uvula (mm2) | 1.48 | 0.45 | 2.80 | 4.88 | 0.214 |
| 25. Tongue (mm2) | 25.86 | 3.32 | 27.29 | 3.65 | 0.241 |
TWB: Twin block, FFRD: Forsus Fatigue Resistant Device, SD: Standard deviation, mm: Millimeter
| TWB group | FFRD group | TWB versus FFRD Pvalue | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | P | ||
| Skeletal measurements | |||||||
| 1. SNA (°) | –0.65 | 2.77 | 0.383NS | –1.22 | 1.59 | 0.012* | 0.208NS |
| 2. SNB (°) | 1.30 | 2.31 | 0.005** | 0.06 | 1.38 | 0.974NS | 0.045* |
| 3. ANB (°) | –1.80 | 2.21 | 0.000*** | –1.28 | 1.70 | 0.005** | 0.499NS |
| 4. Co-Gn (mm) | 3.72 | 3.20 | 0.000*** | 2.60 | 3.55 | 0.015* | 0.998NS |
| 5. SN/GoGn (°) | –0.91 | 4.73 | 0.501NS | 0.70 | 2.49 | 0.201NS | 0.093NS |
| 6. ANS-Me (mm) | 5.06 | 4.47 | 0.000*** | 5.08 | 3.76 | 0.000*** | 0.557NS |
| Dental measurements | |||||||
| 7. U1/SN (°) | 1.28 | 6.99 | 0.696NS | 0.02 | 9.94 | 0.896NS | 0.768NS |
| 8. IMPA (°) | 5.34 | 6.05 | 0.000*** | 5.88 | 7.73 | 0.009** | 0.091NS |
| 9. Overjet (mm) | –2.79 | 2.41 | 0.000*** | –2.92 | 2.15 | 0.000*** | 0.603NS |
| 10. Overbite (mm) | –1.29 | 2.28 | 0.003** | –1.68 | 2.27 | 0.012* | 0.553NS |
| Pharyngeal airway measurements | |||||||
| 11. SAS (mm) | 2.40 | 2.37 | 0.000*** | 2.46 | 2.18 | 0.001*** | 0.450NS |
| 12. MAS (mm) | 0.03 | 0.57 | 0.728NS | –0.13 | 2.84 | 0.900NS | 0.748NS |
| 13. IAS (mm) | 1.56 | 3.57 | 0.05* | 0.50 | 2.99 | 0.223NS | 0.237NS |
| Uvula measurements | |||||||
| 14. Uvula length (mm) | 0.98 | 5.17 | 0.253NS | 1.99 | 3.44 | 0.098NS | 0.523NS |
| 15. Uvula inclination (°) | –1.48 | 2.14 | 0.015* | –1.12 | 3.16 | 0.05* | 0.292NS |
| 16. Uvula thickness (mm) | 0.30 | 1.97 | 0.539NS | 0.87 | 1.86 | 0.084NS | 0.728NS |
| Tongue measurements | |||||||
| 17. Tongue length (mm) | 6.01 | 9.07 | 0.001*** | 4.28 | 6.57 | 0.012* | 0.675NS |
| 18. Tongue inclination (°) | –4.33 | 6.09 | 0.012* | –4.20 | 6.56 | 0.014* | 0.914NS |
| Hyoid measurements | |||||||
| 19. H-C3 (mm) | 3.24 | 4.70 | 0.004** | 1.61 | 3.78 | 0.127NS | 0.406NS |
| 20. H-SN (mm) | 6.19 | 7.21 | 0.000*** | 5.92 | 7.06 | 0.002** | 0.715NS |
| 21. H-RGN (mm) | 3.87 | 6.22 | 0.002** | 2.17 | 6.12 | 0.223NS | 0,263NS |
| 22. H-MP (mm) | 1.00 | 3.28 | 0.193 | 0.75 | 3.63 | 0.306NS | 0.820NS |
| Area measurements | |||||||
| 23. Oropharynx (mm2) | 0.77 | 1.58 | 0.021* | 0.43 | 1.75 | 0.554NS | 0.110NS |
| 24. Uvula (mm2) | 0.08 | 0.37 | 0.221NS | 0.19 | 0.26 | 0.154NS | 0.249NS |
| 25. Tongue (mm2) | 3.36 | 2.45 | 0.000*** | 2.34 | 2.62 | 0.003** | 0.656NS |
TWB: Twin block, FFRD: Forsus Fatigue Resistant Device, SD: Standard deviation, mm: Millimeter, NS: Not significant, *: P<0.05, **: P<0.01, ***: P<0.001
Cephalometric results showed that ANB, representing the skeletal maxillomandibular relationship, was decreased significantly in the TWB group (P < 0.001). The overjet and the overbite reduction were significant at the end of the treatment in both groups. While significant mandibular protraction (in SNB by 1.30 ± 2.31) was observed in the TWB group (P < 0.05), and significant maxillary inhibition (in SNA by −1.22 ± 1.59) was found in the FFRD group (P < 0.05).
There were significant increments in lower face length (ANS-Me, P < 0.001), and the mandibular incisors showed significant proclination in the groups (P < 0.01). However, the inclination of the maxillary incisors did not change significantly in either group (P > 0.05).
Tongue length and area increased and inclination decreased significantly (P < 0.05) in both groups. Inferior airway space increased significantly in the TWB group (P < 0.05), but no significant change was observed in the FFRD group (P > 0.05). Superior airway space increased in both treatment groups (P < 0.001). Oropharyngeal area increased significantly in the TWB group (P < 0.05), but no significant change was found in the FFRD group (P > 0.05).
Hyoid position showed significant forward and downward movement in the TWB group (P < 0.05). Uvula length, thickness, and area did not change significantly (P > 0.05) in either group. However, significant decreases were observed in the uvula inclinations in both groups (P < 0.05).
When changes in uvula, tongue, oropharyngeal, and dentoalveolar measurements were compared, no statistically significant differences were found between the groups (P > 0.05).
DISCUSSION
Intraoral findings of mandibular retrognathia are not limited to dental Class II malocclusion. This anomaly causes a more backward tongue position in relation to the uvula and leads to a narrower PAP.[17] There is a consensus in the literature about the beneficial effects of removable functional orthopedic devices on PAP.[6,14,18-21] However, the effects of fixed functional appliances on PAP are controversial.[11,13] Alhammadi et al.[8] compared removable (TWB) and fixed (FFRD) functional devices on dentoskeletal and PAP dimensions with cone-beam computed tomography (CBCT) and reported that TWB showed more evident skeletal effects and that changes in PAP dimensions were more obvious compared to FFRD therapy. However, there is limited knowledge about their effects on hyoid, uvula, and tongue dimensions and positions. Therefore, this study aimed to compare two different functional treatment approaches on the dentoskeletal and uvulo-glossopharyngeal structures in terms of cephalometric aspects.
There are concerns in the literature on the evaluation of three-dimensional pharyngeal structures with two-dimensional cephalograms.[22-24] Evaluation of pharyngeal structures with three-dimensional imaging, such as CBCT, can give precise outcomes.[8,25,26] However, relatively high radiation doses and limited accessibility restricts the use of this method. Therefore, evaluation was conducted with lateral cephalograms in this study.
While all subjects of the groups were in the growth period at the beginning of the therapies, TWB effectively moved the mandible anteriorly compared to FFRD therapy. Differences in anchorage designs and the replacement of condyle with TWB may have led to this outcome. Previous researches comparing TWB and FFRD reported similar findings.[8,27] FFRD restrained the maxilla with a significant decrease in SNA° (−1.22°). However, no significant difference was found in the change of SNA with TWB treatment. This finding is in accordance with Giuntini et al.[27] while in contrast with Alhammadi et al.[8] This difference could be attributed to the differences in age groups and treatment durations. Both treatments showed similar effects on the vertical skeletal dimensions. These treatments did not cause any significant rotation of the mandible, and this finding was in accordance with the literature.[8,11,27]
Dental changes were similar between TWB and FFRD. Both treatments proclined lower incisors and decreased overjet and overbite significantly, in accordance with the literature.[8,11,13,27]
Functional treatments may induce the anterior relocation of the mandible, and the morphology of the upper airway may be influenced by this repositioning, such as anterior traction of the hyoid bone and forward repositioning of the tongue. These movements lead to moving the tongue away from the uvula and consequently increase the dimensions of the pharyngeal airway.[14] Both treatment groups showed significant downward movements of the hyoid bone; however, in the TWB group, the hyoid bone also moved forward significantly. In the literature, Lin et al. researched the effects of removable functional treatments on hyoid position and found significant anterior movement with a modified Bionator, in accordance with our findings.[20] There was anterior movement in the FFRD treatment as well, but this change was not statistically significant. This finding appears to be compatible with Ozdemir et al.[13] but in contrast with Bavbek et al.[11] who found significant forward shifting in the hyoid bone with FFRD treatment. The discrepancies in these outcomes may be related to the differences in mean treatment times and the amount of mesial movements of the mandibular teeth.
Both treatments exhibited significant increases in tongue dimensions, and significant decreases in inclinations were observed, which may be due to the downward and forward displacement of the tongue tip. Mesial movements of the mandibular arch may lead to broadening the chamber of the tongue, resulting in these outcomes. Yassaei et al.[18] found a significant increase in tongue length after treatment with a Farmand functional appliance, and Ozdemir et al.[13] reported a significant increment in tongue area after FFRD treatment, in accordance with our study.
Both treatments caused a significant reduction in the inclination of the uvula. Recent studies evaluating the effects of TWB on the uvula reported outcomes compatible with our study. Jena et al.[14] suggested that functional treatment with TWB reduces the pressure of the tongue on the uvula and leads to significant changes in uvula length, thickness, and inclination. Ghodke et al.[9] reported a significant decrease in the inclination of the uvula but no significant changes in thickness and length. Only one study investigating the effect of FFRD on the uvula was found in the literature: Ozdemir et al.[13] reported that uvula area did not change significantly after FFRD treatment, in contrast to our study. The lesser widening of the tongue area as compared to our study may be responsible for this difference.
Following adaptive changes in the tongue and uvula, a significant increase occurred in the oropharyngeal area (0.77 ± 1.58) in the TWB group. Recent TWB studies reported significant improvements in PAP dimensions.[8,9,14] Jena et al.[14] and Ghodke et al.[9] indicated significant increments (2.12 mm and 1.54 mm, respectively) in PAP, in accordance with the present study. Alhammadi et al.[8] also reported a significant increase in oropharyngeal volume in the TWB group, ascertained through 3D analysis. However, no significant changes were observed in the FFRD group. A literature review revealed controversial outcomes of FFRD on oropharyngeal dimensions. While Bavbek et al.[11] found significant increases in the FFRD group, Ozdemir et al.[13] showed no significant differences in oropharyngeal area in the FFRD group, in accordance with our study. Bavbek et al.[11] suggested that proclination of the lower incisors and medicalization of the molars may create more space for the tongue and change its posture, subsequently leading to an increase in passage dimensions. However, Ozdemir et al.[13] proposed that dentoskeletal changes with FFRD may not be enough to affect PAP dimensions. Differences between treatment durations, age groups, and level of skeletal maturation may result in these discrepancies.
Comparison of the changes in uvulo-glossopharyngeal measurements between the groups revealed that there are no significant differences between TWB and FFRD treatments. Only the changes in SNB° were statistically different between the groups, and no significant differences were found in the other skeletal and dental parameters. It appears that a significant 1.3° displacement of the mandible in the TWB group was not sufficient to make a significant difference between the uvulo-glossopharyngeal parameters of the two treatments. In the literature, studies comparing removable and fixed functional appliances on PAP morphology are limited. Jena et al.[14] compared TWB and mandibular Protraction-IV appliances and reported that improvements with the TWB appliance were significantly greater than those with MPA-IV. Alhammadi et al.[8] compared the effects of TWB and FFRD appliances and indicated that TWB was more efficient than FFRD in the increase of PAP volume. Our findings are not compatible with these researches. Different age groups, treatment durations, activation protocols, and amounts of tooth movement may be responsible for the different effects on PAP dimensions.
The first limitation of this study was the lack of a control group with mandibular retrognathy with which to compare growth changes. However, ethically, exposing participants to radiation without treatment for an average duration of 9 months are unacceptable. This study also showed the short-term effects of functional appliances on uvulo-glossopharyngeal structures with two-dimensional lateral cephalograms. While typical orthodontic imaging techniques, including CBCT, are often limited in the assessment of OSA,[28] future studies should use three-dimensional imaging techniques to achieve more accurate results in the assessment of craniofacial structures. Research should also be designed to include long-term changes to detect relapses over time and involves different ages and sexes, a greater sample size, and other functional appliances.
CONCLUSION
The outcomes of this study demonstrated that while significant mandibular protraction and increases in oropharyngeal area were observed with TWB therapy, no significant differences were observed in the changes of uvuloglossopharyngeal measurements between TWB and FFRD treatments in the short-term treatment effects.
Acknowledgments
The authors thank Miss Ebru Dumlupinar for her kind assistance with the statistical analyses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod. 2010;80:1061-7.
- [CrossRef] [PubMed] [Google Scholar]
- Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns. Am J Orthod Dentofacial Orthop. 2006;130:742-5.
- [CrossRef] [PubMed] [Google Scholar]
- Natural head posture, upper airway morphology and obstructive sleep apnoea severity in adults. Eur J Orthod. 1998;20:133-43.
- [CrossRef] [PubMed] [Google Scholar]
- Dentoskeletal effects of twin block and herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod. 2013;36:164-72.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment effects of the twin block appliance: A cephalometric study. Am J Orthod Dentofacial Orthop. 1998;114:15-24.
- [CrossRef] [Google Scholar]
- Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327-36.
- [Google Scholar]
- Changes in upper airway width associated with Class II treatments (headgear vs activator) and different growth patterns. Angle Orthod. 2011;81:440-6.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional skeletal and pharyngeal airway changes following therapy with functional appliances in growing skeletal Class II malocclusion patients. J Orofac Orthop. 2019;80:254-65.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of twin-block appliance on the anatomy of pharyngeal airway passage (PAP) in Class II malocclusion subjects. Prog Orthod. 2014;15:68.
- [CrossRef] [PubMed] [Google Scholar]
- Upper airway changes after Xbow appliance therapy evaluated with cone beam computed tomography. Angle Orthod. 2013;84:693-700.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in airway dimensions and hyoid bone position following Class II correction with forsus fatigue resistant device. Clin Oral Investig. 2016;20:1747-55.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the upper airway dimensions following herbst appliance treatment in adolescents: A retrospective study. APOS Trends Orthod. 2020;10:153-63.
- [CrossRef] [Google Scholar]
- Effects of fixed functional therapy on tongue and hyoid positions and posterior airway. Angle Orthod. 2013;84:260-4.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of twin-block and mandibular protraction appliance-IV in the improvement of pharyngeal airway passage dimensions in Class II malocclusion subjects with a retrognathic mandible. Angle Orthod. 2012;83:728-34.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment timing for twin-block therapy. Am J Orthod Dentofacial Orthop. 2000;118:159-70.
- [CrossRef] [PubMed] [Google Scholar]
- A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg. 2008;37:228-31.
- [CrossRef] [PubMed] [Google Scholar]
- Changes of tongue position and oropharynx following treatment with functional appliance. J Clin Pediatr Dent. 2007;31:287-90.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term changes in pharyngeal airway dimensions following activator-headgear and fixed appliance treatment. Eur J Orthod. 2008;30:598-605.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in the pharyngeal airway and position of the hyoid bone after treatment with a modified bionator in growing patients with retrognathia. J Exp Clin Med. 2011;3:93-8.
- [CrossRef] [Google Scholar]
- Oropharyngeal airway dimensions after treatment with functional appliances in Class II retrognathic children. J Oral Rehabil. 2011;38:588-94.
- [CrossRef] [PubMed] [Google Scholar]
- Cephalometric analysis in patients with obstructive sleep apnea Part I: Diagnostic value. J Orofac Orthop. 2002;63:143-53.
- [CrossRef] [Google Scholar]
- Frontal and lateral cephalometry in patients with sleep-disordered breathing. Laryngoscope. 2001;111:634-41.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of lateral cephalometric radiographs in the assessment of the upper airway in children: A retrospective study. Angle Orthod. 2020;90:47-55.
- [CrossRef] [PubMed] [Google Scholar]
- Pharyngeal airway volume and shape from cone-beam computed tomography: Relationship to facial morphology. Am J Orthod Dentofacial Orthop. 2009;136:805-14.
- [CrossRef] [PubMed] [Google Scholar]
- Cephalometric and computed tomographic predictors of obstructive sleep apnea severity. Am J Orthod Dentofacial Orthop. 1995;107:589-95.
- [CrossRef] [Google Scholar]
- Treatment effects produced by the twin-block appliance vs the forsus fatigue resistant device in growing Class II patients. Angle Orthod. 2015;85:784-9.
- [CrossRef] [PubMed] [Google Scholar]
- Obstructive sleep apnea and orthodontics: An American association of orthodontists white paper. Am J Orthod Dentofacial Orthop. 2019;156(13):28-e11.
- [CrossRef] [PubMed] [Google Scholar]






