Translate this page into:
Correction of severe facial asymmetry: A case with fractured condyle

*Corresponding author: Dr. Bhagyashree B. Desai, Department of Orthodontics and Dentofacial Orthopaedics, AMC Dental College and Hospital, Bhalakia Mill Compound, Opposite Anupam Cinema, Khokhra, Ahmedabad - 380 008, Gujarat, India. bhagyashree1@live.com
-
Received: ,
Accepted: ,
Abstract
The current paper depicts the challenges faced during the treatment of a complicated case of mandibular condylar head fracture, facial asymmetry, and centric relation-centric occlusion (CR-CO) discrepancy along with Class III malocclusion. A 20-year-old female reported with the chief complaint of difficulty in chewing and concern with her appearance due to deviated jaw and had a history of trauma over chin region. The clinical and radiographic examination revealed significant facial asymmetry with long face, right-sided deviation of the mandible, fractured condyle, CR-CO discrepancy, cross- bite with Class III malocclusion, and a missing mandibular single incisor along with non-vital 21 and 22. She was treated with 0.022 MBT appliance along with guiding plane for CR-CO correction followed by asymmetric bilateral sagittal split osteotomy and differential set back on the right and left sides and finally rigid fixation. A good facial profile and functional occlusion were achieved and non-vital 21 and 22 were esthetically rehabilitated with PFM crowns. The stability of surgical as well as orthodontic corrections was excellent and appreciable in the records obtained 2-year post-treatment. When faced with mutilated malocclusion, with multiple problems, sequential correction of functional malocclusion with dental decompensation followed by skeletal correction with surgical approach has yielded a appreciable facial correction with good stability showing 2-year post-treatment follow-up.
Keywords
Angle’s class iii malocclusion
Condylar fracture
Facial asymmetry
Orthognathic surgery
INTRODUCTION
Symmetry is considered as a hallmark of facial attractiveness.[1] Perfect bilateral face and body symmetry are largely a theoretical concept that seldom exists in living organisms.[2] The cause of asymmetry can be multivariate, dental, functional, skeletal, muscular, or combination of any of the above. The problem may originate from abnormal dental eruption, premature loss of primary or permanent teeth, trauma, or asymmetrical maxilla or mandible. According to Severt and Proffit,[3] the frequencies of facial laterality are 5%, 36%, and 74% in the upper, middle, and lower thirds of the face, respectively.
The prevalence of asymmetry is common, and its nature and cause might differ in various populations. The total facial structures were found to be larger on the right side than on the left. The attributing cause could be unilateral chewing.[4,5]
Diagnosis of transverse discrepancy should be accomplished by a thorough clinical examination and analysis of records including patients’ age[6] so as to determine the dental, skeletal, functional, or soft- tissue component. The first step should be checking of centric relation (CR) with centric occlusion (CO). Keeping these factors as well as the nature and severity of the transverse problems in mind, surgical approach along with fixed mechanotherapy can be used to address the skeletal problems to fine tune the occlusion on corrected bases and to obtain harmonious facial proportions.
This article illustrates a challenging case of mandibular asymmetry with fractured condyle, boasting beauty of diverse orthognathic protocol.
CASE REPORT
Etiology and diagnosis
A 20-year-old female reported with the chief complaints of irregular teeth, difficulty in chewing, and concern with her appearance due to deviated lower jaw. She had a history of trauma over the chin region due to fall, about 6 years ago, and was treated by a plastic surgeon, but the patient lacked essential records pertaining to the same. She had undergone unsuccessful orthodontic treatment attempt for 4 years.
Clinical findings
From a frontal view, the patient presented with the long face and increased lower facial height, significant facial asymmetry, and apparent mandibular deviation toward the right side by 5–6 mm while deviation of the nose toward the left side making the asymmetry appear worse [Figure 1]. She had reduced incisor display and asymmetrical lower lip line. The maxillary dental midline was coincident with the Cupid’s bow.
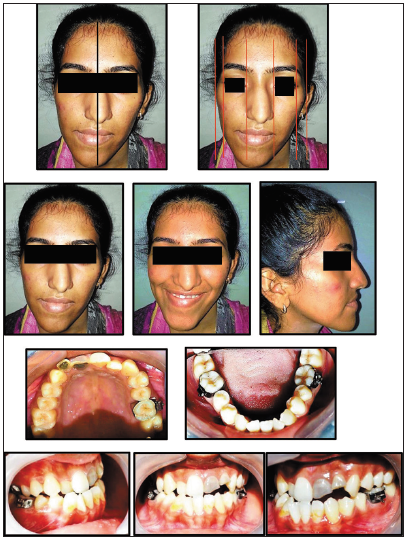
- A 20-year-old female with significant mandibular asymmetry and skeletal Class III malocclusion before treatment.
In the sagittal view, the patient had concavity of hard tissues due to a prognathic mandible with straight soft-tissue profile.
Intraoral examination revealed Angle’s Class III malocclusion, evident CR-CO discrepancy, and the presence of fractured, non-vital, and discolored but root canal treated 21 and 22. Single mandibular incisor was missing which might have been removed during previous treatment attempt with compensatory retroclination of the mandibular incisors. The anterior and unilateral posterior crossbite was noted in the right premolar and molar region.
Significant mandibular deviation on the right side was evident during opening and closing movements. Right condylar palpation was difficult. Orthopantomogram and lateral and posteroanterior (PA) cephalometric analysis confirmed the clinical findings; Class III skeletal bases, completed maturation of skeletal growth indicators, and true skeletal asymmetry with CR-CO discrepancy due to the absent condyle. On panoramic examination, the right condyle was absent, and only mandibular right third molar was present while the rest, all 3rd molar buds and a single mandibular incisor were missing [Figure 2a]. CT scan was done to confirm the status of missing condyle, and it was found that the condyle was fractured and was displaced medially to ramus and a fibrous joint was formed; the cause of which was past traumatic injury [Figure 2b].
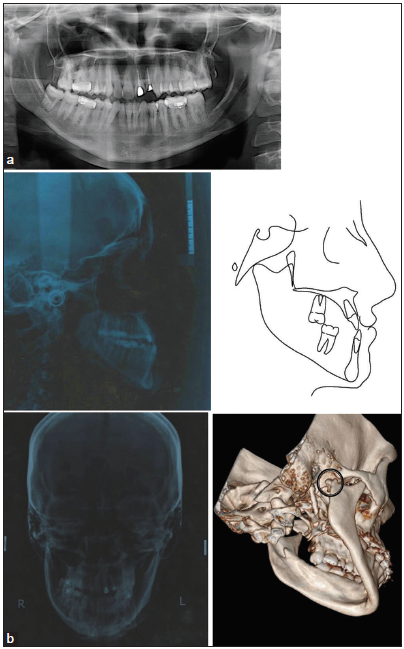
- Pre-treatment radiographs (a) Orthopantomogram and lateral cephalogram with pre-treatment tracing of lateral cephalogram. (b) Pre- treatment posteroanterior cephalogram; three-dimensional computed tomography scan showing fractured and displaced condylar head on the right side.
Treatment objectives
The prime objective of the treatment was to correct facial asymmetry and CR-CO discrepancy. A secondary objective was the attainment of a functional occlusion with ideal over-jet and overbite, elimination of dental compensations by aligning and leveling the arches, and correction of cross-bite and chin plane cant, which was planned to be followed by corrective rhinoplasty.
Treatment alternatives
The pendulum of the decision was swinging between bilateral sagittal split osteotomy (BSSO) with condylar reconstruction or only asymmetrical BSSO due to the presence of fractured condyle. After thorough cephalometric analysis, prediction tracing, and discussion with maxillofacial surgeon, the final treatment plan was zeroed down to the mandibular guiding plate along with fixed appliance therapy for CR-CO correction followed by asymmetrical BSSO to be followed at later stage by correction rhinoplasty. Knowing the asymmetry in lateral pterygoid, naturally formed fibrous functional joint and condyle were planned to be left undisturbed.
In the presented case, fractured condylar head was found to be displaced behind the posterior ramal border which required an arduous dissection for reconstructing the condyle and prognosis regarding reattachment was not assuring. In addition, there was a functional soft-tissue joint formed naturally. Due to a long standing fracture and retrival surgery would not have beniffited the condition; it was accepted as it was.
Treatment progress
To achieve alignment and leveling of arches, 0.022 × 0.028” slot MBT prescription brackets were bonded, and archwire sequence starting with thermal 0.016” NiTi and progressing until 0.019 × 0.025” SS was followed, which took around 9 months. The 3rd molar was extracted so as to have a sufficient healing period before the surgery [Figure 3].
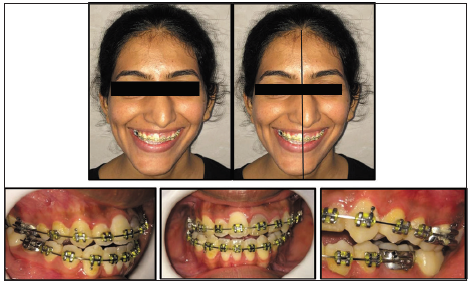
- 0.022” slot MBT prescription brackets and maxillary and mandibular 0.019 × 0.025” SS archwires in place.
To correct the evident CR-CO discrepancy and for deprogramming mandibular muscles, the guiding plate was fabricated and delivered with prosthodontic consultation. Acceptable results were achieved in 4 months with improvement in mandibular deviation [Figure 4].

- (a) Maxillary and mandibular arches prepared for surgery and correction achieved with guiding plate. (b) Radiographs showing the pre- surgical condition.
Asymmetrical BSSO with differential set back on left and right sides was performed to achieve functional occlusions and correct jaw base relation while matching the mandibular skeletal midline with the facial midline, followed by rigid fixation [Figure 5a and b].
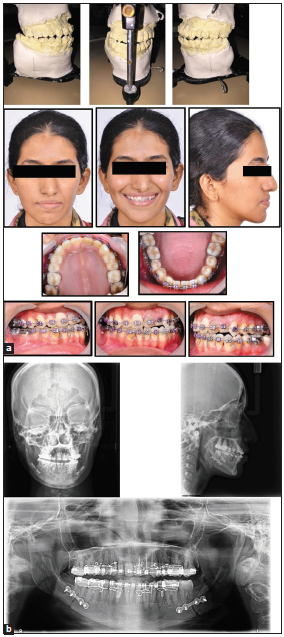
- (a) Photographs of the patient; 2 weeks after surgery. (b) Radiographs showing asymmetrical bilateral sagittal split osteotomy to match mandibular skeletal midline with facial midline followed by rigid fixation.
Treatment results
Finishing, detailing, and settling were initiated after a few weeks; good, acceptable functional occlusion with good facial esthetics was achieved. The patient was then referred for ceramic crowns for non-vital and root canal treated discolored, 21 and 22 [Figure 6]. The final records revealed convincing results, and the superimpositions confirmed the achievement of all treatment objectives [Figure 7].
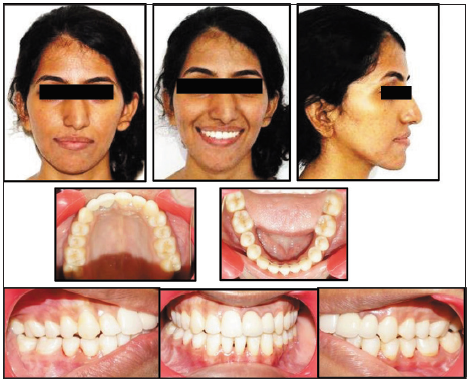
- Extraoral and intraoral photographs, after removal of the appliance.
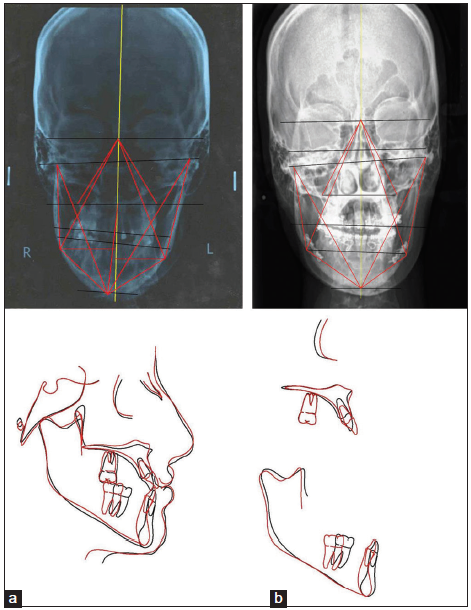
- Comparing pre- and post-treatment records: (a) Posteroanterior cephalograms showing the correction of asymmetry. (b) Superimposition of lateral cephalometric tracings pre-treatment (black) and post- treatment (red).
To enhance the facial esthetics further, the patient was advised to go for corrective rhinoplasty for nasal deviation, but as she was happy with the results achieved by mandibular surgery, she refused to undergo any further surgery.
Retention
Maxillary Hawley’s and mandibular fixed lingual retainer were given.
After 2 years’ follow-up [Figure 8], stability of surgical and orthodontic correction could be appreciated [Figure 9].

- (a) Two-year post-treatment follow-up: Extraoral and intraoral photographs. (b) Radiographs depicting the stability of achieved results.

- We have come a long way.
DISCUSSION
Facial asymmetry can severely hamper the esthetics. In the permanent dentition, dental asymmetries can be corrected through tooth movement. However, the difficulty arises in the case of skeletal asymmetry, due to mandibular arch, which is often the case,[7] due to longer growth period of the mandible.
When skeletal discrepancy is beyond the orthodontic envelope, camouflage of underlying skeletal discrepancy cannot be relied on to rectify severe dentofacial asymmetries. Surgical correction becomes challenging when the soft- and hard-tissue discrepancies do not match.[8]
In this patient, although the hard-tissue profile was concave, the soft-tissue profile was straight. The primary objective of the pre- surgical orthodontic treatment is to make the occlusal asymmetry equal in magnitude with that of the skeleton to enable to maximize correction of facial esthetics and achieve stable results, thus precluding the need for unnecessary surgery in the maxilla.[9] Correction of malocclusion, therefore, required an asymmetrical set back yielded favorable results.
To obtain post-operative long-term stability and fine results, planning dental and skeletal movement with reasonable bone positioning and rigid fixation are essential to achieve symmetry[10] and has led to the stable results for the presented case.
CONCLUSION
Complex facial asymmetry further mutilated by fractured condyle has been treated well after thoroughly evaluating the hard-tissue and soft-tissue discrepancies in all three planes with proper diagnosis and meticulous execution by carefully guiding the mandible in centric relation followed by combined orthodontic and surgical approach yielded extremely satisfying results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- History and current concepts in the analysis of facial attractiveness. Plast Reconstr Surg. 2006;118:741-56.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of facial asymmetry in the dentofacial deformities population at the university of North Carolina. Int J Adult Orthodon Orthognath Surg. 1997;12:171-6.
- [PubMed] [Google Scholar]
- An assessment of asymmetry in the normal craniofacial complex. Angle Orthod. 1978;48:141-8.
- [PubMed] [Google Scholar]
- Diagnosis and management of facial asymmetries. J Orthod Res. 2015;3:81-7.
- [CrossRef] [Google Scholar]
- Nonsurgical treatment of facial asymmetry in a growing patient. J Clin Orthod. 2013;47:121-8.
- [PubMed] [Google Scholar]
- Mysteries of asymmetries. Am J Orthod Dentofacial Orthop. 2000;117:577-9.
- [CrossRef] [Google Scholar]
- Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44:97-103.
- [PubMed] [Google Scholar]
- Asymmetric class III dentofacial deformities In: Dentofacial Deformities-Integrated Orthodontic and Surgical Correction Vol 4. (2). St. Louis, MO: Mosby; 1999. p. :2162-228.
- [Google Scholar]
- Post-operative stability after bimaxillary surgery in patients with facial asymmetry: Comparison of differences among different original skeletal class patterns. J Maxillofac Oral Surg. 2015;14:789-98.
- [CrossRef] [PubMed] [Google Scholar]






