Translate this page into:
Digital workflows in contemporary orthodontics
Address for Correspondence: Dr. Lars R. Christensen, 69-71 Banbury Road, Oxford, OX2 6PE, UK. E-mail: lchristensenortho@gmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Digital workflows are now increasingly possible in orthodontic practice. Workflows designed to improve the customization of orthodontic appliances are now available through laboratories and orthodontic manufacturing facilities in many parts of the world. These now have the potential to improve certain aspects of patient care.
Keywords
Custom appliances
digital impressions
indirect bonding
intraoral scanning
maxillary expanders
progress review
twin-block
INTRODUCTION
The rising popularity in intraoral scanning has opened up new avenues for planning, designing, and executing orthodontic treatment for our patients. This paper is by no means an exhaustive review of all the available options on the market but simply aims to give the reader ideas of some of the new workflows in the area of digital orthodontics.
DATA ACQUISITION
Intraoral three-dimensional (3D) data can be collected in many ways. Impressions or cast of patients can be scanned with desktop scanners and digital study models created for diagnostic purposes or to produce orthodontic appliances. Although this path is perfectly possible, one of the reasons for a digital workflow would be to avoid impression taking and model fabrication; this option is more suitable for eliminating larger quantities of already produced study models. The storage of models is often an issue for larger orthodontic practices as regulations surrounding medico-legal records often prohibit clinicians from discarding these. Several colleagues have been able to free up so much space from storage that they have been able to utilize the space for a new treatment room or something equally productive.
Over the last 3–4 years, the availability of intraoral scanning devices has increased considerably.[1,2] The speed and quality of the data set produced by these devices have increased considerably while the size and cost have reduced – the latter perhaps not as dramatically as the speed and quality.
Several of the intraoral scanners are now able to produce study and working models in color,[2] increasing the diagnostic and treatment planning options.
Clinicians have a wide variety of devices to choose from. The purpose of this paper is not to advocate a certain device. It is intended simply to illustrate some of the possible workflows with digital data capture. Our preferred choice is the Trios® 3 intraoral scanner (3Shape, Copenhagen, Denmark).
THE DIGITAL WORKFLOW
Having acquired the 3D data, they are usually saved in a Standard Triangulation Language (STL) format. The majority of the capturing systems are now “open” which means that we are able to use the STL files in various programs. There are usually several types of subscriptions or contracts available with the chosen scanner provider that will allow the user to export the data set either directly to a laboratory of choice or to other programs with specific functions for data manipulation. It is certainly recommended to research the various devices and subscriptions to ensure that the type of device and the output it produces are applicable to the functions the operator would like to use the data for.
From a personal perspective, I have been apprehensive with the implementation of a digital workflow in my practice. Until recently, there have been several obvious gaps in the workflow, and although there are advantages in many steps, the real advantage comes when the workflow is truly complete. I believe we are nearly at this stage now.
PATIENT EXPECTATIONS
Satisfying our patient’s expectations with our orthodontic care is what we all strive for. While this is not always possible, using photographs or an intraoral color scan can help the patient and the orthodontist determine which aspects the treatment plan needs to address for the resolution of their concerns [Figure 1].
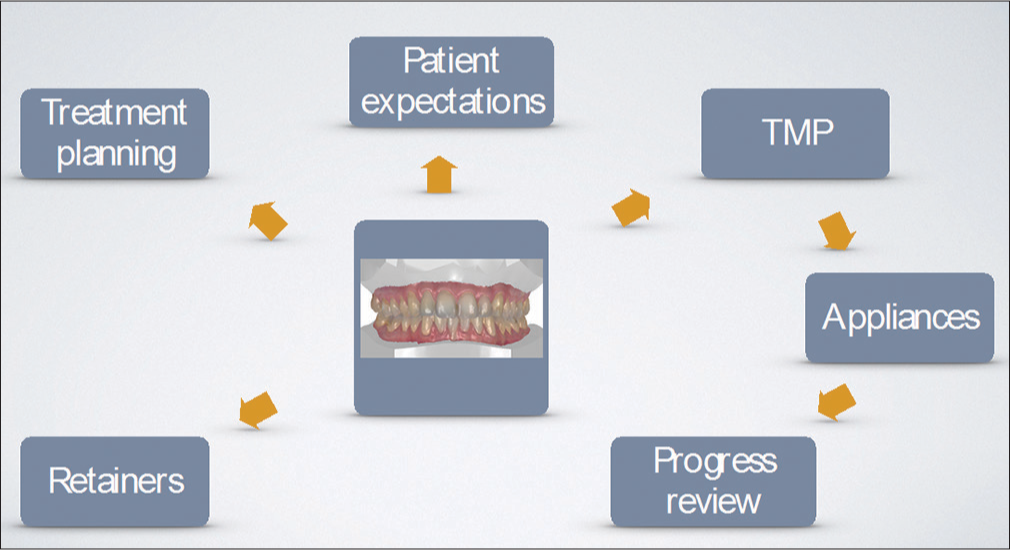
- Workflows discussed in the present article
TREATMENT PLANNING
Having a 3D model available for analysis can help the clinician obtain an array of data points in a very short period of time. Arch length, arch width, crowding, spacing, tooth size discrepancies, and occlusal plane assessments can be achieved with minimal effort.
Software packages are available to help the orthodontist or technician produce diagnostic setups that can then be reviewed with the patient to discuss different options for the orthodontic therapy and their likely visual outcomes. This can be particularly helpful if there are treatment options that require restorative or prosthodontic input – an obvious example being a canine substitution case where we can then illustrate the restorative needs for the canine and first premolar.
In adult-compromised cases, it can be helpful aligning the teeth digitally and reviewing this with the patient prior to agreeing, for example, that a residual overjet is inevitable if we treat a Class II case without surgery. Agreeing and obtaining consent with the patient is more valuable with this additional visual aid [Figure 2].

- Intraoral color scan is ready for use in discussion about treatment objectives with patient and for use in diagnosis and treatment planning
MANAGEMENT PORTALS
The 3D data can be exported to laboratories for production of appliances. Many of the companies offering appliances have portals helping the clinicians transfer the data securely through the Internet. Once received and accepted by the provider, the appliances can be designed and manufactured with possibilities for feedback during the design process by the responsible clinician. Examples of these are the Incognito Treatment Management Portal (3M Oral Care, USA) [Figure 3] and the Insignia custom bracket system (Ormco, USA). Many of the available providers will allow the clinician to review the predicted outcome of the appliance and revise the design to affect the design of the final appliance.

- The Incognito Treatment Management Portal used in the order and review process of the Incognito customized lingual appliance
APPLIANCES
It is impossible within the scope of this article to produce a definitive list of appliances that can be produced with 3D data. Instead, the aim of this paper is to show examples of appliances so far produced for my practice [Figure 4].

- The acquisition of a three-dimensional intraoral dataset can now be used for the manufacture of most orthodontic appliances
LABIAL APPLIANCES
The most frequent use of the 3D dataset so far has been for the production of bonding trays for indirect bonding. So far, we have tried three principal pathways; pressure-formed bonding trays, transparent and nontransparent silicone bonding trays, and direct 3D-printed bonding trays.
With the help of commercially available software, we can place the brackets on the 3D model and use tools to help facilitate the most accurate placement of the brackets [Figure 5].

- (a) The Orthoanalyzer Indirect Bonding Module allows the clinician or technician to place and customize brackets on the virtual study model. The customization can be fully controlled with the output of bracket placement heights, adhesive thickness as well as tip and torque values for each bracket. (b) The program calculation of occlusal interferences on the lower right premolar brackets (red circles on brackets)
Some software options offer the option to review the aligned brackets and teeth with a full-size wire, giving the clinician an indication of the 3D outcome after alignment of the dentition with the chosen bracket position [Figure 6]. The clinician can then modify the bracket position virtually and improve the predicted outcome. To my knowledge, to date, there has been no scientific validation of the actual outcomes achieved with these methods. Personally, I find it far simpler to review the bracket positions on the virtual model because of the multiple views we can obtain at the click of a button.

- Ormco Insignia Approver software for use with customized labial appliance manufacture
Once the clinician has validated the bracket positions, the bonding trays can be manufactured. This can be achieved in several ways; a 3D-printed model can be produced with the virtually placed brackets and a bonding tray can be produced on this model [Figures 7 and 8]. The model is produced with the tie-wing and hook undercuts blocked out to ensure the brackets fit in the bonding tray. The laboratory or clinical staff can then insert the brackets in the bonding tray prior to the bonding session.
![Formlab 2 SLA 3D printer used to produce models for indirect bonding models [Figure 8a] and retainer models](/content/9/2017/7/1/img/APOS-7-012-g007.png)
- Formlab 2 SLA 3D printer used to produce models for indirect bonding models [Figure 8a] and retainer models

- (a) Following the virtual bracket placement, a bracket transfer model can be produced using Appliance Designer software (3Shape, Copenhagen). The model produced has been designed with all undercuts of bracket tie-wings and hooks blocked out, facilitating easy insertion of the brackets into the bonding tray of choice. (b) Memosil customized indirect bonding tray for use with light-cured bonding materials. (c) Putty and wash-customized indirect bonding tray for use with chemically cured bonding materials
Our latest and most significant development in labial indirect bonding is to be able to print the bonding tray directly and without the need of a model. With the recently available, flexible biocompatible indirect bonding tray material (NextDent Ortho IBT) developed by NextDent, Eindhoven, NL, we are now able to design the bonding tray using Appliance Designer (3Shape, DK) [Figure 9] and output the design directly to a dental 3D printer [Figure 10]. At the time of writing this, only the Rapid Shape 3D printer (Rapid Shape GMBH, Germany) has specifications for this material. The material thickness can be selected exactly to the individual clinician’s preference. We chose to cover the entire bracket with 0.5 mm tray material and then digitally add a second layer of 1.5 mm for the incisal/occlusal part of the bracket. By covering the lingual surface, it is easy to get a very clear fit of the tray, and in cases with severe irregularity, we will add extra material on the occlusal aspect of the bonding tray to increase the stiffness of the bonding tray.

- Indirect bonding tray designed using Appliance Designer

- (a) Indirect bonding tray printed on Rapid Shape printer in biocompatible flexible NextDent Indirect Bonding Tray material. (b) Because of the materials’ flexibility and unique shape memory, it is possible to cover the entire bracket with the indirect bonding material. The bonding material can be easily bend away from the brackets after light curing because all the undercuts have been blocked out on the virtual model prior to designing the bonding tray. (c) Bonding tray in place with excellent fit to teeth
Ormco Insignia is a custom-made labial appliance produced from intraoral scans or scans of polyvinyl siloxane impressions of patients. Currently, only a self-ligating bracket with a custom cut base and bonding pad is available from the Insignia system. These custom appliances are delivered to the clinician in bonding trays ready for delivery to the patient [Figure 11].

- Ormco Insignia Custom appliance ready for indirect bonding
EXPANDERS
Custom-made maxillary expansion appliances can be produced from the 3D dataset. These appliances can be laser sintered directly from the STL files producing individualized “bands” for the patient’s teeth. The three main advantages are that we no longer need to place separators between the teeth thereby eliminating a visit and the inherent discomfort that is associated with separators and the appliance can be produced with laser welding, thus avoiding the traditional soldering techniques with the potential allergenic components in the solder. Finally, the fit will often be more smooth and comfortable for the patient as the rings created for the teeth are 100% custom made [Figure 12a-c].

- Laser-sintered maxillary expander with laser-welded midline expansion screw (Technician Stefano Negrini). (a) Occlusal view. (b) Palatal view. (c) Maxillary expander in place
FUNCTIONAL APPLIANCES
The success rate of functional appliances depends on many things, but certainly the precision fit of the appliance is a significant factor. In collaboration with Stefano Negrini (Ortodonzia Estense, Italy), we have developed a treatment flow where we can eliminate the impression taking and bite registration with the traditional methods. Instead, the dentition is captured with an intraoral scan, and following the scan of the occlusion, a protrusive bite registration is obtained with the patient instructed to bite to the desired protrusive position [Figure 13].

- Intraoral scans positioned with protrusive bite scan
The functional appliance is subsequently designed using Appliance Designer (3Shape, DK) and sent to the clinician for approval prior to production [Figure 14]. The appliance can then be milled in polymethyl methacrylate using a 3D dental milling machine. Provided the teeth supporting the appliance have sufficient undercuts, the appliance can be made completely without metal components. However, if the teeth are shallow, adding one or more metal clasps to the appliance can increase retention [Figure 15]. Likewise, expansion screws can be added as necessary [Figures 16 and 17].

- Design prepared by technician (Stefano Negrini) and sent for approval

- Milled and polished twin-block appliance with retentive ball hooks placed after milling

- The milled appliances can have expansion screws placed after milling and before finishing polish

- Example of milled functional appliance. (a) Pretreatment occlusion. (b) Appliance in place. (c) Posttreatment occlusion before fixed appliance phase
Once suitable biocompatible 3D-printing resins become available, it will be possible to produce the appliance on a 3D printer rather than using more expensive 3D milling machines.
Our clinical experience so far has been very favorable as we can make the appliances less visible, and in many cases, very low profile [Figures 18 and 19] which shortens the adaptation period, is more acceptable to the patients, and aids with speech adaptation.

- Example of low-profile twin-block with only acrylic retention. This design requires care and attention in the design step as any erupting tooth can disrupt the fit of the appliance once delivered

- Occlusal view of low-profile appliance
ALIGNER SYSTEMS
There are multiple aligner suppliers that can now receive 3D dataset and produce the setups and aligners from the data. We have experience with ClearCorrect and Invisalign which both have dedicated portals for several scanner systems including our preferred system Trios 3 (3Shape, DK). The significant advantage is the elimination of shipping and the time for the records to reach the aligner manufacturer. This has significantly reduced our turnover times, which is often very much appreciated by our patients. We have experienced better fitting appliances delivered in a shorter time frame.
PROGRESS REVIEW
One of our constant clinical challenges is to monitor our patient’s progress. Using intraoral 3D scanning can be a very helpful tool for this. By simply scanning the patient during treatment, we can superimpose the scans and check tooth movement a little more precisely [Figure 20]. With a good-quality intraoral scanner, this can be a quick and noninvasive technique to review patient progress. Currently, the Trios 3 (3Shape, DK) is preferred; this is a 2–3 min process for double jaw scanning. Jung et al.[3] have documented the accuracy of intraoral scans from the Trios and iTero scanners on scans with brackets in place to be clinically acceptable for progress comparisons.

- Progress review using intraoral scans. The left diagram shows patient’s intraoral scan for the design of the Incognito appliance. The middle diagram shows treatment scan of the upper jaw with the appliances in place. To the left, the two scans have been superimposed using surface superimposition around the palatal rugae. The progress of the incisor correction and arch form can be reviewed
We have found this a very valuable tool in progress reviews with the patient and perhaps particularly helpful in more challenging aligner and lingual appliance cases.
RETENTION
Our clinical aim is for our patients to have the retainers delivered later the same day or the next day the latest for optimal fit and retention of the achieved result. By obtaining a posttreatment scan immediately after debonding, we can print the arches for pressure-forming technique within 3–4 h. This is in principle not faster than an aliginate impression, poured and set, but the staff time is less and it is more comfortable for the patient. The added benefit is that the 3D model has a better strength and there is no risk of breaking incisal edges with the pressure-forming technique, which is not infrequent when we try and rush a set of retainers to form plaster models for a patient. The retainer model can be stored either with the patient or in house and reused whenever new retainers are required.
Commercially available software can remove the brackets from the virtual models, so it is in fact possible to perform a scan of the patients’ dental arches (preferably without the archwire in place) and digitally remove the brackets and produce the retention devices so they are ready on the day of debonding. Several laboratories are now offering this service. Clearly, the last visit needs to be with passive archwires for this process to work well.
When fixed retainers are needed, we scan the anterior teeth of the two arches on the patient’s penultimate appointment and we then have the laboratory (CA-Digital, Germany) produce high-precision custom-fixed retainer wires. The Memotain wires are machine cut from a flat sheet ensuring the wire is in one plane with a dimension of 0.4 mm × 0.4 mm (0.0165 × 0.0165) [Figures 21 and 22]. We have used the Memotain wires routinely for complex cases over the last 18 months and these are particularly helpful in the upper arch where it is often difficult to avoid occlusal contact from the lower canine teeth. The wires are delivered in time for the debonding appointment and can be fitted while the fixed appliance is still in place in cases where we are trying to prevent even the smallest relapse of, for example, a median diastema.

- Memotain (CA Digital) retainer delivered with positioning jig

- Memotain retainer placed with Transbond LV and occlusion checked
CONCLUSIONS
The introduction of intraoral scanning has helped us to produce new practice workflows that have enabled us to produce more complex appliances with high precision. This has most certainly benefitted the patients and in many situations has eliminated appointments such as separation placement and repeated appointments for retainer impressions. Over the last 2½ years, we came across only one patient who preferred the alginate impressions.
The time-saving aspects of not having to courier impressions or other records overseas for the preferred laboratory means that we can now work with our preferred partners much more efficiently and at a little less cost.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr Christensen holds advisory board positons with 3M Oral Care and 3Shape.
References
- Orthodontic scanners: What’s available? J Orthod. 2015;42:136-43.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoral scanning systems – A current overview. Int J Comput Dent. 2015;18:101-29.
- [Google Scholar]
- Accuracy of four different digital intraoral scanners: Effects of the presence of orthodontic brackets and wire. Int J Comput Dent. 2016;19:203-15.
- [Google Scholar]






