Translate this page into:
Early timely orthodontic treatment: Treatment of unerupted maxillary laterals

*Corresponding author: Peter Ngan, Department of Orthodontics, West Virginia University, Morgantown, West Virginia, United States. pngan@hsc.wvu.edu
-
Received: ,
Accepted: ,
How to cite this article: Ngan P, Sarraj M, AlSaty G. Early timely orthodontic treatment: Treatment of unerupted maxillary laterals. APOS Trends Orthod 2021;11(1):4-13.
Abstract
There is no universal agreement as to which type of orthodontic or orthopedic treatment deserves early intervention. In addition, there is a need for more information as to which treatments are the most effective and less costly if they are initiated timely in the mixed dentition. Early timely treatment may benefit young patients with a maxillary transverse deficiency with or without a posterior crossbite that requires maxillary expansion. It may also be indicated in children with anteroposterior jaw discrepancy that requires chin cup or maxillary protraction. In this paper, the authors will focus on early maxillary expansion to facilitate the eruption of maxillary laterals. In specific, the authors will present a contemporary protocol using a bonded maxillary expander as anchorage for treatment of unerupted maxillary laterals. The use of this protocol was illustrated with two case reports to enable clinicians to routinely achieve a beautiful smile on a young patient by timely alignment of the maxillary incisors.
Keywords
Banded maxillary expansion
bonded maxillary expansion
early treatment
INTRODUCTION
An estimate of 25% of malocclusions can be intercepted at an early age.[1] However, there is still an ongoing discussion among dentists and orthodontists as to the optimal time to initiate orthodontic or orthopedic treatment under various clinical conditions.[2] The fact is that there is a delicate balance between the benefit of early orthodontic or orthopedic treatment and the biological and financial cost of having another phase of treatment. Hence, clinicians are still debating as to which type of treatments are most beneficial to initiate in the mixed dentition.
In the literature, there is no universal agreement as to which type of early treatment will achieve the best outcome. The American Orthodontist Association recommends an orthodontic consultation for all children by the age of 7 years.[3] However, if you are parents, you will agree with me that all 8-year-old children should have a beautiful smile. The “Gold Standard” of starting orthodontic treatment is in the late mixed dentition or early permanent dentition. This is because there will be some growth remaining to assist in the treatment and permanent dentition will be available for positioning of occlusion. However, one may depart from the “Gold Standard” if there is prolonged growth unfavorably or there is persistent anterior open bite due to excessive eruption of posterior teeth relative to the vertical growth of the ramus. In addition, certain malocclusions may benefit from earlier treatment such as maxillary transverse deficiency that requires expansion to take advantage of the patent maxillary sutures;[4] posterior crossbite due to a functional side shift; or anteroposterior jaw discrepancy that requires chin cup or maxillary protraction.[5] This article focuses on early maxillary expansion to facilitate eruption of unerupted maxillary laterals. Specifically, the authors present a contemporary protocol using a bonded expander as anchorage to facilitate the alignment of maxillary incisors in the early mixed dentition.
DIAGNOSIS OF MAXILLARY TRANSVERSE DEFICIENCY
Diagnosis in the transverse dimension should be on the top of our problem list when we formulate a treatment plan for young patients. The presence of facial asymmetry, anteroposterior jaw differences, insufficient buccal overjet, and dental compensation can all contribute to a “relative” or “absolute” transverse deficiency.[6]
Clinically, unilateral posterior crossbite with a functional shift or bilateral posterior crossbite is the most common findings for patients with maxillary transverse deficiency. However, patients with dental compensation of the posterior molars may not present with a posterior crossbite. Vanarsdall[7] proposed the use of a posterior-anterior (PA) cephalogram and a Maxillo-mandibular Transverse Differential to quantify the differential width of the maxilla and mandible. The limitation of this method is that few clinicians are taking PA cephalogram for diagnosis. In addition, the antegonial landmark is far back from the dentition and may not be an accurate landmark to be used to determine the skeletal width of the mandible. McNamara and Brudon[8] measured the transpalatal width from lingual groove to lingual groove on the opposite side of the maxillary first molars and reported an average norm of 35 ± 1.4 mm. However, this measurement did not take into consideration the buccolingual inclination of the molars. At West Virginia University, the Will Andrews and Larry Andrews (WALA) Ridge, or the most prominent portion of the mandibular mucogingival junction suggested by Andrews[9] is used as a landmark for determining the buccal lingual position of the lower teeth. For example, the optimal position of the mandibular first molar is 2 mm from the facial axis or FA point of the clinical crown to the WALA ridge [Figure 1]. In this position, the first molars are decompensated, and the width of the mandibular arch can then be measured from the central fossae of the mandibular first molar to the opposing molar to compare with the maxillary arch width. This measurement can also be performed with the help of a cone-beam computed tomography scan to check the root inclination and angulation in addition to the clinical crown.[10,11]

- Facial axis (FA) point of the clinical crown and WALA Ridge of the mandibular arch showing the optimal position of the mandibular first molar is 2 mm from the FA point of the clinical crown to the WALA ridge.
TREATMENT OF UNERUPTED MAXILLARY LATERALS
Early diagnosis and treatment can guide the eruption of teeth into a more favorable position and preserve space for permanent teeth.[12] In the primary or early mixed dentition, treatment of maxillary transverse deficiency can still utilize conventional tooth-borne rapid palatal expansion (RPE) appliance without the aid of temporary skeletal anchorage devices. One also has the choice of using a conventional banded expander or a bonded RPE as anchorage for maxillary expansion. Two case reports were presented to contrast the treatment of unerupted maxillary laterals using a conventional banded RPE with bonded RPE using contemporary bonding materials.
Conventional treatment with a banded RPE and 2 × 4 fixed appliance
The Hyrax RPE appliance consisted of a central expansion jackscrew and four attached arms soldered to orthodontic bands. The jackscrew was connected to the maxillary primary first molars and permanent first molars by a heavy wire (0.043). The appliance was activated twice daily (0.025 mm per turn) for 1–2 weeks, depending on the amount of maxillary deficiency.
At the completion of maxillary expansion, orthodontic brackets were bonded to the maxillary four incisors. A sequence of wires was placed to align the incisors and to maintain the forward position of the incisors. An open coil spring was placed between the primary first molars and the incisors to facilitate closure of the diastema if necessary. The length of treatment is around 6–8 months, followed by retention with a retainer until the exfoliation of primary molars. An alginate impression was taken after removal of appliances and a Hawley or clear plastic retainer with full palatal coverage was fabricated to maintain the arch width and alignment of incisors.
Case 1
Diagnosis
An 8-year-old female presented to the WVU Orthodontic Clinic with a chief concern of “space in the upper front teeth.” Clinical examination revealed a convex profile with a retrusive mandible. Intraoral examination revealed a Class I malocclusion with a 2 mm overjet and 30% overbite. The maxillary intercanine width (ICW) was 26 mm and the mandibular ICW was 27 mm width. The maxillary intermolar width (IMW) was 37 mm and the mandibular IMW was 40 mm. There was moderate-to-severe crowding in the maxillary and mandibular arches with a 2 mm median diastema and blocked out maxillary laterals [Figure 2]. Panoramic evaluation showed the presence of all permanent teeth and no pathology [Figure 3]. Lateral cephalometric analysis revealed a Class I skeletal relationship (ANB = 2, Wits = 0 mm) with a normal divergent growth pattern [Figure 4]. Soft-tissue analysis showed lip incompetency in repose with a slightly protrusive lower lip.

- Case 1 pre-treatment facial and intraoral photographs. An 8-year-old female with crowding in the upper anterior teeth.
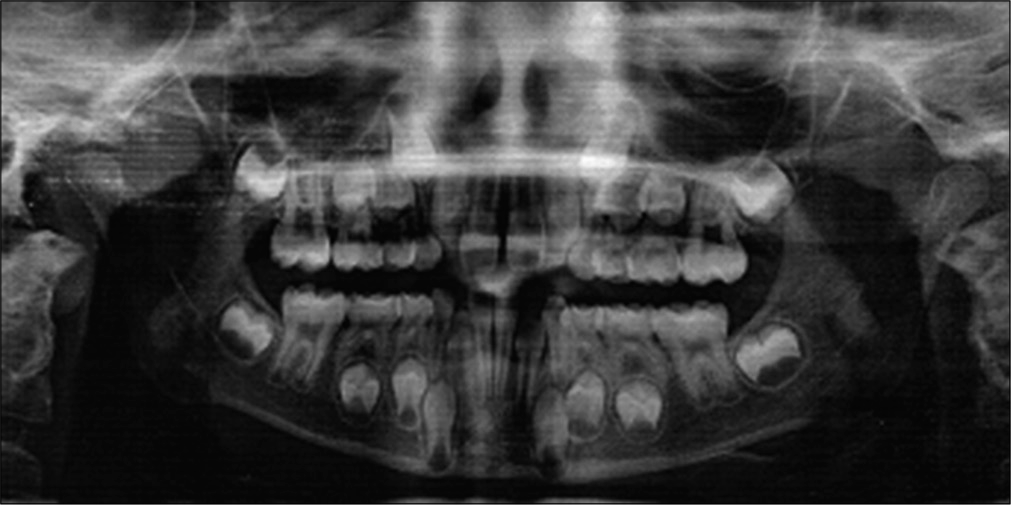
- Case 1 pre-treatment panoramic radiograph.
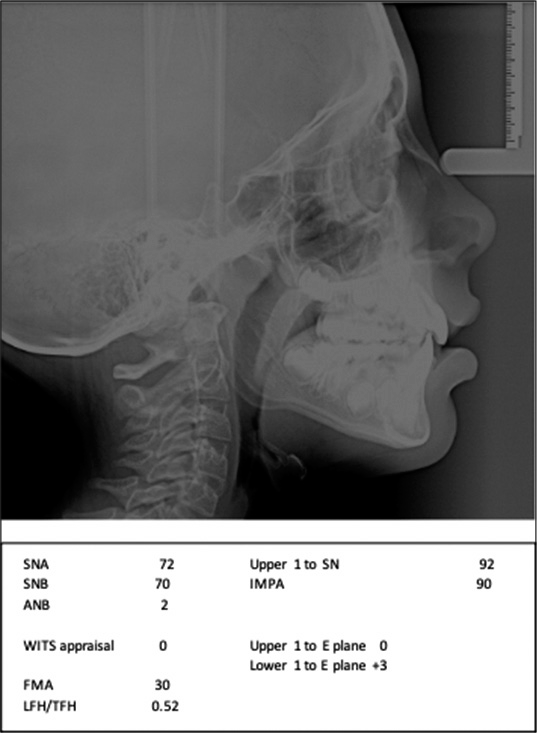
- Case 1 pre-treatment lateral cephalogram and measurements.
Treatment objectives
The treatment objectives were to normalize the maxillary dental arch width and resolve maxillary crowding to facilitate the eruption of maxillary lateral incisors. The patient also requested an improvement in facial appearance and smile. Alignment of mandibular incisors was deemed not necessary because of secondary spacing in the lower arch and this objective can be resolved during Phase II comprehensive orthodontic treatment.
Treatment alternatives
Two different treatment options were suggested. The first option was an early phase of expansion and alignment of maxillary incisors. The second option was to wait until the eruption of all the permanent teeth and perform the comprehensive orthodontic treatment to resolve both the maxillary transverse deficiency and crowding issues in one phase of treatment. The patient and the parents agreed to the first treatment option and desired a better-looking smile for the school picture.
Treatment progress
Orthodontic bands were fitted on the maxillary first primary molars and permanent first molars. A Hyrax RPE was fabricated and cemented with glass ionomer cement. Patient was asked to make two turns per day on the jet screw for 2 weeks. A maxillary diastema of 3.5 mm was obtained after expansion. Orthodontic brackets were bonded on the maxillary incisors together with a 0.014 NiTi wire to maintain the forward position of the incisors. At the second appointment, a 0.018 NiTi wire was placed and a coiled spring was trapped between the maxillary central incisor and the primary canines to open space for the eruption of the laterals. At the third appointment, 0.018 SS wire was placed and the maxillary incisors were consolidated with chain elastics and retracted using the RPE as anchorage [Figure 5].
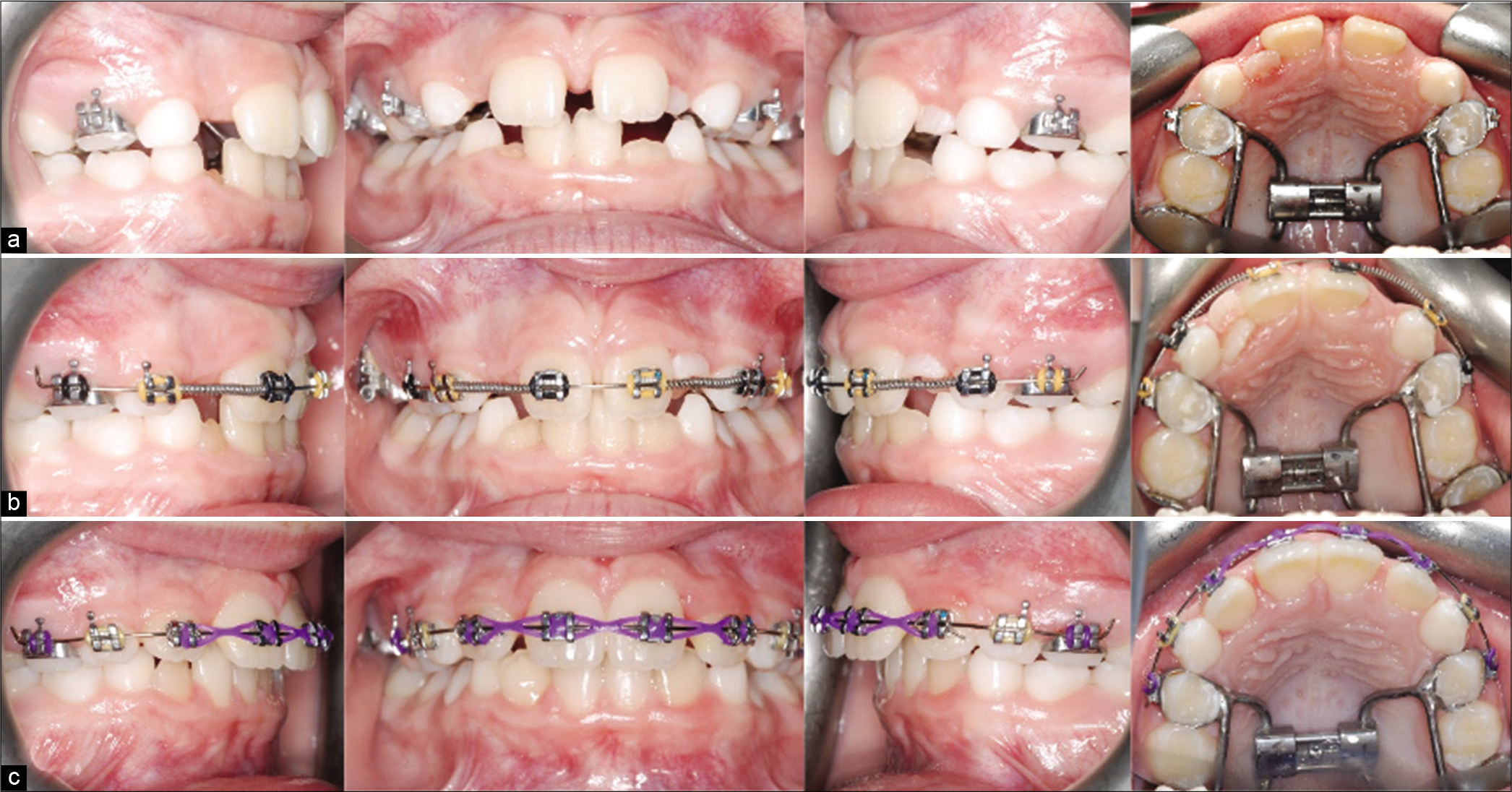
- Case 1 (a) progress treatment photographs after maxillary expansion. (b) Progress treatment photographs showing the use of coiled springs to close diastema. (c) Progress photographs of alignment of maxillary incisors.
Treatment results
Treatment was completed in 8 months. A Hawley retainer was fabricated for retention. This early phase of treatment normalizes the width of the dental arch. The post-treatment photographs show an improvement in the dental arch form and alignment of the maxillary incisors. The facial photograph shows an improved smile with a balanced lip position [Figure 6].

- Case 1 post-treatment facial and intraoral photographs.
Contemporary treatment with a bonded RPE and 2 × 4 fixed appliance
The use of a bonded RPE is not new to the clinicians. The advent of new materials for the fabrication of the appliance as well as the ease of appliance removal significantly reduces the number of appointments, chair time, and efficiency of a bonded expansion appliance. The bonded RPE consisted of a central expansion jackscrew and occlusal coverage for all the posterior teeth with the material Biocryl® (Great Lakes Orthodontics, Tonawanda, NY). The DeLuke Contoured Expander technique simplifies and improves the efficiency of palatal sutural expansion.[13] The thickness of the material was chosen based on the type of malocclusion (1–2 mm for routine expansion and 3 mm thickness for open-bite cases). Table 1 shows the steps in the fabrication of a contemporary bonded RPE [Figures 7a-j]. Table 2 shows the steps in the placement of the appliance in a patient.
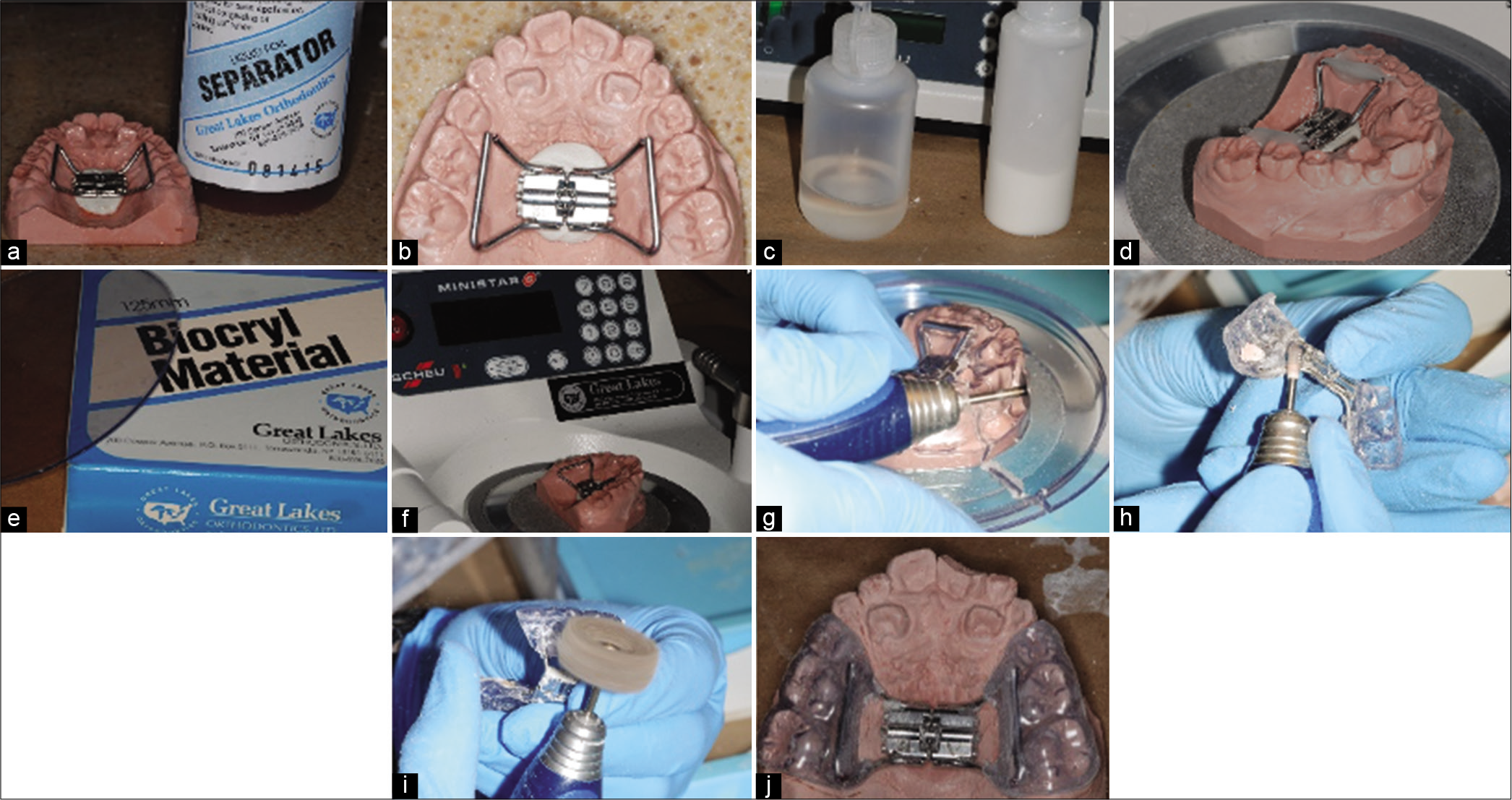
- (a-j) Steps in fabrication of a bonded RPE appliance. Table 1 for description of each steps.
| 1. Block out any undercuts on the dental cast used for fabrication of the appliance 2. Apply Liquid Foil Separator® (Great Lakes Orthodontics, Tonawanda, NY) on the cast using a brush to facilitate the separation of the appliance from the cast. [Figure 7a] 3. Adapt the arms of the jackscrew with the palate and position it 1–2 mm away from the tissue and the teeth 4. Bend the posterior arms to align with the middle of the lingual surface of the first molar and bend the anterior arms to align with the middle of the lingual surface of the first primary molars 5. Secure the jackscrew in the middle of the palate (arrow pointing toward the posterior) and secure it with wax [Figure 7b] 6. Mix acrylic (monomer and polymer) and place a small amount over the expander arms only to secure the bond between the expander arms and the Biocryl® [Figure 7c and d] 7. Using a thermal vacuum machine (Minstar S®, Great Lakes Orthodontics, Tonawanda, NY) to heat the Biocryl®to the specified times according to the manufacturer’s directions and form over the model [Figure 7e-g] 8. After the acrylic hardens, remove the appliance from the pressure pot and trim away excess Biocryl®material 9. Remove the expander from the cast and trim the buccal and lingual surfaces. Contour the acrylic to the gingival margins of the posterior teeth and end in a gentle taper [Figure 7h and i] |
| 1. Prophy the maxillary posterior teeth 2. Try-in the expander in the patient’s mouth, remove and dry the appliance before bonding 3. Apply Plastic Conditioner® (Reliance, Itasca, IL) on all the internal surfaces of the expander for 60 sec. and dry the appliance 4. Etch the buccal surface of all posterior teeth for 30 s, rinse and dry. Etching the lingual and occlusal surfaces in addition to the buccal surface may result in excess retention and difficulty to remove on debonding of the appliance 5. Apply Assure Plus® (Reliance, Itasca, IL) bonding resin on the buccal surface of posterior teeth and cure with LED light 6. Mix and apply Excel Regular Paste A&B® (Reliance, Itasca, IL) bonding material on all the internal surfaces of the expander. We recommend the use of fluoride-releasing bonding material 7. Insert the expander and make sure it is fully seated 8. Remove all excess bonding material around the margins of the expander with Q-tips or micro-brush. We recommend the use of moderate-viscosity, colored bonding material for ease of placement and cleanup 9. Ask the patient to keep biting on two cotton rolls (one on each side) for three minutes 10. Start activating the jet screw on the same day |
The activation protocol was similar to the conventional RPE. At the completion of maxillary expansion, orthodontic brackets were bonded to the maxillary four incisors. Molar tubes or brackets can be bonded on the buccal surface of the expander using Bond Aligner® (Reliance, Itasca, IL) resin. The wire sequence in the alignment of the incisors was similar to the conventional RPE protocol. For removal of the bonded RPE, an acrylic debonding Plier® (Ortho Technology, West Columbia, SC) was used to remove the appliance without causing discomfort to the patient. The remaining material was removed by a scaler or with the help of a bur.
Case 2
Diagnosis
A 10-year-old female presented to West Virginia University Orthodontic Clinic with a chief concern of “My dentist said I need to see you.” Clinical examination revealed a straight facial profile with lip strain on repose. Intraoral examination revealed an end-to-end molar relationship and a Class I canine relationship with a 2 mm overjet and 20% overbite. The maxillary and mandibular ICW were both 28 mm. The maxillary IMW was 40 mm and the mandibular IMW was 43 mm. There was moderate to severe crowding in the maxillary and mandibular arches with a 2 mm median diastema and completely blocked out maxillary laterals [Figure 8]. Panoramic evaluation showed the presence of all permanent teeth and no pathology [Figure 9]. Lateral cephalometric analysis revealed a Class I skeletal relationship (ANB = 1, Wits = -1 mm) with a slightly hyperdivergent growth pattern [FMA = 31, Figure 10]. Soft-tissue analysis showed the presence of lip strain in repose with slightly protrusive lower lip.

- Case 2 pre-treatment facial and intraoral photographs. A 10-year-old female with severe crowding and blocked out maxillary laterals.
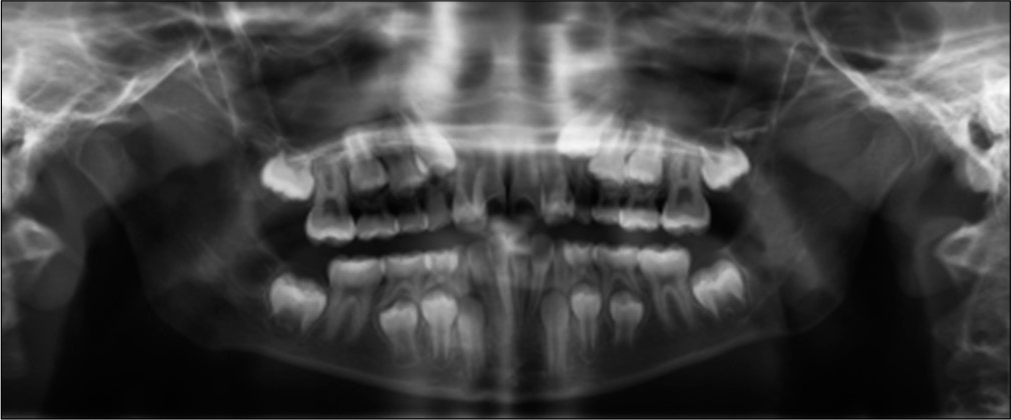
- Case 2 pre-treatment panoramic radiograph.
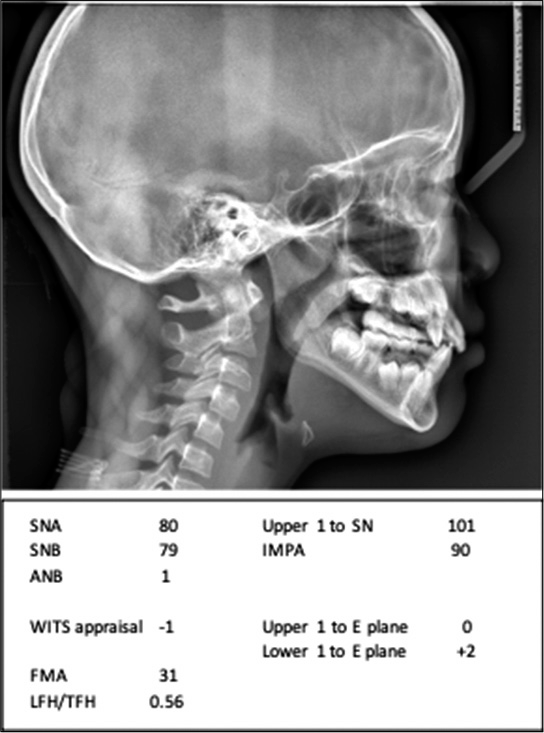
- Case 2 pre-treatment lateral cephalogram and measurements.
Treatment objectives
The treatment objectives were to normalize the maxillary dental arch width and resolve maxillary crowding to facilitate the eruption of maxillary laterals. The patient wanted to improve her facial appearance and smile esthetics. Alignment of mandibular incisors is not necessary as this objective can be resolved during Phase II comprehensive orthodontic treatment.
Treatment alternatives
Patient was informed that the early phase of expansion and alignment of maxillary incisors were mandatory due to complete block out of the maxillary laterals. Maxillary expansion to normalize the width of the maxillary arch will provide space for alignment of the maxillary incisors without extraction of the primary canines. The patient and the parents agreed to the suggested treatment and desired a better-looking smile for the school picture.
Treatment progress
An alginate impression was taken to fabricate a bonded maxillary expansion appliance [Figure 11]. Maxillary premolar brackets were bonded on the buccal surface of the expander to provide a slot for archwire engagement [Figure 12]. The over-retained maxillary primary lateral incisors were extracted. Patient was asked to make two turns per day on the jet screw for 2 weeks. A maxillary diastema of 3.5 mm was obtained after expansion. Orthodontic brackets were bonded on the maxillary central incisors and primary canines together with a 0.014 NiTi wire. At the second appointment, a coiled spring was trapped between the maxillary central incisor and the primary canines to open up space for the eruption of the laterals. At the subsequent appointments, the maxillary central incisors were consolidated, and the maxillary laterals were guided into the dental arch using the RPE as anchorage [Figure 13].
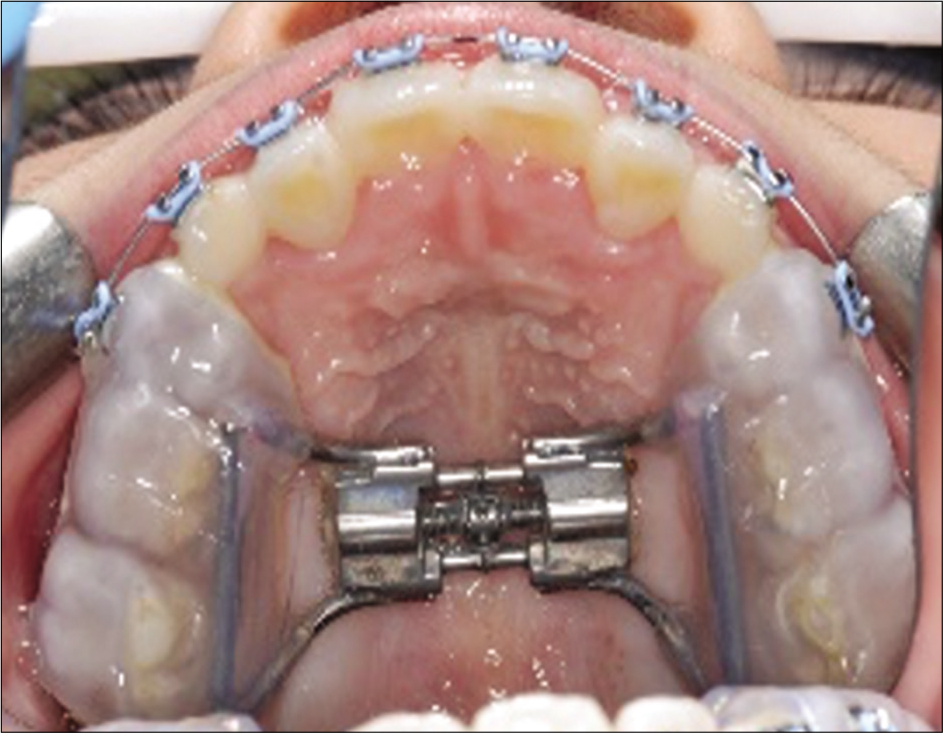
- Fabrication of a bonded RPE using the DeLuke Expander technique.

- The technique of bonding a bracket on the buccal surface of a bonded RPE.
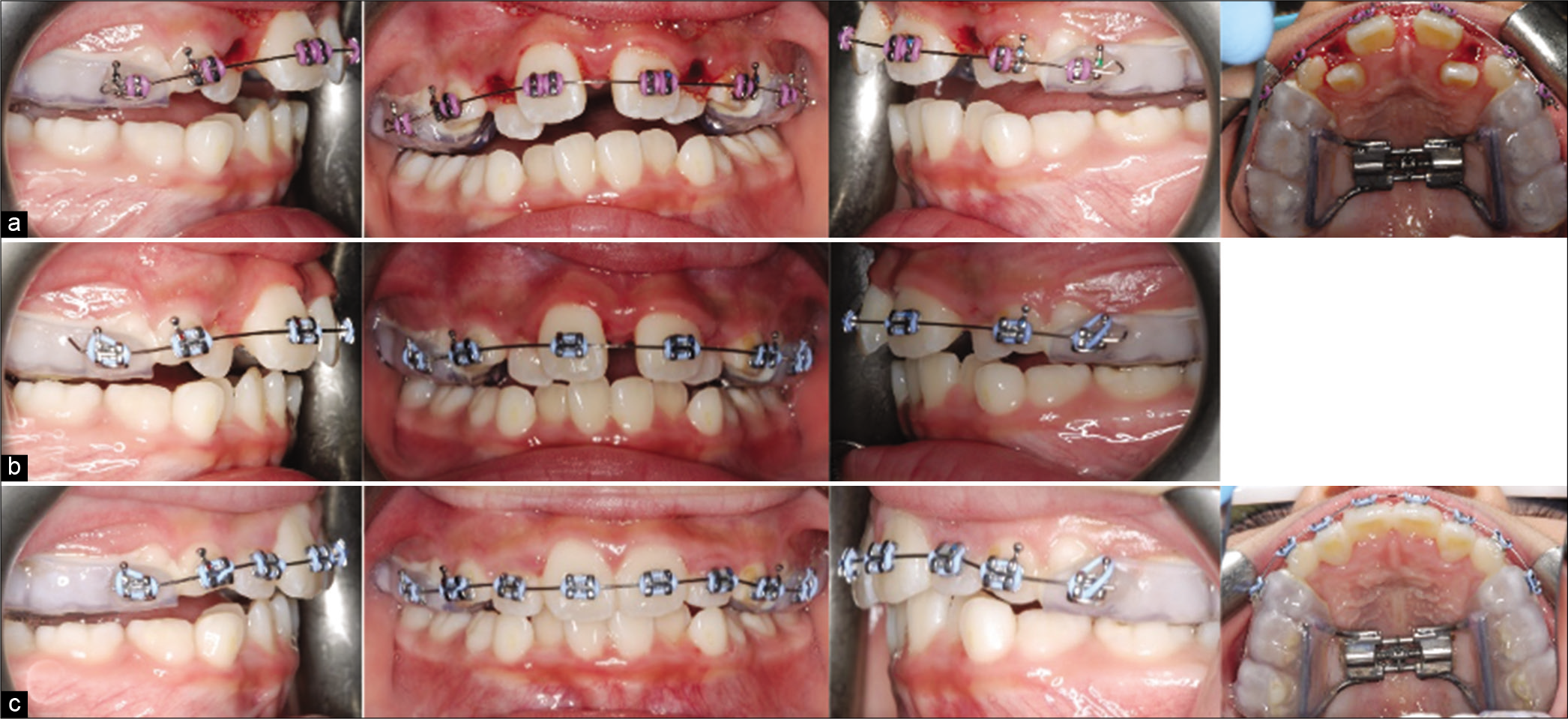
- Case 2 (a) progress treatment photographs after maxillary expansion. Notice the bite-opening immediately after expansion. (b) Settling of the posterior occlusion after 2 months. (c) progress treatment photographs showing alignment of the maxillary incisors.
Treatment results
Treatment was completed in 6 months and a Hawley retainer was fabricated for retention. The post-treatment photographs show a normalized maxillary arch width and improvement in the alignment of the maxillary incisors. The facial photograph shows improved smile esthetics with a balanced lip position [Figure 14].

- Case 2 post-treatment facial and intraoral photographs.
DISCUSSION
There is no universal agreement as to which type of early treatment will achieve the best orthodontic outcome. Clinicians must evaluate the cost-benefit ratio to decide whether to add another phase of treatment. Early treatment of maxillary transverse deficiency takes advantage of the patent maxillary sutures and elicits a more physiological separation of the sutures. Maxillary expansion performed after pubertal growth spurt may change from skeletal to a more dentoalveolar adaptation.[14] An estimate of 60% of treated malocclusions may benefit from some sort of maxillary expansion.[15] In addition, skeletal separation of the mid-palatal sutures creates space for alignment of maxillary incisors, especially in cases with mild-to-moderate amount of crowding. This may prevent the need for extraction of permanent teeth, especially in marginal extraction malocclusions. This idea of early intervention appears to be logical to prevent an occurrence of abnormality rather than waiting until it has been developed fully.[16]
Most clinicians agree that maxillary expansion should be initiated in the late mixed dentition. However, earlier intervention is sometimes indicated. For example, when crowding is severe enough to prevent the natural eruption of the permanent laterals, earlier intervention may prevent unfavorable enamel wear on the malpositioned teeth.[17]
There are two theories trying to explain the etiology of palatally impacted maxillary canines. According to the guidance theory, the canine lacks the guide during the eruption pathway because of extra space in the apical part of the maxilla, due to the hypoplastic or missing lateral incisor. This theory supports that palatally displaced canines are frequently found in dentitions with peg-shaped or missing laterals and spaced and late developed dentitions.[12] Therefore, in situations with the completely blocked out maxillary laterals such in the second case report, unerupted maxillary lateral should be brought in place as early as possible. Clinicians should avoid using rectangular archwires to minimize root movements and therefore disturb the eruption of the maxillary canines which may lean on the apical aspect of the laterals.
The use of a bonded RPE for maxillary expansion and anchorage may reduce the number of appointments and save chair time. Banded appliances require an appointment for placement of separators and fitting of molar bands and soldering of jackscrew to the molar bands. With the advent of intraoral scanning, the fabrication of a bonded RPE can be done in-house and requires only an intraoral scan and printout of the cast with a 3-D printer.
Proper rigidity of the appliance is necessary to prevent unwanted tipping of the dentition. Sarver and Johnston pointed out the rigidity of an appliance could decrease the rotational component of force along the long axis of the tooth.[18] Asanza et al.[19] suggested that the occlusal coverage of a bonded RPE appliance can reduce the extrusive side- effects of RPE and can minimize the buccal tipping of posterior teeth and the alveolar processes.[20,21] Another benefit of the posterior occlusal coverage is to intrude or maintain the vertical position of the posterior teeth.[22] In addition, the bite-block effect facilitates correction of anterior crossbites in patients with deep bite malocclusion due to elimination of occlusal interferences.[23]
CONCLUSION
There is a need for assessing the cost-benefit ratio when instituting early orthodontic treatment. Early treatment of unerupted maxillary laterals with expansion and 2 × 4 fixed appliances allows clinicians to normalize the width of the dental arch, prevent blocked out maxillary lateral incisors as well as providing a pleasing smile for the growing child. The use of a contemporary bonded expander reduces the number of appointments, chair time, as well effective anchorage for maxillary expansion and alignment of maxillary incisors. The laboratory fabrication of the appliance and clinical management was outlined to facilitate clinicians adapting to their clinical practice.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A longitudinal comparison of the orthodontic treatment priority index and the subjective appraisal of the orthodontist. J Public Health Dent. 1971;31:2-8.
- [CrossRef] [PubMed] [Google Scholar]
- Early timely treatment of Class III malocclusion. Semin Orthod. 2005;11:140-5.
- [CrossRef] [Google Scholar]
- Orthodontic intervention in the early mixed dentition: A prospective, controlled study on the effects of the eruption guidance appliance. Am J Orthod Dentofacial Orthop. 2008;133:254-60.
- [CrossRef] [PubMed] [Google Scholar]
- An interview with Dr. Eric Liou by Dr. Narayan Gandedkar. J Asia Pac Orthod Soc. 2010;1:1-8.
- [Google Scholar]
- Maxillary transverse expansion in adults: Rationale, appliance design, and treatment outcomes. Semin Orthod. 2018;24:52-65.
- [CrossRef] [Google Scholar]
- Transverse dimension and long-term stability. Semin Orthod. 1999;5:171-80.
- [CrossRef] [Google Scholar]
- Orthodontic and orthopedic expansion in the transverse dimension: A four decade perspective. Semin Orthod. 2019;25:3-15.
- [CrossRef] [Google Scholar]
- The six elements of orofacial harmony. Andrews J Orthod Orofac Harmony. 2000;1:24-5.
- [Google Scholar]
- A CBCT evaluation of root position in bone, long axis inclination and relationship to the WALA ridge. Semin Orthod. 2019;25:24-35.
- [CrossRef] [Google Scholar]
- A review of early displaced maxillary canines: Etiology, diagnosis and interceptive treatment. Open Dent J. 2011;5:39-47.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.deluke.com/bonded-expander
- Evaluation of the effect of rapid maxillary expansion on the upper airway using nasofibroscopy: Case report and description of the technique In: Dent Press J Orthod. Vol 16. 2011. p. :81-9.
- [CrossRef] [Google Scholar]
- Mandibular changes in persons with untreated and treated Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 1998;113:661-73.
- [CrossRef] [Google Scholar]
- Early orthodontic treatment: What are the imperatives? J Am Dent Assoc. 2000;131:613-20.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal changes in vertical and anterior displacement of the maxilla with bonded rapid palatal expansion appliances. Am J Orthod Dentofacial Orthop. 1989;95:462-6.
- [CrossRef] [Google Scholar]
- Arch dimensional changes concurrent with expansion in mixed dentition patients In: Trotman CA, McNamara JA Jr, eds. Orthodontic Treatment: Outcome and Effectiveness.Ann Arbor Craniofacial Growth Series Center for Human Growth and Development, the University of Michigan. 1995.
- [Google Scholar]
- A comparison of dentoalveolar inclination treated by two palatal expanders. Eur J Orthod. 2008;30:67-72.
- [CrossRef] [PubMed] [Google Scholar]
- Response of the midface to treatment with increased vertical occlusal forces. Treatment and posttreatment effects in monkeys. Angle Orthod. 1985;552:51-63.
- [Google Scholar]
- Orthodontics and Dentofacial Orthopedics Ann Arbor: Needham Press Inc.; 2001. p. :211-31.
- [Google Scholar]






