Translate this page into:
Effects of skeletal anchorage on mandibular rotation with fixed functional appliance therapy in class II malocclusion patients – A systematic review and meta-analysis

*Corresponding author: Aboli Jaydeep Muley, Department of Orthodontics and Dentofacial Orthopedics, Government Dental College and Hospital, Nagpur, Maharashtra, India. abolimuley@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Muley AJ, Chavan SJ, Bhad W, Shekokar SS, Khade DM. Effects of skeletal anchorage on mandibular rotation with fixed functional appliance therapy in class II malocclusion patients – A systematic review and meta-analysis. APOS Trends Orthod 2023;13:176-83.
Abstract
Objectives:
The study aimed to systematically investigate the effect of skeletal anchorage on mandibular rotation during FFA therapy during Class II correction in adolescents.
Material and Methods:
The review protocol was registered under the PROSPERO database (CRD42021256690). Electronic searches of databases and screening were performed up to May 2022. Only randomized clinical trials (RCT) and non-randomized controlled trials (non-RCT) were included in the study. Revised Cochrane risk-of-bias tool for RCTs (RoB 2) and risk of bias in non-randomized studies-of interventions tool for non-RCT were used for studies. Meta-analysis was performed and a forest plot was obtained. The primary outcome was mandibular rotation. Other outcomes assessed were angles SNA, SNB, ANB, mandibular incisor proclination, and failure rates of mini-screws and mini plates.
Results:
Twelve studies (eight RCTs and four non-RCTs) were included fulfilling inclusion criteria. Evidence showed a low-to-moderate risk of bias for different domains. Meta-analysis for mandibular rotation revealed a greater increase in mandibular plane angle in patients who received FFA with skeletal anchorage as compared to patients who did not receive skeletal anchorage.
Conclusion:
With or without skeletal anchorage, mandibular rotational changes during FFA therapy are similar. FFA when combined with skeletal anchorage causes more skeletal changes in sagittal parameters than conventional FFA used alone. FFA with skeletal anchorage reduces lower incisor proclination.
Keywords
Class II malocclusion
Fixed functional appliances
Mandibular rotation
Skeletal anchorage
INTRODUCTION
Angle’s Class II malocclusion caused by mandibular retrognathism is one of the most prevalent orthodontic issues, affecting a significant population. Using functional appliances on growing children, clinicians intend to change the profile and correct the malocclusion.[1] Fixed functional treatment is effective in treating Class II malocclusion with skeletal effects when performed during the pubertal growth phase.[2]
Protrusion of the mandibular incisors is an inherent effect of conventional fixed functional appliances (FFA) limiting its skeletal effects. Recently, to obtain more skeletal effects and to reduce lower incisor protrusion, temporary skeletal anchorage devices (TSADs) have been used in conjunction with FFAs. Various authors have concluded that adding skeletal anchorage (TSADs) produces more noticeable and superior results than traditional FFA.[3,4]
FFA therapy noticeably enhances soft tissues, profile, and chin prominence along with correction of malocclusion. These variables are linked to mandibular rotation and advancement. In the literature, no studies have investigated the effects of skeletal anchorage on mandibular rotation during FFA therapy. Therefore, this systematic review aimed to assess and compare mandibular rotational changes with or without TSADs in FFA.
MATERIAL AND METHODS
Protocol registration
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The review protocol was registered under the PROSPERO database (CRD42021256690).
Eligibility criteria
Inclusion criteria
Population
Healthy patients in the age group of 10–20 years with Angle’s Class II division 1 malocclusion were included in the study.
Intervention
FFA with skeletal anchorage (mini-screws/mini plates) to treat Class II malocclusion.
Comparison
Conventional FFA without skeletal anchorage.
Outcomes
Primary outcome: Skeletal change – Mandibular plane rotation – SN-MP (in degrees).
Other outcomes: Skeletal – Angles SNA, SNB, ANB, Dental – Mandibular incisor inclination (in degrees), the failure rate of TSADs.
Study designs
RCTs, prospective, controlled, and clinical trials and retrospective controlled clinical trials on humans with no restriction on the sample size.
Exclusion criteria
Patients undergoing pre-surgical orthodontics and patients with temporomandibular disorders were excluded from the study.
Study designs
Case reports, case series, review articles, editorials, commentaries, abstracts, retrospective studies, and laboratory studies.
Information sources, search strategy, and study selection
A literature search was performed using the database from PubMed, Central of the Cochrane library, Clinical Trials Registry, and Google Scholar. The database was searched till May 2022 with no specific filter applied during the search. Gray literature also was searched using a combination of MeSH terms and respective keywords. By looking through the included articles’ references, a further search was conducted. All articles were searched using the combination of keywords such as FFA, skeletal anchorage, and orthodontics with Boolean characters “AND” and “OR” combination.
The titles and abstracts of all relevant articles were screened by independent reviewers for inclusion. A study was judged eligible when it included the intervention of FFA with skeletal anchorage versus conventional FFA. Disagreements were resolved by discussion among the reviewers.
Data collection process and items
Data collection was performed using a customized data extraction form: (1) Author and year of study, (2) country, (3) type of study, (4) population – sample size, age, and gender, (5) intervention – FFA, skeletal anchorage, site of anchorage site, and failure rate, (6) comparator group – FFA, (7) treatment duration, and (8) outcomes [Table 1].
| S. No. | Author and Year | Country | Study design | Population | Intervention | Comparator/Control groups | Treatment duration | Outcome | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size | Age | Gender | FFA | Skeletal anchorage | Site of insertion | Failure of miniscrews/miniplates | |||||||
| 1. | Manni et al. 2012[5] | Italy | RCT | 50 I-25 C-25 |
11.8±1.7 years | M=27 F=23 |
Herbst | Miniscrews | Between 5 and 6 | Not mentioned | Standard Herbst | 7.5 months | Skeletal and dento-alveolar changes (Pancherz Analysis) |
| 2. | Aslan et al. 2014[6] | Turkey | RCT | 48 I-17 C-15 |
(13.68±1.6 years) I-13.68±1.09 years C-14.64±1.56 years Cl-14.13±1.50 years |
M=15 F=18 |
Forsus FRD | Miniscrews | Between 3 and 4 | Bilaterally in 2 patients (4/32) | Conventional Forsus FRD | 6.5 months | Skeletal and dento-alveolar changes, failure of TADs |
| 3. | Elkordy et al. 2016[7] | Egypt | RCT | 43 I-16 C-15 Cl-12 |
I-13.25±1.12 years C-13.07±1.14 years Cl-12.71±1.44 years |
F=43 | Forsus FRD | Miniscrews | Between 3 and 4 | 13% (4/30) |
C-Conventional Forsus FRD Cl-Untreated patients |
6.25 months | Skeletal, dentoalveolar changes, failure rate |
| 4. | Manni et al. 2016[13] | Italy | Retro-spective CCT | 60 I-EC-20 I-ML-20 C-20 |
11.6±1.9 years I-EC-11.9±1.7 years I-ML-11.6±2.4 years C-11.3±1.7 years |
M=32 F=28 |
Herbst | Miniscrews Group 1: EC Group 2: ML |
Between 4 and 5 or 5 and 6 | 8 in EC group and 6 in ML group | Standard Herbst | 7.4 months | Skeletal and dento-alveolar changes, failure rate |
| 5. | Turkkahraman et al.2016[8] | Turkey | RCT | 30 I-15 C-15 |
I-12.77±1.24 years C-13.26±0.82 years |
M=10 F=20 |
Forsus FRD | Miniplates | Anterior region of mandible | 9 % (3/32) |
Conventional Forsus FRD | 9.46 months | Skeletal, dento-alveolar and soft tissue changes, failure of TADs |
| 6. | Celikoglu et al.2016[14] | Turkey | Retro-spective CCT | 32 I-16 C-16 |
I-13.20±1.33 years C-13.56±1.27 |
M=13 F=19 |
Forsus FRD | Miniplates | Mandibular symphysis | Not mentioned | Herbst | 7.5 months | Skeletal, dentoalveolar changes |
| 7. | Eissa et al. 2017[9] | Egypt | RCT | 45 I-15 C-14 Cl-9 |
I-12.52±1.12 years C-12.76±1.0 years Cl-12.82±0.9 years |
M=17 F=28 |
Forsus FRD | Miniscrews | Between 3 and 4 | Not mentioned | C-Conventional Forsus FRD Cl-Untreated patients |
6.4 months | Skeletal, dentoalveolar changes |
| 8. | Elkordy et al. 2019[10] | Egypt | RCT | 48 I-16 C- 16 Cl- 16 |
I-12.5±0.9 years C-12.1±0.9 years Cl-12.1±0.9 years |
F=48 | Forsus FRD | Miniplates | Mandibular symphysis | 13.3 % | C-Conventional Forsus FRD Cl-Untreated patients |
7.26 months | Skeletal and dento-alveolar changes, failure of TADs |
| 9. | Manni et al. 2019[15] | Italy | Prospective CT | 26 I-13 C-13 |
I-12.8±1.5 years C-12.2±1.3 years |
M=13 F=13 |
Herbst | Miniscrews | Between 4–5 or 5–6 |
30.7% | Standard Herbst | 10.8 months | Skeletal, dentoalveolar changes |
| 10. | Gandedkar et al.2019[16] | Singapore and India | Prospective CT | 16 I-8 C-8 |
I-13.11 ± 0.38 years C-12.96±0.38 years |
F=16 | Forsus FRD | Miniplates | Anterior region of mandible | Not mentioned | C-Conventional Forsus FRD | 10.45 months | Skeletal, dentoalveolar and TMJ changes |
| 11. | Kochar et al. 2020[11] | India | RCT | 32 I-16 C-16 |
I-12.37±1.09 years C-12.06± 1.34 years |
M=17 F=15 |
Forsus FRD | Miniplates | Maxilla-above the apices of maxillary first molar Mandible - along the mandibular canine |
Not mentioned | C-Conventional Forsus FRD | 7.28 months | Skeletal, dentoalveolar changes |
| 12. | Pyarilal et al. 2021.[12] | India | RCT | 30 I-15 C-15 |
12–16 years | M=13 F=17 | Advansync2 | Miniscrews | Between mandibular canine and first premolar root area | Not mentioned | Advansync2 | 7.2 months | Skeletal, dentoalveolar changes |
Where RCT: Randomized clinical trial, CT: Controlled trial, FFA: Fixed functional appliance, I: Intervention, C: Comparator, Cl: Control, EC: Elastic chain, ML: Metallic ligature
Risk of bias
To evaluate the risk of bias in individual studies, different tools were used.
For RCTs, the assessment was conducted using the recommended approach in Cochrane Reviews using the software RevMan 5.4.1. The two-part tool was used to address the six specific domains (sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other bias).
For non-RCTs, the assessment was conducted using the recommended approach for assessing the risk of bias using the risk of bias in the non-randomized studies-of-interventions (ROBINS-I) tool. The two-part tool was used to address the seven specific domains (Bias due to confounding, selection of participants, classification of intervention, deviations from intended interventions, missing data, measurement of outcomes, and selection of the reported result).
Meta-analysis
The meta-analyses, using the random effects model, were applied with RevMan 5.4 (RevMan 5.4, The Nordic Cochrane Centre, Copenhagen). Data on the mean difference (MD) and standard deviation were obtained from selected studies. Heterogeneity was assessed by a Q test and quantified with I2 statistics. Mandibular rotation was considered the main outcome. In addition, a funnel plot was performed to evaluate the publication bias based on a sufficient number of included studies.
RESULTS
Study selection and characteristics
PRISMA guidelines were followed to scrutinize the articles as detailed in [Figure 1]. The database search and reference checks turned up a total of 186 documents. Ninety-seven records were chosen after the elimination of duplicates. After screening the titles and abstracts, 76 were excluded and 21 articles were selected. After further careful full-text review, nine studies were excluded due to different study designs, interventions, and comparators. Ultimately, 12 trials fulfilled the inclusion criteria and were selected.

- Preferred reporting items for systematic reviews and meta-analyses flow diagram.
Among the included studies, eight were RCTs[5-12] and four were controlled clinical trials (non-RCTs).[13-16]
Participants – There were 460 patients treated for Class II correction in included trials. Out of 460, 211 were treated using FFAs with skeletal anchorage, 190 using FFAs alone, and 59 served as untreated controls.
FFA used – Among the included studies, three investigated the effects of Herbst,[5,13,15] seven studies assessed the effects of Forsus fatigue resistant device (FRD),[6-11,16] one study assessed the effects of Advan-sync2,[12] whereas one study assessed the effects of Forsus versus Herbst.[14]
Skeletal anchorage used – In five studies, miniplates were used[8,10,11,14,16] and in seven studies, miniscrews were used.[5-7,9,12,13,15]
Outcomes – All studies evaluated skeletal and dentoalveolar changes before and after treatment. One study by Gandedkar et al.[16] evaluated changes using cone beam computed tomography. The remaining 11 studies had data from conventional lateral cephalograms.
Risk of bias results
While a majority of RCT studies showed a low risk of bias for research and few studies with questionable and high risk of biases. Five domains were assessed – including “bias in the randomization process (selection bias), “bias due to deviations from intended interventions,” “bias due to missing outcome data (attrition bias),” “bias in outcome assessment,” and “bias in selection of the reported result” [Figure 2].

- Risk of bias summary for the randomized clinical trials.
For the CCTs (non-RCTs), the risk of bias was performed following the ROBINS-Itool. Among non-RCTs, two studies by Manni et al.[13,15] showed a high risk of bias in domains of classification of intervention, bias due to deviation from intended outcome, and measurement of outcome. Other studies showed questionable and moderate risk of bias in few domains [Figure 3].

- Risk of bias summary for the non-randomized clinical trials.
Results of meta-analysis
For analyses, if the test showed substantial heterogeneity (I2 > 50%), a random effects model was applied, or else (I2 ≤ 50%), a fixed effects model would be used.
The meta-analysis was performed on 10 studies that qualified with the required data outcome that could be analyzed quantitatively. Out of these 10 studies, one study by Manni et al.[13] had two sub-groups; hence, data from these subgroups were considered as if it was data from two studies for analysis.
The other two studies[5,15] were excluded as the data reported could not be analyzed (data were not in MD and SD).
The results of the overall comparison have been depicted as a forest plot [Figure 4].

- Forest plot depicting results of meta-analysis of mandibular rotational changes.
Eleven sub-groups (studies) were included in the meta-analysis comparing mandibular rotation between FFAs with skeletal anchorage and conventional FFA alone. With the meta-analysis conducted for selected studies, heterogeneity was more than 50% (I2 = 83%); hence, the random effect model was applied.
Results showed that the mandibular rotation was more among FFA with skeletal anchorage group as compared to only the FFA group, with an MD of 0.39 (95% CI = −0.27–1.06; Z value = 1.16); However, the difference in mandibular rotation among two groups was statistically non-significant (P = 0.25).
Reporting bias assessment
The funnel plot shows the effect estimates of the included studies against their measure of precision or size of the studies. The shape of the funnel plot was asymmetrical between the right and the left sides, which means that there may be publication bias due to the absence of smaller-sized studies on the left side of the plot. The funnel plot showed asymmetry indicating heterogeneity and possible publication bias [Figure 5].
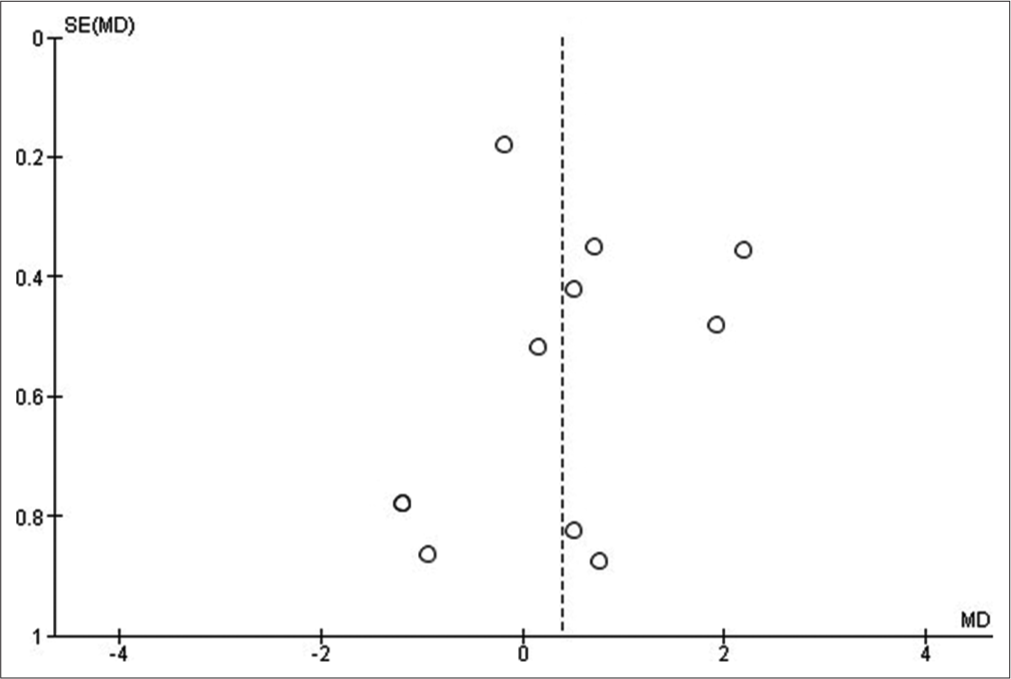
- Funnel plot.
DISCUSSION
FFA are effective bite-jumping treatment in the management of Class II malocclusion. FFA facilitates the forward and downward displacement of the mandible. Mandibular incisor proclination is the most pronounced dentoalveolar side-effect seen during fixed functional treatment.[17] It is of paramount importance to control this undesirable side effect. Skeletal anchorage has been proposed to enhance the effects of FFA and minimize common side effects like mandibular incisor proclination.
For this systematic review, 12 controlled and clinical trials were selected based on inclusion criteria. All these trials had an intervention of FFA with miniscrew/mini plates and a comparator of conventional FFA. The primary outcome assessed was mandibular rotation and other outcomes were skeletal changes in sagittal dimensions, dental effects in lower incisor proclinations, and failure rate of skeletal anchorage systems. A systematic review by Elkordy et al. in 2016[18] concluded that skeletal anchorage systems cause more skeletal effects than conventional FFA. However, this review was based on fewer studies. Hence, this more comprehensive review topic was undertaken including the latest trials.
Mandibular rotation
Meta-analysis showed that mandibular rotational changes with or without the use of skeletal anchorage were similar. Studies by Kochar et al.,[11] Manni et al.,[13] and Turkkahraman et al.[8] found that mandibular rotation was more in conventional FFA. However, seven studies[6,7,9,10,12,14,16] found that mandibular rotation was more in the skeletal anchored group than conventional FFA. When a forest plot was made using data from these studies, it showed that mandibular rotation was more in the skeletally anchored FFA group by 0.39°. However, this difference between the groups was statistically insignificant. The findings are similar to that of a review by Arvind and Jain.[3] where only four studies of Forsus FRD were included in the study.
Secondary outcomes assessed in this review were skeletal parameters – SNA angle, SNB angle, and ANB angle, which depict sagittal relations of the maxilla, mandible, and inter-jaw relationship. Nine studies that reported skeletal effects (angles SNA, SNB, and ANB in degrees) were selected for qualitative analysis.
SNA angle
Evidence depicted that the patients treated with FFA combining skeletal anchorage had no significant difference in the change in SNA angle. This indicates that skeletally anchored FFAs do not exhibit superior inhibition of maxillary growth.
SNB angle
Compared with FFA alone, patients treated with FFA with skeletal anchorage had a significant difference in the change in SNB angle demonstrating that using FFA in combination with TSADs gains more mandibular advancement. This is consistent with reviews found in the literature.[3,4,18]
ANB angle
When compared with FFA alone, patients treated with FFA with skeletal anchorage had a significant difference in the change in the ANB angle indicating that a favorable effect on the skeletal relationships between the maxilla and mandible can be achieved using FFA with skeletal anchorage.
The inclination of the lower incisors
Major Class II correction with FFAs takes place due to lower incisor proclination in conventional FFA. Evidence synthesis suggests – patients treated with FFA with skeletal anchorage had a significant difference in the change in the lower incisor inclination angle. This indicates that skeletal anchorage has a significant impact on reducing lower incisor proclination. TSADs potentially inhibit side-effect of conventional FFAs.
Failure rate
All participants in included trials were growing children belonging to the age group of 10–20 years. Hence, invasiveness was a limitation owing to the immature bone during growth years. However, only six trials[6-8,10,13,15] with low failure rates reported TSADs failure. Thus, evidence suggested that the skeletal anchorage system can effectively be applied in combination with FFA in adolescent patients.
Strengths and limitations
This is a comprehensive review based on the latest clinical trials. The data were retrieved from electronic database. No filter was applied regarding the timeline. Only a language filter was used to remove evidence that was not available in English. All included trials used the same intervention and comparator, as specified in the inclusion criteria, which improved the data comparability. All studies were considerably recent. This made the conclusions clinically relevant and applicable.
However, some limitations must be mentioned. In all included studies, sites of TSADs placement were not uniform. Radiographic facilities and parameters were not uniform. Furthermore, manual tracing of lateral cephalograms could not be rendered error-free. Heterogeneity existed among the included studies. Several patient-related factors such as gender, race, and skeletal maturation stages could not be formally assessed in this review.
CONCLUSION
According to existing evidence, the following conclusions can be drawn regarding the effectiveness of the use of skeletal anchorage with FFAs:
With or without skeletal anchorage, mandibular rotational changes during FFA therapy are similar.
FFA when combined with skeletal anchorage causes more skeletal changes in sagittal parameters than conventional FFA used alone.
Adding skeletal anchorage effectively reduces the lower incisor proclination during FFA therapy.
Skeletal anchorage systems (TSADs) may be used in adolescent children during FFA treatment with utmost consideration of developing bone and knowledge of managing risks anticipated.
The findings of this review need to be interpreted cautiously. Standardization regarding participants’ age, gender, skeletal maturity parameters, type of FFA, and site of TSADs is needed in upcoming trials examining the efficiency of FFA with skeletal anchorage systems. Future research in well-designed controlled clinical settings is necessary to comprehend the stability and long-term effects of skeletal anchorage systems.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The use of functional appliances in contemporary orthodontic practice. Br Dent J. 2015;218:123-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment effects of fixed functional appliances alone or in combination with multibracket appliances: A systematic review and meta-analysis. Angle Orthod. 2015;85:480-92.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletally anchored forsus fatigue resistant device for correction of Class II malocclusions-A systematic review and meta-analysis. Orthod Craniofac Res. 2021;24:52-61.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of fixed functional appliances with temporary anchorage devices on Class II malocclusion: A systematic review and meta-analysis. J World Fed Orthod. 2021;10:59-69.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between Herbst appliances with or without miniscrew anchorage. Dent Res J (Isfahan). 2012;9:S216-21.
- [Google Scholar]
- Treatment effects of the forsus fatigue resistant device used with miniscrew anchorage. Angle Orthod. 2014;84:76-87.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional effects of the mini-implant-anchored forsus fatigue resistant device: A randomized controlled trial. Angle Orthod. 2016;86:292-305.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of miniplate anchored and conventional forsus fatigue resistant devices in the treatment of Class II malocclusion. Angle Orthod. 2016;86:1026-32.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcomes of Class II malocclusion cases treated with miniscrew-anchored forsus fatigue resistant device: A randomized controlled trial. Angle Orthod. 2017;87:824-33.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the miniplate-anchored forsus fatigue resistant device in skeletal Class II growing subjects: A randomized controlled trial. Angle Orthod. 2019;89:391-403.
- [CrossRef] [PubMed] [Google Scholar]
- Management of skeletal Class II malocclusion using bimaxillary skeletal anchorage supported fixed functional appliances : A novel technique. J Orofac Orthop. 2021;82:42-53.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of the skeletal effects of Advansync2 and Advansync2 used with Miniscrew anchorage. Ann Romanian Soc Cell Biol. 2021;25:20874-82.
- [Google Scholar]
- Herbst appliance anchored to miniscrews with 2 Types of ligation: Effectiveness in skeletal Class II treatment. Am J Orthod Dentofacial Orthop. 2016;149:871-80.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment effects of skeletally anchored Forsus FRD EZ and Herbst appliances: A retrospective clinical study. Angle Orthod. 2016;86:306-14.
- [CrossRef] [PubMed] [Google Scholar]
- Herbst appliance anchored to miniscrews in the upper and lower arches vs standard Herbst: A pilot study. Am J Orthod Dentofacial Orthop. 2019;156:617-25.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of conventional and skeletal anchorage system supported fixed functional appliance on maxillo-mandibular complex and temporomandibular joint: A preliminary comparative cone beam computed tomography study. Int Orthod. 2019;17:256-68.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical effects of fixed functional appliance on craniofacial structures. Angle Orthod. 2009;79:668-75.
- [CrossRef] [PubMed] [Google Scholar]
- Can the use of skeletal anchors in conjunction with fixed functional appliances promote skeletal changes? A systematic review and meta-analysis. Eur J Orthod. 2016;38:532-45.
- [CrossRef] [PubMed] [Google Scholar]







