Translate this page into:
Evaluation of apical root resorption in Class III patients who received one- or two-phase orthodontic treatment

*Corresponding author: Elif Dilara Seker, Department of Orthodontics, Bezmialem Vakif University, Fatih, Istanbul, Turkey. dilaraarsln@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Seker ED, Yilmaz BS, Yagci A. Evaluation of apical root resorption in Class III patients who received one- or two-phase orthodontic treatment. APOS Trends Orthod 2021;11(2):123-31.
Abstract
Objectives:
The aim of this study was to compare the incidence root resorption and dilaceration between the patients with and without previous orthopedic treatment after the fixed orthodontic treatment.
Materials and Methods:
The pre- and post-treatment digitized panoramic films of 40 Class III adult patients meeting the inclusion criteria were selected from patient population of the orthodontic department. Half of the patients were treated with two-phase treatment (orthopedic therapy followed by fixed appliance treatment; Group 1), while the others wore only fixed appliances (Group 2). Root resorption was evaluated from the first molar to the first molar for each arch using the ImageJ software (Bethesda, Maryland, USA). The presence of root dilacerations was also recorded on the pre-treatment panoramic radiographs. Paired samples t-test and Mann– Whitney U-test were used to compare root length.
Results:
Intragroup comparisons for each tooth indicated that the upper and lower incisors, first molars and upper left second premolars presented a significant decrease in Group 1 (P < 0.05). In contrast, in Group 2, a significant decrease in tooth length was found only in the upper incisors (P < 0.05). Intergroup comparisons for root length change indicated statistically significant differences for the lower incisors, upper second premolars, and all first molars except for the upper left molars (P < 0.05). Nevertheless, the prevalence of root dilaceration in Group 1 was higher than that in Group 2.
Conclusion:
Class III patients who received two-phase treatments experienced more root resorption and dilaceration compared with patients who received one-phase treatments. It should be remembered that early orthopedic forces may have potential adverse effects on a dental root in the long-term.
Keywords
Angle Class III
Root resorption
Orthodontics
INTRODUCTION
The prevalence of Class III malocclusions varies between 0% and 26.7% in different racial and ethnic groups.[1] There are alternative treatment options that may be chosen based on the etiology of Class III malocclusion and the growth-stage of the patient. The orthopedic treatment of Class III malocclusions includes the use of chin cups, functional appliances, and reverse headgears (RHg) in the early period.[2,3] Maxillary transverse discrepancy frequently exists in patients with Class III malocclusion. Therefore, the combination of rapid maxillary expansion (RME) and RHg is often used to treat Class III skeletal malocclusion related to maxillary retrognathia in growing patients.[4] Non-growing patients who have a recurrent Class III malocclusion or adult patients who request orthodontic treatment in the late period for correction of a mild skeletal Class III malocclusion may be treated with fixed orthodontic treatment.[5] In this camouflage treatment, the teeth are subjected to orthodontic forces generated by Class III elastics during late correction.[3,6] Although there is a general idea that heavy forces lead to interruption of root development in teeth with incomplete root formation, the potential side effects of orthopedic treatment using RME&RHg are not well documented in the literature.[7] A previous study[8] reported that heavy orthopedic forces interrupt root development in the mixed dentition period, and the combination of RME&RHg treatment is a possible risk factor for future root resorption. Root resorption due to orthodontic treatment is a pathological condition that is characterized by loss of the superficial layer of the cells of tooth roots.[9] To diagnose the root resorption, radiographic examination is required. Conventional radiographs such as periapical and panoramic X-rays and cone-beam computed tomography (CBCT) are commonly used to quantify root resorption.[10]
Furthermore, it was also reported that heavy orthodontic forces have negative effects such as dilacerations on root formation of teeth with immature roots in mixed dentition. Dilacerations are considered to result from traumatic displacement of already formed hard tissue. This is because any traumatic force can affect the non-calcified part of tooth germ and lead to formation of roots at an abnormal angle.[11]
In this context, considering that an orthodontic force is a controlled trauma, it is reasonable to conclude that the combination of RME&RHg treatment that is often used in pediatric patients with incomplete root formations may increase the possibility of root resorption during fixed orthodontic treatment. The first aim of the study was to compare the incidence and amount of apical root resorption radiographically between the adult patients with and without previous orthopedic treatment after the fixed orthodontic treatment. The second aim of this study was to evaluate whether early orthopedic forces affect the prevalence of root dilacerations. The null hypothesis of this study was that there is no significant difference in the dental root length/ dilaceration between two-phase treatment with RME&RHg followed by fixed appliance treatment and conventional fixed orthodontic treatment.
MATERIALS AND METHODS
This retrospective study was approved by the Local Ethics Committee of the Bezmialem Vakif University. The patients were selected from records of the archives of the orthodontic department at Bezmialem Vakif University. The inclusion criteria as follows: (1) Patients with mild Class III malocclusion who had a previous RME&RHg treatment history (Petit type RHG with full-coverage bonded RME appliance) or did not have previous RME&RHg treatment history, (2) end-to-end incisor relationship at the beginning of the fixed orthodontic treatment with the straight-wire edgewise technique, (3) orthodontic treatment without extraction of permanent teeth, (4) permanent dentition, (5) teeth at Nolla stages 9 and 10 (upper and lower incisors, canines, premolars and first molars), and (6) available preand post-treatment radiographic records. Patients with any systemic and metabolic disease or craniofacial syndrome, any history of trauma in early childhood, root-canal treatment, apical lesions, missing teeth, and poor-quality radiographs were excluded from the study.
The radiographic records of a total of 76 individuals were obtained from patient population of the orthodontics department based on the inclusion criteria at first. After application of the exclusion criteria, forty patients (17 girls and 23 boys) were included in the study. All patients had been treated with fixed orthodontic appliances from 2014 to 2018. Twenty patients (8 girls and 12 boys) had been treated with RME&RHg appliances in the past [Group 1]. The mean age was 8.32 ± 2.1 years at the initial orthopedic treatment with RME&RHg, and the mean treatment time was 9.1 ± 1.1 months. These patients had a mean age of 12.48 ± 1.03 years at the start of the fixed orthodontic treatment, and the mean duration of the fixed treatment was 24.6 ± 6.56 months. The upper and lower permanent incisors and first molars had erupted in these patients. However, the upper and lower permanent canines and premolars had not erupted.
The other twenty patients (9 girls and 11 boys) were only treated with fixed orthodontic appliances (Group 2). The RME procedure was not performed in the Group 2 patients. They had a mean age of 13.28 ± 1.45 years at the beginning of fixed orthodontic treatment. The mean orthodontic treatment time was 23.28 ± 6.68 months.
The demographic characteristics of the treatment groups are presented in [Table 1]. Initial and final cephalometric variables of the patients are presented in [Table 2].
| Group 1 | Group 2 | P-value | |
|---|---|---|---|
| Sex | |||
| Boys (n%) | 12 (60%) | 11 (55%) | NS |
| Girls (n %) | 8 (40%) | 9 (45%) | NS |
| Mean age (year)±sd | 12.48±1.03 | 13.28±1.45 | NS |
| Mean treatment time (month) | 24.6 ± 6.56 | 23.28±6.68 | NS |
| ΔU1-SN | 3.22±6.2 | 3.7±5.01 | NS |
| ΔIMPA | –2.37±7.1 | –3.3±6.4 | NS |
sd: Standard deviation, NS: Insignificant, t1: Pre-treatment, t2: Posttreatment, ΔU1-SN: The change of the angle between upper incisors and sella-nasion plane from t1 to t2; ΔIMPA: The change of the angle between lower incisor and mandibular plane from t1 to t2
| Variables | Group 1 | Group 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| t1’ | t2’ | P-value | t1 | t2 | P-value | t1 | t2 | P-value | |
| Mean±sd | Mean±sd | Mean±sd | Mean±sd | Mean±sd | Mean±sd | ||||
| SNA | 79.1±3.6 | 81.5±3.9 | 0.03 | 81.3±4.3 | 80.9±4.1 | NS | 80.3±3.4 | 79.9±3.6 | NS |
| SNB | 81.1±3.4 | 81.5±3.9 | NS | 81.9±3.8 | 82±3.6 | NS | 81.4±3.1 | 81.1±3.4 | NS |
| ANB | –2±1.8 | 0±2.1 | 0.01 | –0.6±2.1 | –1.1±1.9 | NS | –1.1±3 | –1.2±3.1 | NS |
| SNGoGn | 35.6±5.8 | 37.4±6.1 | 0.04 | 35.8±7 | 36.1±6.8 | NS | 34.7±2.8 | 36.3±2.3 | NS |
| U1-SN | 106±6.7 | 108±6.1 | 0.03 | 110.7±5.7 | 113.3±6.3 | 0.04 | 108.2±5.1 | 111.9±5.8 | 0.01 |
| IMPA | 87.3±4.9 | 85.7±6.9 | NS | 84.4±5.1 | 81.03±4.5 | 0.02 | 85.7±5.5 | 82.4±3.07 | 0.03 |
sd: Standard deviation, NS: Insignificant, t1’: At the beginning of the RME&RHg treatment, t2’: At the end of the RME&RHg treatment, t1: At the beginning of the fixed orthodontic treatment pre-treatment, t2: At the end of the fixed orthodontic treatment
Power analysis revealed that a sample size of twenty patients would provide more than 95% power to detect significant differences with an effect size of 0.80 and on a significance level of α = 0.05.
The RME&RHg treatment protocol was as follows (based on data from the patients’ files): A full coverage acrylic cap splint type RME appliance (tooth-tissue borne and full occlusal coverage) was used for rapid maxillary expansion (activation of the screw 2 times a day). The active expansion was maintained until an overcorrection of the maxillary constriction was obtained. After opening sutures, an elastic force of 350–500 g (per side) was applied to the hooks on the rapid maxillary expander from the Petit-type RHg. The active RHg therapy was completed when a positive overjet was reached.
The patients were treated with the same protocol with fixed conventional brackets (Roth prescription, 0.018-inch slot) and general arch-wire sequences of 0.014-inch nickel-titanium to 0.016 × 0.022-inch stainless steel (G&H Orthodontics, Franklin, Ind). First, both maxillary and mandibular teeth were aligned. After leveling, 0.016 × 0.022-inch stainless steel arch-wires were placed, and Class III elastics were applied from lower canine brackets to the upper first molar bands until a Class I dental relationship was achieved.
Radiographic examinations
Pre-treatment (t1-the beginning of the fixed orthodontic treatment) and post-treatment (t2-the end of the fixed orthodontic treatment) radiographs had been taken by the same device (Planmeca ProMax, Helsinki, Finland) and the same standardized method. All measurements were performed by the same operator. The operator was blinded to the patients’ treatment history to reduce bias in the results of the study. Another operator set up the blinding process using a different identification letter code for each radiograph.
Cephalometric analysis
Changes in anterior teeth inclination related to treatment outcomes may cause shorter or longer root lengths on panoramic radiographs than actual root dimensions.[12] Therefore, the cephalometric radiographs of the 40 patients were analyzed using the Dolphin Imaging Program (Version10.0, Dolphin Imaging Software, Calif). U1-SN (the axial inclination of the upper incisors to the sella-nasion plane) and IMPA (the axial inclination of the mandibular incisors to the mandibular plane) measurements were recorded to analyze the changes in the inclination of the incisors during the fixed treatment.
Panoramic analysis
Digitized panoramic radiographs were imported into the image analysis software (ImageJ software1.37, Maryland, USA). Calibration of measurements was performed using Set Scale in the ImageJ toolbar. First, a known distance was measured using the straight-line tool in the ImageJ toolbar. After this, the known distance was entered into the corresponding box of Set Scale. When the setting procedure was completed, the program automatically calculated the distance based on the registered distance (16.07 pixels/ mm). Root resorption was assessed on the upper and lower incisors, canines, premolars, mesio-buccal roots of the upper first molars, and distal roots of the lower first molars. The mesiobuccal roots of the upper first molars were included in the study since buccal root measurement was simple, reproducible and more reliable, unlike the palatal and distobuccal roots.[13] A previous study[14] reported that distal roots of lower molars showed more root resorption. Therefore, the distal roots of lower first molars were included to evaluate the root resorption in the lower molars. The closest linear distance from the center of the incisal border or the cusp tip to the root apex was used for root length measurements [Figure 1]. Differences of magnification among the preand post-treatment panoramic films were calculated and corrected using the formula below [Figure 2]. This technique was recommended by Linge and Linge[15] (1983) at first and then its accuracy was confirmed by Blake et al.[16]
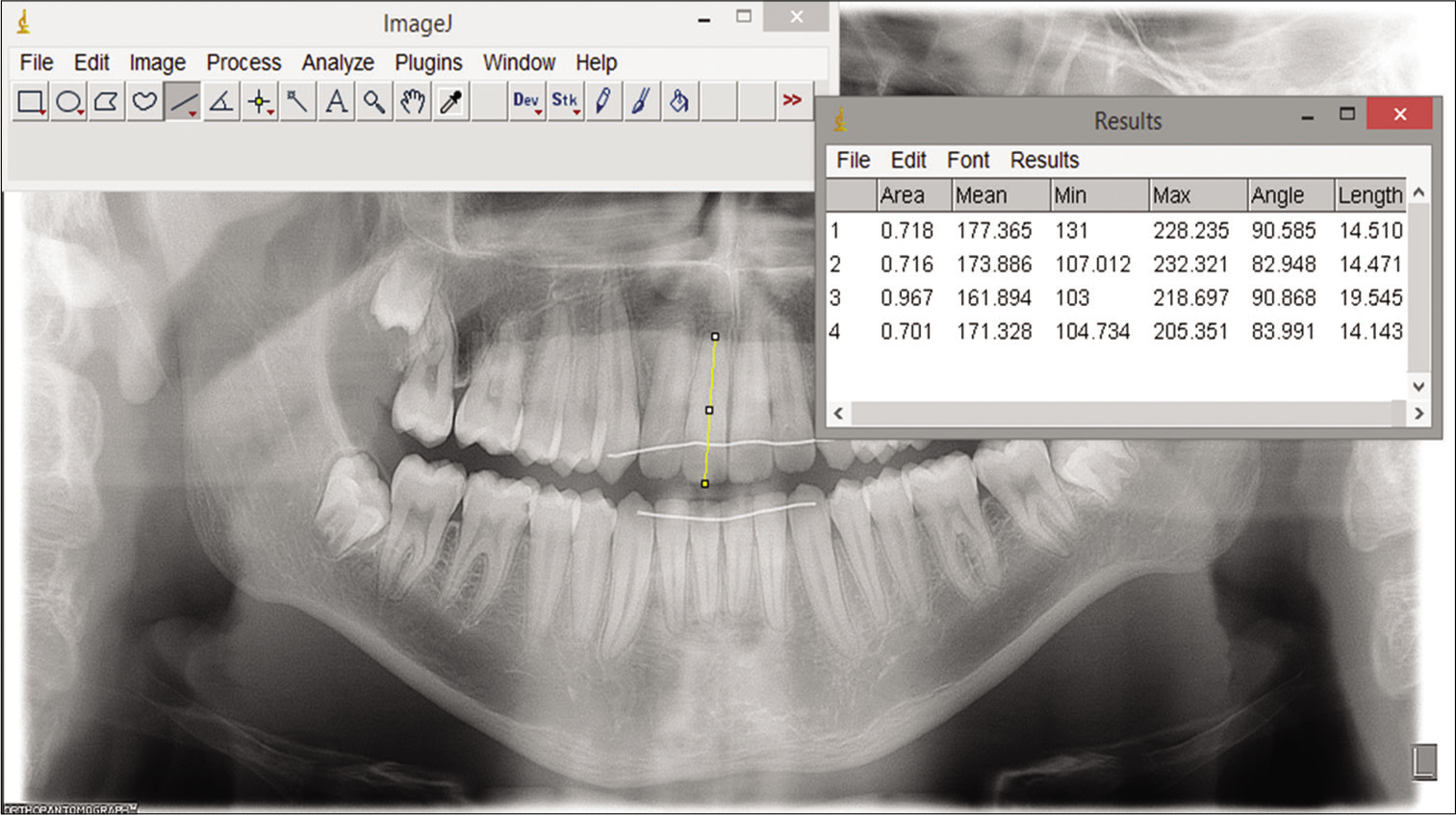
- Measurement of tooth length on digitized panoramic radiograph with the ImageJ software.

- Measurements for calculation of magnification differences between panoramic at t1 and t2 images and establishment of the correction Formula (C=Crown length, TL=Tooth length, CEJ=Cementoenamel junction).
Correction formula of root length value:
Change of root length value (t2–t1) = TL2–TL1c
C1: Radiographic crown length at t1; C2: Radiographic crown length at t2; TL1: Radiographic total tooth length at t1; TL2: Radiographic total tooth length at t2; TL1C: Corrected TL1
In addition, the presence of root dilacerations was also recorded on the pre-treatment panoramic films for both groups. In this study, if a tooth had mesial or distal deviation of ≥20 from the long axis of the tooth (the axial inclination between the crown and the root of a tooth), this tooth was considered to have root dilaceration.[17]
Statistical analysis
The data were tested for normality using Shapiro–Wilk test. Independent-samples t-tests were used for comparison of the descriptive parameters. Paired-samples t-test was used for comparison of the tooth length between t1 and t2. Mann– Whitney U-test was used to compare the change in the tooth length value between the groups. Ten panoramic films (240 teeth) were reassessed after 3 weeks to evaluate intra-observer reliability using Dahlberg’s formula.[18] As a result, the method error was insignificant (P = 0.08).
RESULTS
The two treatment groups were well matched for age, sex, and mean fixed orthodontic treatment duration. A total of 960 tooth lengths were measured for this study. The descriptive data are presented in [Table 1].
Results of tooth length measurements
Group 1 included the patients who had worn RME&RHG in the early period and were then treated with fixed orthodontic appliances. The comparison of the mean tooth length between t1 and t2 for each tooth indicated that the upper and lower incisors, first molars, and the upper left second premolars presented a significant decrease [P < 0.05, Table 3]. Group 2 consisted of the patients treated by one-phase fixed appliance treatment. In Group 2, a significant decrease in tooth length was found only in the upper incisors [P < 0.05, Table 3].
| Group 1 | Group 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t1 | t2 | P-value | t1 | t2 | P-value | |||||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | |||||||
| 16 | 15.5 | 1.8 | 14.9 | 1.8 | 0.02 | 14.3 | 0.9 | 14.4 | 1 | NS |
| 15 | 15.8 | 2.3 | 15.4 | 2 | NS | 15.6 | 1.2 | 15.6 | 1.3 | NS |
| 14 | 16.1 | 2.7 | 15.8 | 2.5 | NS | 15.7 | 1.2 | 15.6 | 1.1 | NS |
| 13 | 20.2 | 3.2 | 20.5 | 2.6 | NS | 19.5 | 2 | 20 | 2 | NS |
| 12 | 17 | 1.9 | 15.7 | 1.7 | <0.001 | 16.2 | 1.7 | 15.4 | 1.8 | 0.006 |
| 11 | 18.1 | 2 | 16.8 | 2.2 | <0.001 | 17.2 | 1.3 | 16.5 | 1.3 | 0.003 |
| 21 | 18 | 2 | 17 | 1.9 | <0.001 | 17.1 | 1.3 | 16.5 | 1.3 | 0.007 |
| 22 | 16.8 | 1.9 | 15.9 | 2.2 | 0.008 | 16.5 | 1.8 | 15.4 | 1.9 | <0.001 |
| 23 | 20.4 | 2.6 | 20.1 | 2.4 | NS | 19.4 | 2 | 19.7 | 1.9 | NS |
| 24 | 15.8 | 2 | 15.6 | 2.1 | NS | 15.7 | 1 | 15.9 | 1 | NS |
| 25 | 15.9 | 1.9 | 15.4 | 1.5 | 0.02 | 15.6 | 1.3 | 15.6 | 1.5 | NS |
| 26 | 15.6 | 1.5 | 15.1 | 1.6 | 0.01 | 15.1 | 1.1 | 14.9 | 1.3 | NS |
| 36 | 17.3 | 1.8 | 16.7 | 2.1 | 0.01 | 15.9 | 1 | 15.8 | 1.2 | NS |
| 35 | 16.4 | 1.9 | 16.4 | 2.1 | NS | 16 | 0.8 | 15.9 | 1.2 | NS |
| 34 | 16.5 | 1.7 | 16.3 | 2 | NS | 16.5 | 0.9 | 16.2 | 1.2 | NS |
| 33 | 18.9 | 1.9 | 18.5 | 2.2 | NS | 17.6 | 1.5 | 17.7 | 1.8 | NS |
| 32 | 16.5 | 1.7 | 15.3 | 1.7 | 0.002 | 14.9 | 1.5 | 14.8 | 1.2 | NS |
| 31 | 15.8 | 1.7 | 14.5 | 1.6 | 0.001 | 14.2 | 1.2 | 14 | 0.9 | NS |
| 41 | 15.7 | 2 | 14.1 | 1.6 | 0.001 | 14.1 | 1.1 | 14 | 0.8 | NS |
| 42 | 16.4 | 1.8 | 15.1 | 1.5 | <0.001 | 14.9 | 1.2 | 14.8 | 1.2 | NS |
| 43 | 18.4 | 1.9 | 18.1 | 2.2 | NS | 17.4 | 1.4 | 17.6 | 1.3 | NS |
| 44 | 16.8 | 1.9 | 16.5 | 1.7 | NS | 16.2 | 1 | 15.9 | 1.2 | NS |
| 45 | 16.7 | 2 | 17.4 | 1.7 | NS | 16.1 | 1 | 16.3 | 1.1 | NS |
| 46 | 17.4 | 1.9 | 16.8 | 2.1 | 0.01 | 16 | 0.73 | 16.02 | 1.04 | NS |
Mean value is the tooth length in millimeter; SD: Standard deviation, t1: Pre-treatment, t2: Post-treatment, NS: Insignificant
Comparison of the tooth length change (from t1 to t2) between the groups
[Table 4] reports the significant differences in changes in the tooth lengths between Group 1 and Group 2. The patients treated in two phases with RME&RHG and fixed appliances (Group 1) had more root shortening in the lower incisors, upper second premolars and all first molars except for the upper left molar than the patients treated by one-phase fixed appliance treatment (Group 2, P < 0.05).
| Group 1 (n=20) | Group 2 (n=20) | P-value | |||
|---|---|---|---|---|---|
| t2−t1 | t2−t1 | ||||
| mean±SD | mean±SD | ||||
| 16 | –0.58 | 1.1 | 0.1 | 0.49 | 0.004 |
| 15 | –0.39 | 0.9 | –0.04 | 0.42 | NS |
| 14 | –0.3 | 1.4 | –0.1 | 0.57 | NS |
| 13 | 0.2 | 1.78 | 0.4 | 1.11 | NS |
| 12 | –1.23 | 1.08 | –0.78 | 1.12 | NS |
| 11 | –1.26 | 1.22 | –0.69 | 0.93 | NS |
| 21 | –1.05 | 0.97 | –0.58 | 0.85 | NS |
| 22 | –0.89 | 1.34 | –1.13 | 1.13 | NS |
| 23 | –0.28 | 1.6 | 0.31 | 1.01 | NS |
| 24 | –0.19 | 1.06 | 0.17 | 0.81 | NS |
| 25 | –0.5 | 0.94 | 0.03 | 0.86 | 0.03 |
| 26 | –0.54 | 0.89 | –0.21 | 0.82 | NS |
| 36 | –0.59 | 0.94 | –0.04 | 0.71 | 0.04 |
| 35 | –0.04 | 0.94 | –0.08 | 0.76 | NS |
| 34 | –0.21 | 0.93 | –0.24 | 0.77 | NS |
| 33 | –0.39 | 1.38 | 0.02 | 0.99 | NS |
| 32 | –1.15 | 1.34 | –0.08 | 0.81 | 0.005 |
| 31 | –1.35 | 1.32 | –0.16 | 0.67 | 0.001 |
| 41 | –1.53 | 1.6 | –0.17 | 0.72 | 0.002 |
| 42 | –1.26 | 1.29 | –0.08 | 0.62 | 0.001 |
| 43 | –0.31 | 1.49 | 0.21 | 0.83 | NS |
| 44 | –0.27 | 0.74 | –0.24 | 1.05 | NS |
| 45 | –0.01 | 1.03 | 0.16 | 0.62 | NS |
| 46 | –0.56 | 0.97 | 0.02 | 0.49 | 0.01 |
Mean value is the tooth length in millimeter; SD: Standard deviation, t1: Pre-treatment, t2: Post-treatment, NS: Insignificant
Incidence of root dilacerations in the groups
In Group 1, a total of 33 out of 480 teeth were diagnosed as being dilacerated teeth (6.7%). The upper lateral incisors were the most frequently dilacerated teeth (35%), followed by the upper first premolar, lower canine, and first premolar teeth [Table 5].
| Group 1 | Group 2 | |||||
|---|---|---|---|---|---|---|
| Number of teeth examined | Number of total dilaceration | Dilaceration percentage | Number of teeth examined | Number of total dilaceration | Dilaceration percentage | |
| Maxillary | ||||||
| Central incisor | 40 | 1 | 2.5 | 40 | 0 | 0 |
| Lateral incisor | 40 | 14 | 35 | 40 | 1 | 2.5 |
| Canine | 40 | 3 | 7.5 | 40 | 0 | 0 |
| First premolar | 40 | 4 | 10 | 40 | 3 | 7.5 |
| Second premolar | 40 | 2 | 5 | 40 | 2 | 5 |
| First molar | 40 | 0 | 0 | 40 | 0 | 0 |
| Mandibular | ||||||
| Central incisor | 40 | 0 | 0 | 40 | 0 | 0 |
| Lateral incisor | 40 | 0 | 0 | 40 | 0 | 0 |
| Canine | 40 | 4 | 10 | 40 | 0 | 0 |
| First premolar | 40 | 4 | 10 | 40 | 0 | 0 |
| Second premolar | 40 | 1 | 2.5 | 40 | 0 | 0 |
| First molar | 40 | 0 | 0 | 40 | 0 | 0 |
| Total | 480 | 33 | 6.87 | 480 | 6 | 1.25 |
In comparison, root dilaceration was observed in six out of a total of 480 teeth in Group 2 (1.25%). The maxillary first premolars (7.5%) were the most frequently dilacerated teeth. In Group 1, a total of 14 out of 20 patients had at least one dilacerated tooth. On the other hand, root dilaceration was detected in only four out of 20 patients in Group 2.
DISCUSSION
There is substantial evidence in the literature to support that heavy forces lead to an increase in root resorption risk due to creation of high-level stresses on the periodontal ligament.[19,20] However, there are still unidentified risk factors for root resorption.[21,22] Considering that RME&RHg therapy is usually performed in pediatric patients, who still have immature roots, little is known about the long-term possible negative effects of the treatment such as root resorption on teeth.[8,23,24] To the best of our knowledge, no previous study has been published on the relationship between formation of root resorption during fixed orthodontic treatment and past RME&RHg therapy.
We evaluated the change of root length on panoramic radiographs in this study. It was reported that panoramic radiographs provide sufficiently accurate information for linear measurements of root length at different time points.[25] CBCT has high accuracy to detect changes in root length.[26] On the other hand, CBCT imaging may deliver more ionizing radiation doses than panoramic radiography. Adolescents are more susceptible to develop breast and thyroid gland cancer than adults due to the continuing development of tissues, and even very low doses may cause development of malignancy in children and adolescents.[27] Because certain relationships between radiation dose and its biological harm are poorly understood, clinicians should apply the ALARA principles (the concept of “as low as” reasonably achievable) in clinical practice.[27] The correction formula of root length value was used to eliminate the magnification differences between the panoramic radiographs at t1 and t2, similar to the previous studies in the literature.[8,15,16]
The changes in the inclinations of the upper and lower incisors related to fixed orthodontic treatment outcomes may cause shorter or longer root length seen on panoramic radiographs than the actual length.[8] Therefore, the changes in the inclination of the maxillary and mandibular incisors from T1 to T2 were calculated. Since no statistically significant differences were observed in the change of inclination between the groups, it was considered that the change in the inclination of the incisors had no influence on the root length measured on the panoramic radiographs.
We assessed a total of 960 tooth lengths quantitatively using the ImageJ program (version 1.37, National Institutes of Health, Bethesda, Maryland, USA). The upper incisors are more susceptible to root resorption than other teeth during orthodontic treatment, and these are followed by lower incisors and first molars.[15,26,28] Similarly to these findings, the intragroup comparisons showed that the upper central and lateral incisors had root shortening in both groups.[29] We found that root resorption was observed in the upper and lower incisors, first molars and upper left second premolars of the patients who had previously been treated with RME&RHg (Group 1), and this finding was in accordance with what was reported by Castro et al.[30] However, in the patients with no previous RME&RHg therapy, root resorption was observed only in the upper incisors after fixed orthodontic treatment (Group 2).
The intergroup comparison of the root length changes related to treatment outcomes revealed that lower incisors, upper second premolars, and all first molars except for the upper left molars in Group 1 had more root shortening than those in Group 2. De Rossi et al.[31] reported that the occlusal thickness of an acrylic expander leads to an increase in the activity of chewing muscles in both a resting position and habitual mastication. A possible explanation for the increased root resorption in the lower incisors in Group 1 could be forces transmitted to these teeth due to an increase in chewing muscle activity during the RME&RHg treatment. The lingually directed force application on the level of mandibular incisor roots by chin pad of the RHg could be another possible reason of the root resorption.
The RME&RHg treatment transmits heavy forces to permanent teeth directly or through deciduous teeth and it generates high-level stresses on periodontal tissues, and this may negatively influence the dental root development process.[8] The long-term effects of such an orthopedic force applied in the early period may include disorders of root development such as root dilacerations and increased risk of root resorption.[8,32] Therefore, the significant increase in root resorption of the patients treated in two phases could be explained by the potential long-term effects of heavy orthopedic forces.
In terms of root resorption, significant differences were found between the groups in almost all first molars, unlike the premolars in this study. It is known that the survival rate of traumatized teeth with immature roots is higher than traumatized teeth with mature roots after a trauma.[33] However, while the root formation of the first molars is completed by the age of 8 years, the roots of the premolars may continue to develop by the age of 13 years.[34] In this study, the mean age at the time of orthopedic treatment was 8.32 ± 2.1 years. The differences in the root resorption response after fixed orthodontic treatment between the molars and the other posterior teeth that include the canine and premolar teeth could be attributed to their developmental stage of roots at the beginning of the RME&RHg treatment. Therefore, a possible reason could be that the molar teeth that have more mature roots may not tolerate the heavy forces effectively unlike the premolars with a wide-open apex during orthopedic treatment.
Premature arrest of root development of unerupted teeth following dento-periodontal trauma on its primary predecessor may lead to root dilaceration. The wide range of the prevalence of dilaceration (0.42–98%) in the literature results from various definitions of root dilaceration.[32] Our results indicated that the prevalence of root dilaceration was greater in Group 1 (6.8%) than Group 2 (1.25%). It was reported that the maxillary lateral incisors are the teeth that tend to be affected the most from dilaceration.[35] It was also reported that the roots of lateral teeth, when dilacerated, tend to curve in a distal direction.[36] Similarly, in Group 1, the upper lateral incisors had the highest incidence of dilaceration (35%), followed by the maxillary first premolars, mandibular canines, and first premolars [Table 5]. However, there are numerous known and unknown factors which lead to deviations in normal root development.[37] Based on the results of this study, it may be considered that heavy orthopedic force applied in mixed dentition is one of these risk factors for disorders of root development. Another possible reason for the high prevalence of dilacerations in lateral teeth may be that these can be diagnosed more easily on panoramic films compared to other teeth due to a high tendency of these teeth to be distally dilacerated.
A number of limitations of this study need to be considered. The principal limitation of this study was the use of two-dimensional radiographs. Therefore, the shorter or longer root lengths may be observed due to the changes in the buccolingual inclination of the posterior teeth. These torque changes were not possible to assess in this study. The authors were also unable to analyze the labial-buccal and lingual-palatal root dilaceration or volumetric changes of dental roots. On the other hand, CBCT scan to evaluate root resorption was not an option due to ethical reasons. Additional three-dimensional imaging was not needed for the orthodontic diagnosis and treatment planning in these patients. However, the use of two-dimensional panoramic radiographs to measure root resorptions was another limitation of the study. Further studies that provide quantitative three-dimensional analysis need to be carried out to validate the long-term adverse effects of early orthopedic forces.
Considered together, these findings suggest a possible role for early orthopedic intervention in promoting root resorption during fixed orthodontic treatment. RME&RHg therapy is the most effective method used for treatment of skeletal Class III malocclusion in children, and it will, of course, continue to be used for early orthopedic treatment. However, it should be kept in mind that early orthopedic forces may have potential adverse effects on a dental root in the long-term. Patients who have a history of previous RME&RHg therapy should be examined carefully in terms of dental root health at the beginning of a fixed orthodontic treatment. Considering that these patients may have an increased risk of root resorption, orthodontic treatment planning and the mechanics of tooth movement might need to be modified (miniscrew-supported Class III treatment with the RME&RHg). In these cases, clinical examination and radiographic monitoring should be performed periodically to control root resorption.
CONCLUSION
The patients treated in two phases with RME&RHG followed by fixed appliances showed relatively more root resorption
Following fixed orthodontic treatment, significant root length differences were found between the groups. However, it could be considered clinically minor changes
The prevalence of root dilaceration in mesiodistal plane was higher in the patients treated in two phases with RME&RHG followed by fixed appliances.
Ethical approval
The experimental protocols of this study were approved by the Bezmialem Vakif University Local Ethics Committee (03.09.2019, 16/298).
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence of angle Class III malocclusion: A systematic review and meta-analysis. Open J Epidemiol. 2012;2:75-82.
- [CrossRef] [Google Scholar]
- Treatment effects of simple fixed appliance and reverse headgear in correction of anterior crossbites. Am J Orthod Dentofacial Orthop. 2000;117:691-9.
- [CrossRef] [Google Scholar]
- Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop. 2015;148:22-36.
- [CrossRef] [PubMed] [Google Scholar]
- Early orthopedic correction of skeletal Class III malocclusion using combined reverse twin block and face mask therapy. J Indian Soc Pedod Prev Dent. 2015;33:3-9.
- [CrossRef] [PubMed] [Google Scholar]
- Camouflage treatment of skeletal Class III malocclusion with conventional orthodontic therapy. Am J Orthod Dentofacial Orthop. 2017;151:804-11.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the face mask in the treatment of maxillary skeletal retrusion. Am J Orthod Dentofacial Orthop. 1988;93:3888-94.
- [Google Scholar]
- Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2011;82:488-94.
- [CrossRef] [PubMed] [Google Scholar]
- Dental root development associated with treatments by rapid maxillary expansion/ reverse headgear and slow maxillary expansion. Eur J Orthod. 2019;41:544-50.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal anteroposterior discrepancy and vertical type effects on lower incisor preoperative decompensation and postoperative compensation in skeletal Class III patients. Angle Orthod. 2011;81:64-74.
- [CrossRef] [PubMed] [Google Scholar]
- Cone-beam computed tomography versus periapical radiograph for diagnosing external root resorption: A systematic review and meta-analysis. Angle Orthod. 2017;87:328-37.
- [CrossRef] [PubMed] [Google Scholar]
- A radiographic study of posterior apical root resorption in orthodontic patients. Am J Orthod Dentofacial Orthop. 1994;105:345-9.
- [CrossRef] [Google Scholar]
- Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190:16-22.
- [CrossRef] [PubMed] [Google Scholar]
- Measurements of tooth length in panoramic radiographs, 1. The use of indicators. Dentomaxillofac Radiol. 1992;21:26-30.
- [CrossRef] [PubMed] [Google Scholar]
- Apical root resorption in orthodontically treated subjects: Analysis of edgewise and light wire mechanics. Am J Orthod Dentofacial Orthop. 1994;105:350-61.
- [CrossRef] [Google Scholar]
- Apical root resorption in upper anterior teeth. Eur J Orthod. 1983;5:173-83.
- [CrossRef] [PubMed] [Google Scholar]
- A radiographic comparison of apical root resorption after orthodontic treatment with the edgewise and speed appliances. Am J Orthod Dentofacial Orthop. 1995;108:76-84.
- [CrossRef] [Google Scholar]
- Dilaceration of permanent upper lateral incisors: Frequency, direction, and endodontic treatment implications. Oral Surg Oral Med Oral Pathol. 1983;55:519-20.
- [CrossRef] [Google Scholar]
- Statistical Methods for Medical and Biological Students New York: Interscience Publications; 1940.
- [Google Scholar]
- Association of orthodontic force system and root resorption: A systematic review. Am J Orthod Dentofacial Orthop. 2015;147:610-26.
- [CrossRef] [PubMed] [Google Scholar]
- An insight into risk factors for root resorption during orthodontic treatment. J Med Sci. 2017;17:1-9.
- [CrossRef] [Google Scholar]
- Root resorption 4 months after initiation of fixed orthodontic appliance therapy. Pak Oral Dent J. 2018;38:481-5.
- [Google Scholar]
- Orthodontic mechanotherapies and their influence on external root resorption: A systematic review. Am J Orthod Dentofacial Orthop. 2019;155:313-29.
- [CrossRef] [PubMed] [Google Scholar]
- Is early Class III protraction facemask treatment effective? A multicentre, randomized controlled trial: 3-year follow-up. J Orthod. 2012;39:176-85.
- [CrossRef] [PubMed] [Google Scholar]
- Association between root resorption and tooth development: A quantitative clinical study. Am J Orthod Dentofacial Orthop. 2020;157:602-10.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of linear and angular measurements on panoramic radiographs taken at various positions in vitro. Eur J Orthod. 2002;24:43-52.
- [CrossRef] [PubMed] [Google Scholar]
- Apical root resorption during orthodontic treatment: A prospective study using cone beam CT. Angle Orthod. 2011;82:480-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cone-beam computed tomography for routine orthodontic treatment planning: A radiation dose evaluation. Am J Orthod Dentofacial Orthop. 2008;133:640.e1-5.
- [CrossRef] [PubMed] [Google Scholar]
- External apical root resorption in Class II malocclusion: A retrospective review of 1-versus 2-phase treatment. Am J Orthod Dentofacial Orthop. 2003;124:151-6.
- [CrossRef] [Google Scholar]
- Meta analysis of the treatment related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71-8.
- [CrossRef] [PubMed] [Google Scholar]
- Apical root resorption due to orthodontic treatment detected by cone beam computed tomography. Angle Orthod. 2012;83:196-203.
- [CrossRef] [PubMed] [Google Scholar]
- Electromyographic evaluation in children having rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2009;136:355-60.
- [CrossRef] [PubMed] [Google Scholar]
- Malformations of the tooth root in humans. Front Physiol. 2015;6:307.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between pulp dimensions and development of pulp necrosis after luxation injuries in the permanent dentition. Endod Dent Traumatol. 1986;2:90-8.
- [CrossRef] [PubMed] [Google Scholar]
- Altered dental root development in long-term survivors of pediatric acute lymphoblastic leukemia. A review of 17 cases. Cancer. 1987;59:1640-8.
- [CrossRef] [Google Scholar]
- Assessment of root resorption and root shape: Periapical vs panoramic films. Angle Orthod. 2001;71:185-9.
- [Google Scholar]
- The molecular control of and clinical variations in root formation. Cells Tissues Organs. 2007;186:86-93.
- [CrossRef] [PubMed] [Google Scholar]






