Translate this page into:
Evaluation of the upper airway dimensions following Herbst appliance treatment in adolescents: A retrospective study

*Corresponding author: Yanqi Yang, Department of Paediatric Dentistry and Orthodontics, The University of Hong Kong, Prince Philip Dental Hospital, Sai Ying Pun, Hong Kong, China. yangyanq@hku.hk
-
Received: ,
Accepted: ,
How to cite this article: Gu M, Lin Y, McGrath CP, Hägg U, Wong RW, Yang Y. Evaluation of the upper airway dimensions following Herbst appliance treatment in adolescents: A retrospective study. APOS Trends Orthod 2020;10(3):153-63.
Abstract
Objectives:
This retrospective study investigated dimensional changes in the upper airway following Herbst appliance therapy in adolescents with Class II malocclusion and compared those changes with growth data.
Materials and Methods:
Lateral cephalograms from 44 Herbst-treated adolescents (23 boys, mean age = 13.3 ± 1.1 years, and 21 girls, mean age = 12.6 ± 1.1 years) were analyzed for the changes in the upper airway and craniofacial variables. Longitudinal cephalometric data of 34 untreated adolescents (15 boys, mean age = 12.6 ± 0.3 years, and 19 girls, mean age = 12.9 ± 0.4 years) were used as growth data for comparison.
Results:
Following treatment, significant changes were noted in most of the variables. Boys displayed greater downward movement of the hyoid bone than girls did (P = 0.021). Compared with the growth data, a greater increase in retroglossal oropharyngeal depth and hypopharyngeal depth was observed in boys and girls, respectively. Both displayed a decrease in the inclination of the soft palate and a smaller change in nasopharyngeal depth.
Conclusion:
Herbst appliance therapy enlarges the upper airway dimensions at two dissimilar sites in girls (oropharynx) and boys (hypopharynx). Boys display a greater increase in anterior and posterior facial heights than girls do, potentially accounting for the site dissimilarities. Moreover, a Herbst appliance improves the inclination of the soft palate and restricts the growth of the nasopharynx in both boys and girls.
Keywords
Herbst appliance
Upper airway
Growth
INTRODUCTION
The history of using functional appliances (FAs) to correct skeletal Class II malocclusion spans more than 100 years.[1] Evidence has shown that FAs can stimulate the growth of the mandible in growing children, at least in the short term.[2,3] Class II malocclusion has been identified as a risk factor for pediatric sleep-disordered breathing (SDB);[4,5] therefore, whether FAs therapy increases the dimensions of the upper airway merits research.
A number of studies have reported enlarged pharyngeal dimensions following various FAs therapies.[6-11] In a systematic review and meta-analysis, Xiang et al.[12] demonstrated FAs specifically enlarged the oropharyngeal space. The long-term stability following FAs therapies was reported by Yassaei et al.[13] and Hanggi et al.[14] from 4 to 22 years. However, several studies have still reported no change in the upper airway dimension following FAs therapy.[15,16] Ulusoy et al.[17] even reported that the upper airway dimension did not increase during the period of FAs therapy but increase later during the retention period. The combined subjects of boys and girls may result in the different results of the previous studies. Because the growth of the upper airway structures likely differs for adolescent boys and girls,[18] sex should be considered when analyzing the effects of FAs. Therefore, the present study aimed to separately assess the effects of Herbst appliance treatment in boys and girls.
MATERIALS AND METHODS
Study participants
Lateral cephalograms of consecutive patients who were treated with Herbst appliance at the Department of Paediatric Dentistry and Orthodontics of the University of Hong Kong between 2000 and 2012 were screened, and all 44 subjects (23 boys, mean age = 13.3 ± 1.1 years, and 21 girls mean age = 12.6 ± 1.1 years) who fulfilled the following criteria were selected as study participants [Table 1]
| n | Age at baseline (year) | Age at after treatment (year) | Duration of treatment (month) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | ||
| Herbst group | 44 | ||||||||||||
| Male | 23 | 13.3 | 1.1 | 12.0 | 16.0 | 14.4 | 1.1 | 13.0 | 17.0 | 11.7 | 1.3 | 10.0 | 14.0 |
| Female | 21 | 12.6 | 1.1 | 10.0 | 14.0 | 13.6 | 1.2 | 11.0 | 16.0 | 11.6 | 1.3 | 10.0 | 14.0 |
| Control group | 34 | ||||||||||||
| Male | 15 | 12.6 | 0.3 | 12.2 | 13.3 | ||||||||
| Female | 19 | 12.9 | 0.4 | 12.0 | 13.7 | ||||||||
Chinese patients
Age at the baseline: 10–14 years for girls and 12–16 years for boys (ranges represent the average age of the pubertal growth peak ± 2 years)[19]
Duration of the therapy: 10–14 months
A conventional Herbst appliance without a headgear used during the therapy
Quality cephalograms recorded at the beginning and end of Herbst appliance therapy in the natural head posture, displaying recognizable upper airway structures, and not during deglutition
No craniofacial syndromes or clefts.
Longitudinal cephalometric data were obtained from 34 Chinese adolescents (15 boys and 19 girls). At the age of approximately 12 years, they participated in an oral health survey [Table 1], during which they were reviewed during various periods (3–6 months, 5 years, and 15 years) to observe the reproducibility of the natural head posture.[20,21] None of these adolescents underwent any orthodontic treatment during the review period, and none of them exhibited craniofacial syndromes or clefts. The ANB angle and Wits appraisal displayed skeletal Class I pattern in 23 adolescents, and skeletal Class II pattern in 11 adolescents.
The present study was a retrospective study. All the cephalometric data were anonymized and de-identified before analysis, and an ethics approval has been granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (IRB Reference Number: UW 12-405).
Cephalometric analysis
All cephalograms were scanned (Epson Expression 1649XL, Seiko Epson Corp., Japan) and the analyzed using CASSOS software (Soft Enable Technology Limited, Hong Kong, China). The upper airway variables included eight linear variables and one angular variable: Three variables for the soft palate, four for upper airway depth, and two for the position of the hyoid bone.[18] Craniofacial variables consisted of three angular and two linear variables [Table 2 and Figure 1]. All linear variables were corrected according to the actual magnification.
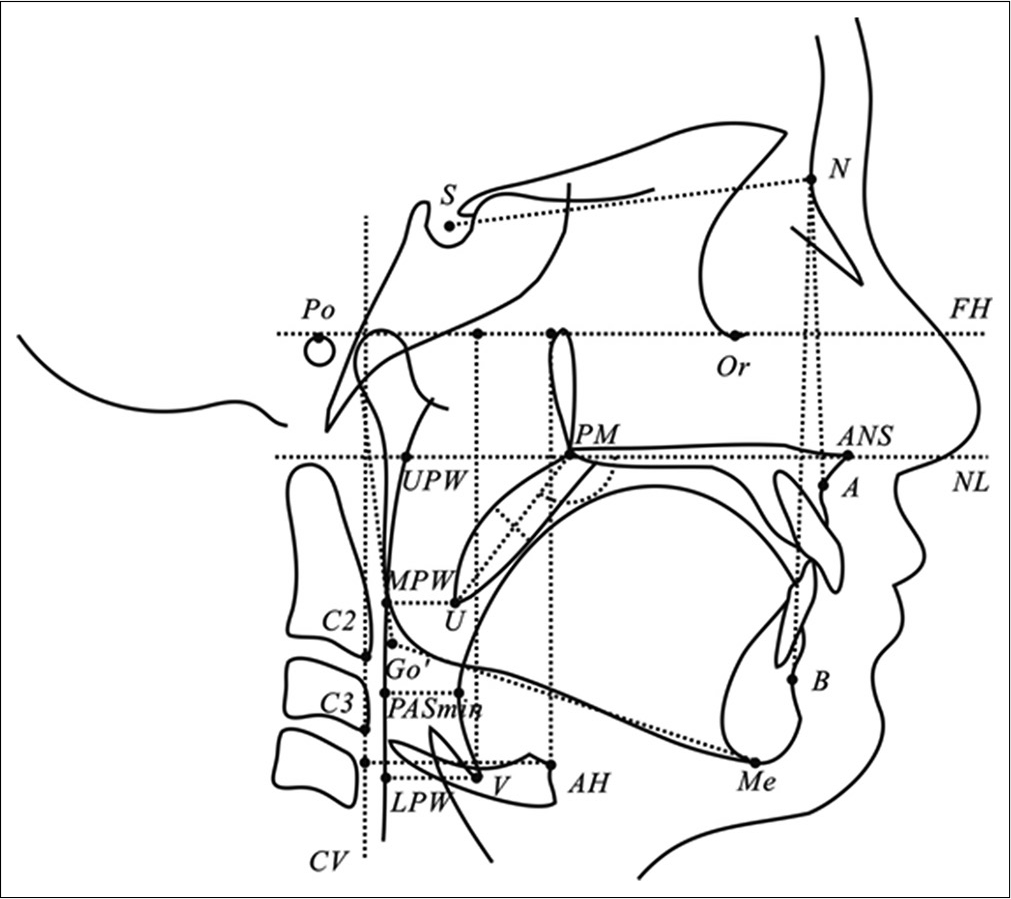
- Landmarks and measurements of the upper airway.
| Variables | Definition |
|---|---|
| Landmarks | |
| Po | Porion, the midpoint of the line connecting the most superior point of the external auditory canal on both sides |
| Or | Orbitale, the lowest point on the average of the left and right inferior borders of the bony orbit |
| ANS | Anterior nasal spine, the tip of the median, sharp bony process of the maxilla |
| PM | Pterygomaxillare, the point at the junction of the pterygomaxilla and the posterior nasal spine |
| U | Uvula, the tip of the uvula |
| UPW | Upper pharyngeal wall, point of intersection of the line NL to the posterior pharyngeal wall |
| MPW | Middle pharyngeal wall, intersection of the perpendicular line from U to the posterior pharyngeal wall |
| LPW | Lower pharyngeal wall, intersection of the perpendicular line from V to the posterior pharyngeal wall |
| V | Vallecula, the intersection of the epiglottis and the base of the tongue |
| AH | Anterior hyoid, the most anterior and superior point on the body of the hyoid bone |
| C2 | Second cervical vertebrae, the point at the most anterior-inferior position on the second cervical vertebrae |
| C3 | Third cervical vertebrae, the point at the most anterior-inferior position on the third cervical vertebrae |
| FH | Frankort horizontal plane, line joining the Or to the Po |
| NL | Nasal line, line joining the ANS and Pm |
| CV | Cervical vertebrae, the line joining the C2 and C3 |
| S | Center of the sella turcica |
| N | Nasion, the deepest point in the concavity of nasofrontal suture |
| A | A point, the deepest point in the concavity of the anterior maxilla between the anterior nasal spine and the alveolar crest |
| B | B point, the deepest point in the concavity of the anterior mandible between the alveolar crest and the Pogonion |
| Me | Mention, the most inferior point on the body chin |
| Go’ | Gonion’ point, the intersection of the tangents of inferior and posterior borders of the mandible |
| Measurements | |
| PM-U (mm) | Length of soft palate, distance from PM to U |
| SPT (mm) | Soft palate thickness, represents the maximal thickness of the soft palate measured perpendicular to PM-U line |
| NL/PM-U (°) | Inclination of the long axis of the soft palate relative to the nasal line |
| PM-UPW (mm) | Depth of the nasopharyngeal airway space from PM to UPW |
| U-MPW (mm) | Depth of the oropharyngeal airway space from U to MPW |
| PASmin (mm) | Shortest distance between the base of the tongue and the posterior pharyngeal wall, the narrowest sagittal airway space |
| V-LPW (mm) | Depth of the hypopharyngeal airway space from V to LPW |
| AH-FH (mm) | Position of the hyoid bone in vertical plane, from AH perpendicular to FH |
| AH-CV (mm) | Position of the hyoid bone in horizontal plane, from AH to CV and parallel to FH |
| SNA (°) | Angle between the S-N line and the N-A line |
| SNB (°) | Angle between the S-N line and the N-B line |
| ANB (°) | Angle between the N-A line and the N-B line |
| TAFH (mm) | Distance from N to Me |
| TPFH (mm) | Distance from S to Go’ |
Data analysis
An examiner (MG) measured all variables. Cephalograms from 15 randomly selected participants (two radiographs per participant) were measured on separate occasions at a 2-week interval. The method error was calculated by Dahlberg’s formula,[22], where ∑d is the difference between the pairs of replicate measurements, and n is the number of replicate measurements. The method errors for the linear and angular measurements were not significant using a paired t-test and did not exceed 1 mm and 1°, respectively.
All variables were presented as the mean ± standard deviation. A paired t-test was used to compare the changes between pre- and post-Herbst appliance therapy. A two- sample t-test was used to compare the changes between boys and girls. The Pearson correlation analysis was conducted to analyze the relationship between changes in the upper airway and craniofacial variables. The levels of statistical significance were set at P < 0.05, P < 0.01, and P < 0.001. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (IBM SPSS Statistics, Version 20, IBM Corp.).
Because the growth data used in the present study comprised longitudinal data of 38 adolescents measured at various review intervals and dissimilar review durations, the quantitative calculation was difficult. Hence, the visual inspection method was used to compare the changes in the upper airway variables with growth curves generated by the locally weighted scatterplot smoothing (LOESS) method. The LOESS method is a flexible nonparametric regression technique that does not require a priori specification of a function to fit a particular model to data.[23] In SPSS, “% of points to fit” was set at 85% for the LOESS option and “Triweight” for the kernel option, similar to a previous study.[24] A line representing the mean change in pre- and post-Herbst appliance therapy was drawn on the same scatterplot. The slope of this line was compared with that of the growth curve. A steeper slope indicated a greater change in an upper airway variable following Herbst appliance therapy compared with that in the same variable because of natural growth, whereas a flatter slope indicated a smaller change.
RESULTS
Following Herbst appliance therapy, significant changes were observed in most of the variables in both boys and girls [Table 3]. The largest increase in upper airway depth was observed in boys at the hypopharynx (V-LPW, 2.1 mm, P = 0.002), followed by the retroglossal oropharynx (PASmin, 1.8 mm, P = 0.009), the largest increase in the upper airway depth was observed in girls at the retroglossal oropharynx (PASmin, 1.8 mm, P = 0.007). Both boys and girls displayed no significant change in nasopharyngeal depth (PM-UPW), with increased absolute values (1 mm in boys and 0.2 mm in girls). The inclination of the soft palate (NL/PM-U) was improved in both boys and girls (‒3°, P = 0.002, in boys; ‒2.7°, P = 0.011, in girls).
| Variables | Definition | Males | P-value | Females | P-value | Gender difference M vs. F | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | d | Pre-treatment | Post-treatment | D | ||||||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||||||||
| Soft palate | |||||||||||
| PM-U (mm) | Length of the soft palate | 32.2±4.5 | 32.8±4.7 | 0.5 | 0.185 | 31.0±4.1 | 31.2±3.4 | 0.2 | 0.609 | 0.3 | 0.609 |
| SPT (mm) | Soft palate thickness | 8.8±1.3 | 9.4±1.3 | 0.6 | 0.021* | 8.3±1.3 | 8.5±1.1 | 0.2 | 0.278 | 0.4 | 0.227 |
| NL/PM-U (°) | Inclination of the long axis of the soft palate relative to the nasal line | 130.4±7.5 | 127.4±6.6 | ‒3.0 | 0.002** | 130.9±6.6 | 128.2±5.4 | ‒2.7 | 0.011* | ‒0.3 | 0.797 |
| Depth of upper airway | |||||||||||
| PM-UPW (mm) | Depth of the nasopharyngeal airway space | 23.4±4.3 | 24.4±3.4 | 1.0 | 0.146 | 21.3±3.8 | 21.5±3.8 | 0.2 | 0.808 | 0.8 | 0.365 |
| U-MPW (mm) | Depth of the retropalatal pharyngeal airway space | 10.3±2.9 | 11.1±2.9 | 0.8 | 0.039* | 9.6±2.0 | 10.9±2.0 | 1.3 | 0.001** | ‒0.5 | 0.352 |
| V-LPW (mm) | Depth of the hypopharyngeal airway space | 16.7±2.7 | 18.8±2,9 | 2.1 | 0.002** | 14.9±2.2 | 15.7±2.2 | 0.8 | 0.128 | 1.3 | 0.113 |
| PASmin (mm) | Depth of the retroglossal pharyngeal airway space | 10.5±2.7 | 12.3±2.8 | 1.8 | 0.009** | 9.1±2.7 | 10.9±2.9 | 1.8 | 0.007** | 0.0 | 0.965 |
| Position of the hyoid bone | |||||||||||
| AH-FH (mm) | Position of the hyoid bone in the vertical plane | 81.5±6.0 | 84.1±7.6 | 2.5 | 0.006** | 77.6±4.2 | 77.4±4.8 | ‒0.2 | 0.788 | 2.7 | 0.021* |
| AH-CV (mm) | Position of the hyoid bone in the horizontal plane | 33.9±3.2 | 35.8±3.8 | 1.9 | 0.007** | 29.9±2.9 | 30.9±2.7 | 0.9 | 0.015* | 1.0 | 0.208 |
| Craniofacial skeleton | |||||||||||
| SNA (°) | e angle between the S-N line and the N-A line | 83.0±4.2 | 81.9±4.4 | ‒1.1 | 0.013* | 81.6±2.6 | 81.0±3.1 | ‒0.5 | 0.080 | ‒0.6 | 0.275 |
| SNB (°) | e angle between the S-N line and the N-B line | 76.6±3.9 | 77.5±4.2 | 0.9 | 0.005** | 75.2±3.1 | 76.7±3.8 | 1.5 | 0.001** | ‒0.6 | 0.240 |
| ANB (°) | e angle between the N-A line and the N-B line | 6.4±2.0 | 4.4±2.0 | ‒2.0 | <0.001*** | 6.3±1.8 | 4.3±2.0 | ‒2.0 | <0.001*** | 0.0 | 0.964 |
| TAFH (mm) | Total anterior facial height, the distance from N to Me | 116.3±6.5 | 122.3±6.4 | 6.0 | <0.001*** | 112.5±4.3 | 117.5±4.3 | 5.0 | <0.001*** | 1.0 | 0.145 |
| TPFH (mm) | Total posterior facial height, the distance from S to Go’ | 77.6±6.4 | 82.1±6.8 | 4.5 | <0.001*** | 73.6±4.8 | 77.4±5.4 | 3.8 | <0.001*** | 0.7 | 0.271 |
Only the changes in the vertical position of the hyoid bone were significantly different between boys and girls. Boys demonstrated the significantly greater downward movement of the hyoid bone than girls did (AH-FH, 2.7 mm, P = 0.021) [Table 3].
The associations between the changes in the upper airway and craniofacial variables were typically weak [Table 4]. The change in retropalatal oropharyngeal depth (U-MPW) was positively associated with the change in the SNB angle (r = 0.39, P = 0.009), and the change in hypopharyngeal depth (V-LPW) was positively associated with the changes in both anterior (r = 0.36, P = 0.017) and posterior (r = 0.53, P < 0.001) facial heights [Table 4].
| SNA (°) | SNB (°) | ANB (°) | TAFH (mm) | TPFH (mm) | ||
|---|---|---|---|---|---|---|
| PM-U (mm) | Coefficient | –0.26 | –0.43** | 0.16 | 0.17 | –0.09 |
| P-value | 0.084 | 0.004 | 0.301 | 0.284 | 0.543 | |
| SPT (mm) | Coefficient | –0.09 | 0.03 | –0.12 | 0.09 | 0.24 |
| P-value | 0.579 | 0.859 | 0.429 | 0.551 | 0.124 | |
| NL/PM-U (°) | Coefficient | –0.20 | –0.29 | 0.09 | –0.15 | –0.30* |
| P-value | 0.192 | 0.056 | 0.576 | 0.345 | 0.045 | |
| PM-UPW (mm) | Coefficient | –0.05 | –0.13 | 0.08 | –0.16 | –0.11 |
| P-value | 0.738 | 0.390 | 0.593 | 0.295 | 0.489 | |
| U-MPW (mm) | Coefficient | 0.17 | 0.39** | –0.22 | –0.01 | 0.30* |
| P-value | 0.258 | 0.009 | 0.155 | 0.950 | 0.046 | |
| V-LPW (mm) | Coefficient | –0.06 | 0.10 | –0.18 | 0.36* | 0.53** |
| P-value | 0.685 | 0.500 | 0.249 | 0.017 | 0.000 | |
| PASmin (mm) | Coefficient | –0.05 | 0.29 | –0.36* | 0.17 | 0.37* |
| P-value | 0.728 | 0.060 | 0.017 | 0.282 | 0.014 | |
| AH-FH (mm) | Coefficient | –0.21 | –0.19 | –0.03 | 0.25 | 0.23 |
| P-value | 0.175 | 0.230 | 0.836 | 0.099 | 0.131 | |
| AH-CV (mm) | Coefficient | 0.06 | 0.10 | –0.04 | 0.11 | 0.50** |
| P-value | 0.694 | 0.518 | 0.803 | 0.481 | 0.000 |
A comparison between the slopes of lines representing changing in the upper airway variables following Herbst appliance therapy and those of growth curves illustrated that the changes in nasopharyngeal depth (PM-UPW) in both boys and girls following Herbst appliance therapy were smaller than those in the corresponding variables after natural growth [Figures 2 and 3], particularly in girls. The changes of in retroglossal oropharyngeal depth (PASmin) in girls [Figure 4], hypopharyngeal depth (V-LPW) in boys, and the inclination of the soft palate (NL/PM-U) following Herbst appliance therapy were slightly greater than those in the corresponding variables after natural growth [Figures 5-7]. The changes in other variables did not evidently differ from those in the corresponding variables after natural growth.
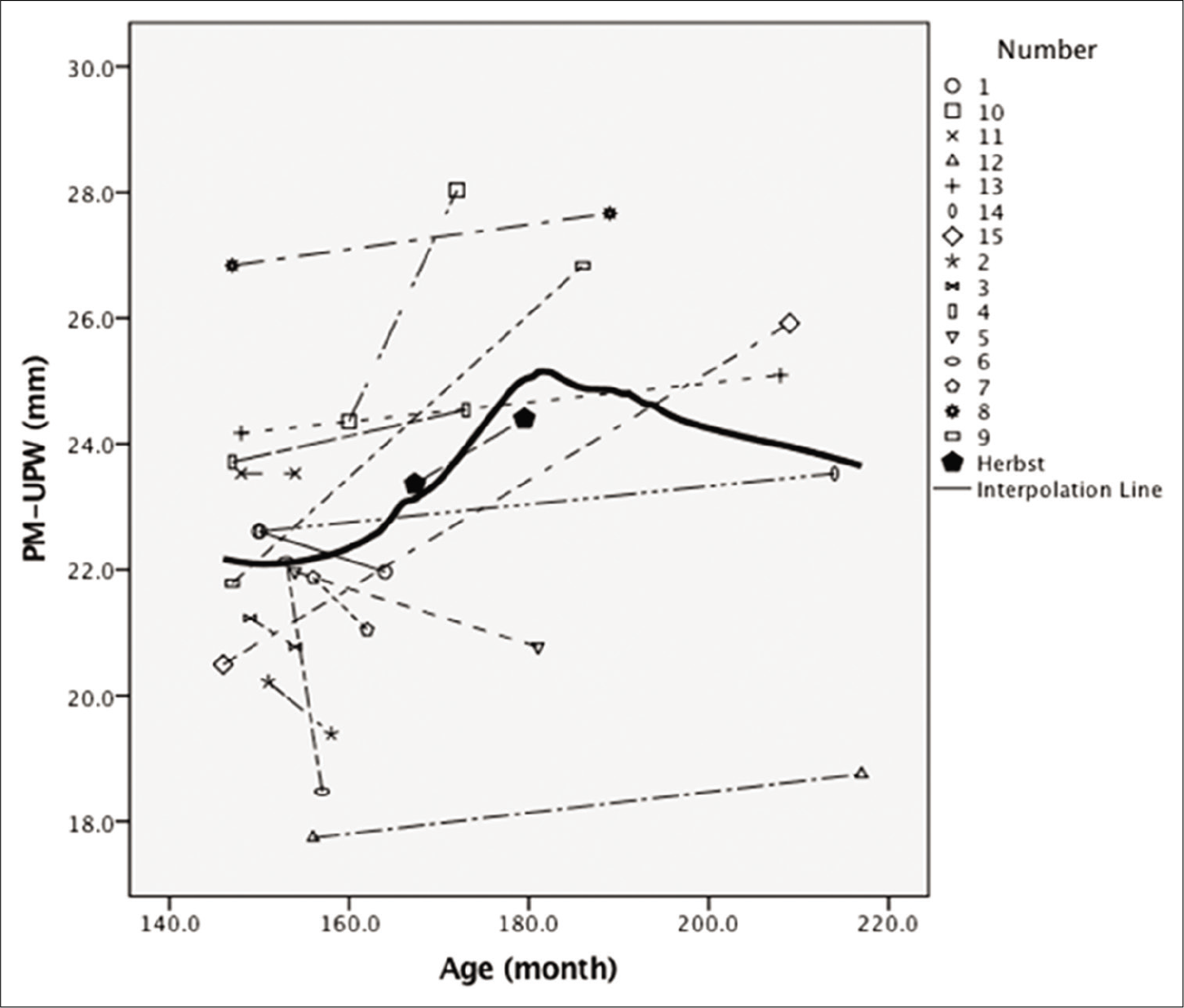
- The graphical comparison for variable of PM-UPW in males.

- The graphical comparison for variable of PM-UPW in females.

- The graphical comparison for variable of PASmin in females.
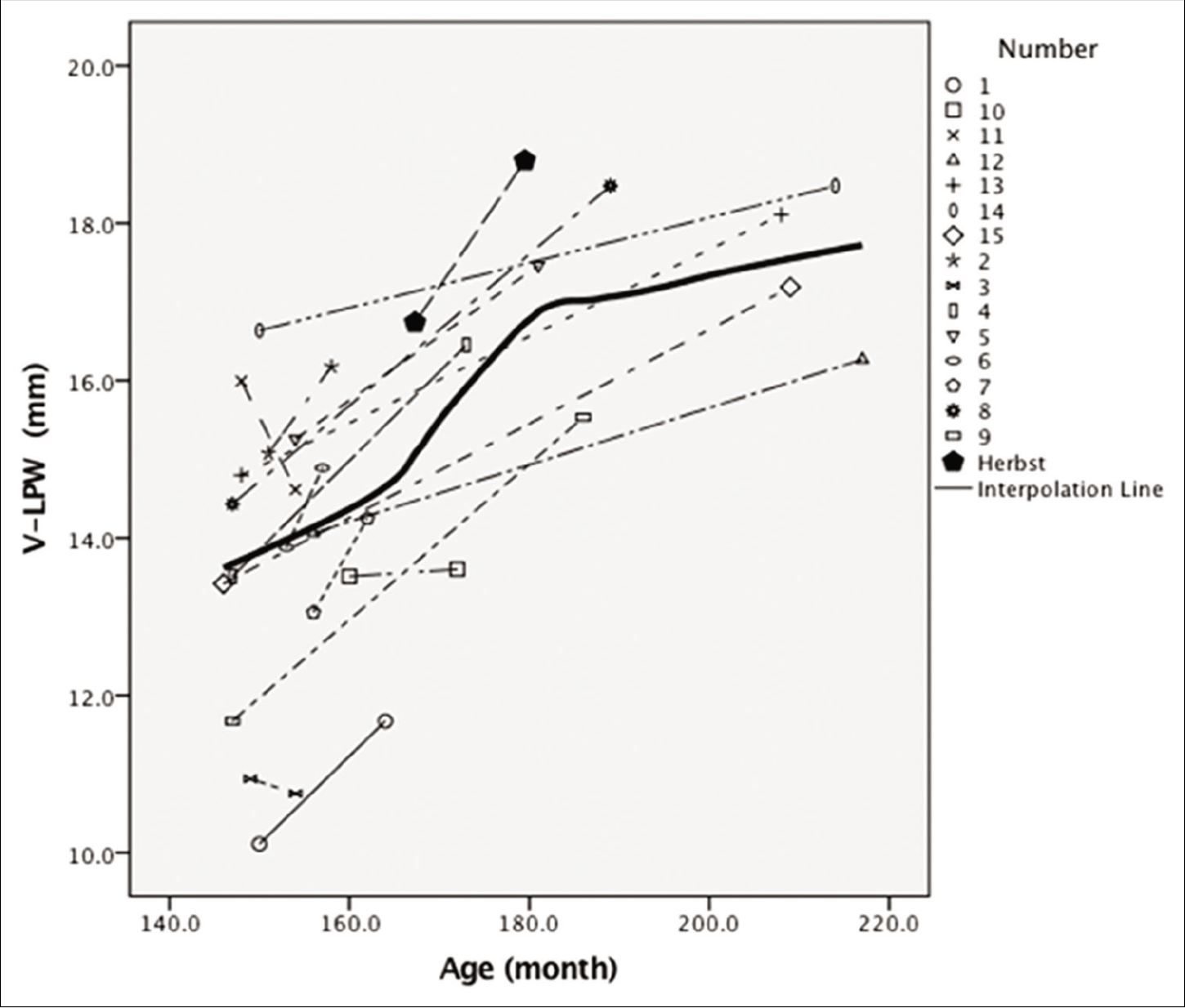
- The graphical comparison for variable of V-LPW in males.
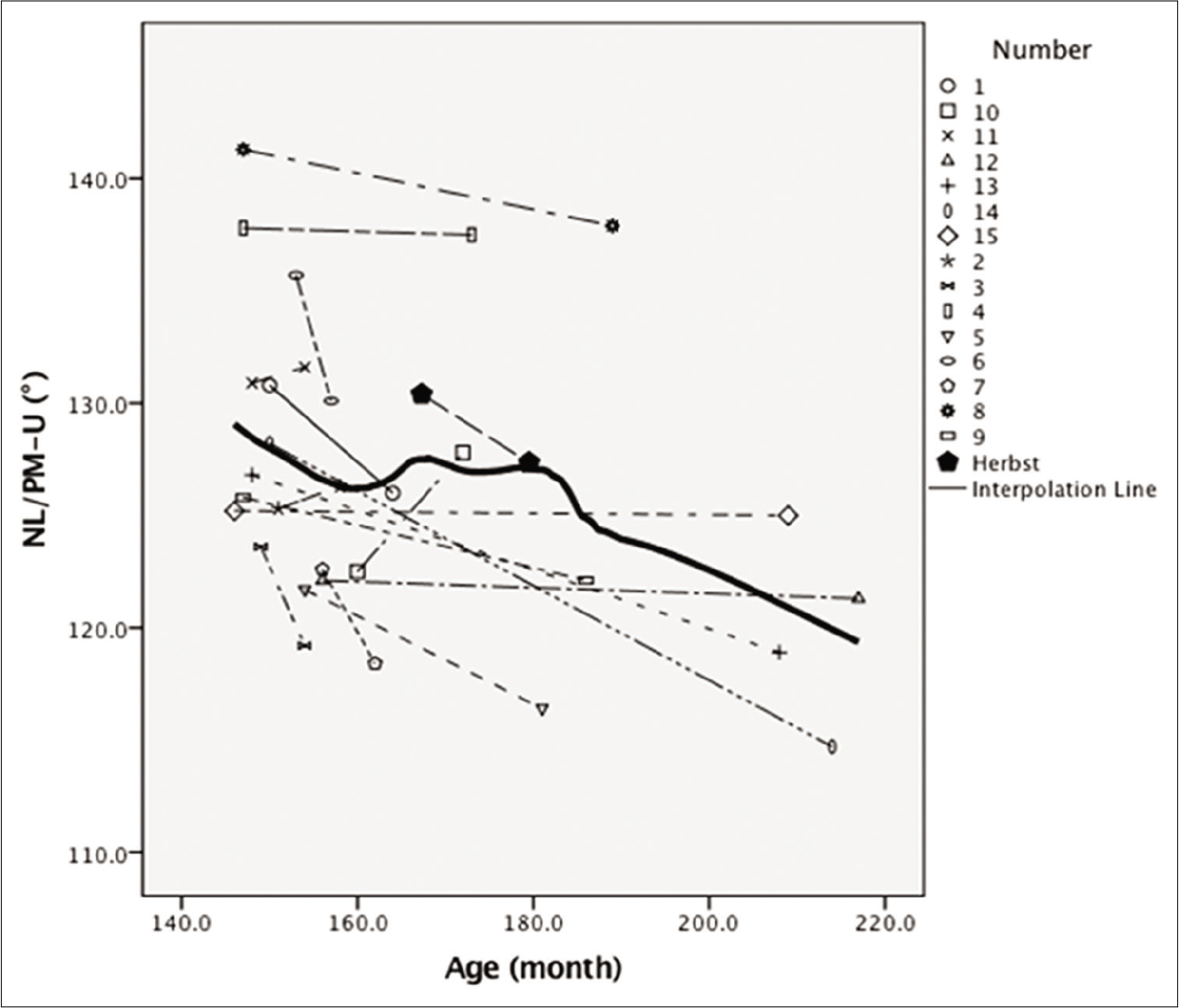
- The graphical comparison for variable of NL/PM-U in males.
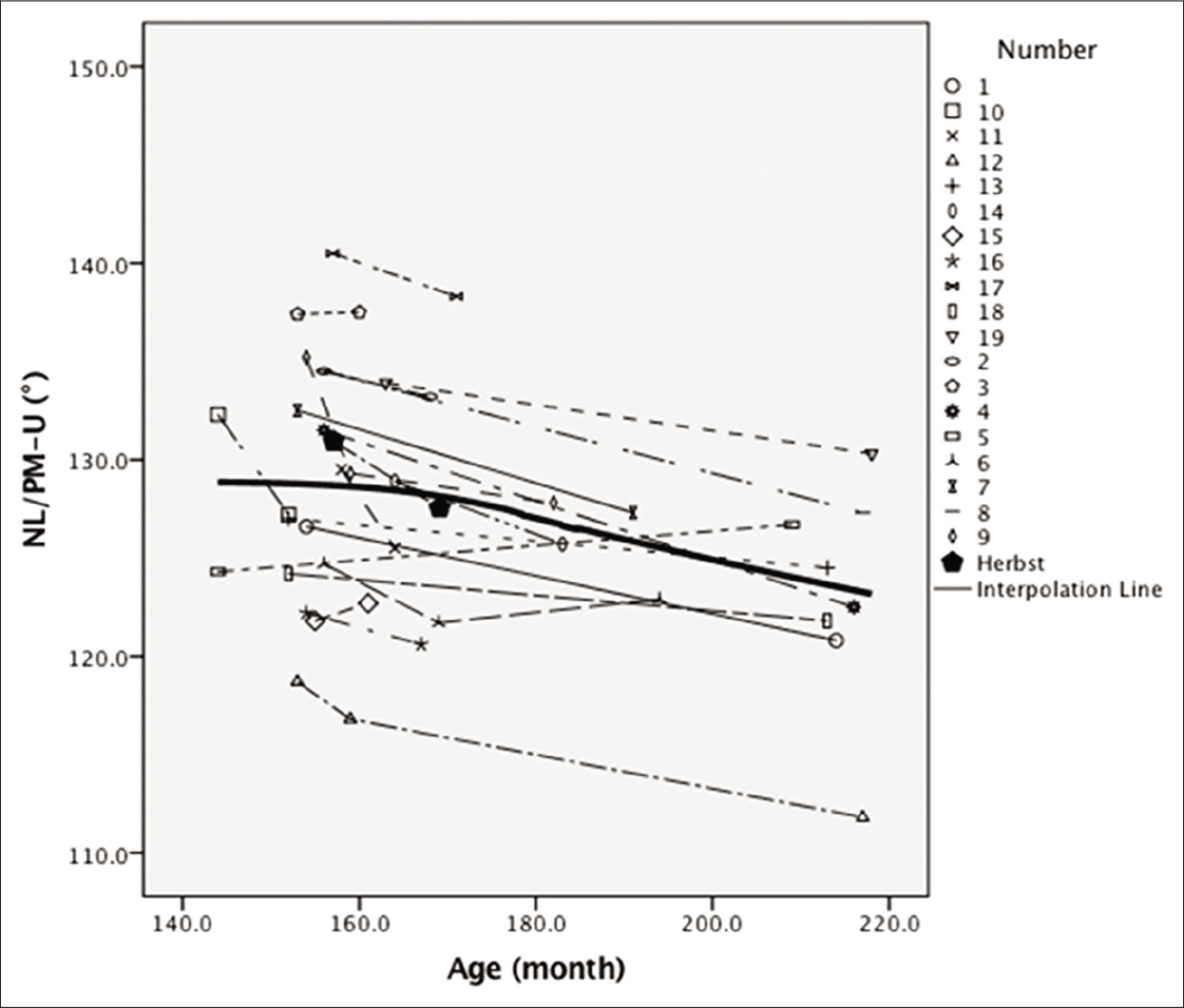
- The graphical comparison for variable of NL/PM-U in females.
DISCUSSION
The present study investigated dimensional changes in the upper airway structures, including the pharynx, soft palate, and hyoid bone, which were potentially influenced by FA therapy.[6,8,25] The tongue was not measured because the tongue contour was not clear without a coat of barium sulfate paste in previous cephalograms.[26] The pharynx was assessed at four regions: The nasopharynx, located superior to the level of the soft palate; the oropharynx, located between the level of the soft palate and the larynx, and further subdivided into two regions as retropalatal and retroglossal regions; and the hypopharynx, located from the base of the epiglottis to the larynx.[27]
Effect of Herbst appliance therapy on the nasopharynx
The effect of FA therapy in the nasopharyngeal airway above the palatal plane is difficult to determine because the size of this region is greatly influenced by adenoid involution during the pre- and early adolescence period,[28] therefore, the present study used pharyngeal level crossing the palatal plane to represent the nasopharynx and found that the average change in nasopharyngeal depth following Herbst appliance therapy in both boys and girls was smaller than that in nasopharyngeal depth after natural growth. This effect was observed potentially because of the headgear effect of the Herbst appliance.[29] The headgear effect refers to the influence of inhibition of the maxillary growth as well as the distalization and intrusion of the upper molars produced by the Herbst appliance with the posterior-upward force on the maxillary complex, which is similar with the effect of a high- pull headgear.[29]
Several studies have reported that headgear treatment can reduce pharyngeal depth in adolescents.[7,30] Another study demonstrated that headgear treatment is likely to be associate with an increase in oropharyngeal depth.[31] However, no studies have reported the headgear effect of a FA on the upper airway. The present study suggested that FA therapy potentially restricts the growth of the nasopharynx.
Effect of Herbst appliance therapy on the oropharynx and soft palate
In the present study, the oropharynx was divided into two regions: Upper (retropalatal) and lower (retroglossal) regions. Because the soft palate is the anterior wall of the retropalatal oropharynx, its size and angulation are likely to be associated with the narrowing of this region,[32] and the FA treatment may change its dimensions.
Jena et al.[8] reported that the length and inclination of the soft palate decreased following Twin block appliance therapy, whereas the thickness of the soft palate and retropalatal oropharynx increased accordingly. The present study demonstrated a mild improvement in the inclination of the soft palate in both boys and girls, whereas changes in retropalatal oropharyngeal depth and the size of the soft palate following Herbst appliance therapy were the same as those observed after natural growth.
The possible explanation of these different results is that the headgear effect is likely to influence the upper region of the oropharynx, but only for a fixed FA, such as a Herbst appliance, because the delivered force is more consistent than removable FAs, such as a Twin Block appliance, or an Activator. Further research is required to compare these two types of appliances.
When the tongue moves forward in response to FA therapy, the depth of the lower region of the oropharynx is likely to increase.[33] The present study demonstrated that the retroglossal pharynx increased following the Herbst appliance therapy, but only in girls.
A similar result was reported by Iwasaki et al.[34] Using cone- beam computed tomography, the researchers observed that following Herbst appliance therapy, the depth of the retroglossal airway increased more in Herbst appliance treated group than the changes in the Class I control group, whereas there was no difference in the retropalatal airway depth between two groups. Because their study comprised a combination of boys and girls as participants, no sex-related differences were reported.
Effect of Herbst appliance on the hypopharynx
Iwasaki et al.[34] reported that a Herbst appliance can improve hypopharyngeal depth, but again no sex-related differences were reported. The present study demonstrated that only boys displayed a greater increase in hypopharyngeal depth compared with the increased that occurred from natural growth.
Therefore, the present study illustrated that Herbst appliance therapy can improve the upper airway dimension distinctly in boys and girls; for girls, the site was the retroglossal oropharynx; and for boys, the site was the hypopharynx.
Boys displayed improvement in a lower position than girls did probably because of the different increase in the facial height. In the present study, boys demonstrated a greater increase in the anterior and posterior facial heights than girls did although did not reach the level of significance. Furthermore, the Pearson correlation analysis revealed a positive association between the change in hypopharyngeal depth and the increase in the anterior and posterior facial heights.
Because the participants were Chinese, these results may not be consistent among other races. Mislik et al.[35] reported that no sex-related differences in oropharyngeal depth were observed in Caucasian children aged >9 years, whereas Gu et al.[18] reported sex-related differences were observed in 12-year-old Chinese children. Furthermore, Hanggi et al.[14] reported that the changes in the oropharyngeal depth following activator- headgear and fixed appliance therapy of Caucasian boys and girls were similar. Therefore, the growth potential is not similar in Chinese and Caucasian children, yielding potentially dissimilar results after FA therapy in these two races.
Effect of Herbst appliance therapy on the position of the hyoid bone
Although the present study revealed that the hyoid bone moved forward and downward significantly (except the vertical movement in girls) following Herbst appliance, none of these changes were caused by the treatment instead by natural growth. Ulusoy et al.[17] observed that the change in the hyoid bone position following activator appliance therapy occurred not in the treatment period but in the retention period, whether the participants of the present study displaying the same result needs further investigation that including the retention period.
Implication and limitations
Although the present study demonstrated that the Herbst appliance potentially restricted growth in the nasopharynx, the absolute value of the nasopharyngeal depth increased, with the improved inclination of the soft palate. Therefore, the influence of the headgear effect on the upper airway cannot be overemphasized. The main effects of Herbst appliance therapy were the enlargement of retroglossal oropharyngeal depth in girls and hypopharyngeal depth in boys. Hence, Herbst appliance therapy may be beneficial to children with potential SDB and Class II malocclusion. Schutz et al.[6] reported the Herbst appliance could improve nocturnal breathing in growing children.
Because of ethical limitations, we could not obtain pure longitudinal cephalometric data of Class II untreated Chinese adolescents. The participants from our growth data comprised adolescents with both skeletal Classes I and II patterns. Their summarized growth pattern is likely to overestimate from that of adolescents with pure Class II pattern,[36] therefore, the effects of Herbst appliance treatment might be underestimated in the present study. Furthermore, the visual inspection method was merely qualitative and not quantitative. Therefore, the results of the present study must be interpreted with caution and further confirmed with a multicenter trial with a larger sample size and proper control subjects.
CONCLUSION
Herbst appliance therapy enlarges the upper airway dimensions at two dissimilar sites in girls (oropharynx) and boys (hypopharynx). Boys display a greater increase in anterior and posterior facial heights than girls do, potentially accounting for the site dissimilarities. Moreover, a Herbst appliance improves the inclination of the soft palate and restricts growth of the nasopharynx in both boys and girls.
Acknowledgments
The authors thank Miss Kar Yan Li and Mr. Shadow Yeung for their kind assistance with the statistical analyses. The authors also thank Dr. M. S. Cooke, who obtained the longitudinal data.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
The authors declare that this study was funded by the Seed Funding Programme for Basic Research in the University of Hong Kong (201410159010) and that they have no financial and non-financial competing interests.
Conflicts of interest
There are no conflicts of interest.
References
- Removable Orthodontic Appliances (2nd ed). Philadlphia, PA: W. B. Saunders Company; 1984.
- [Google Scholar]
- Effectiveness of orthodontic treatment with functional appliances on mandibular growth in the short term. Am J Orthod Dentofacial Orthop. 2011;139:24-36.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599.e1-12. discussion e1-6
- [CrossRef] [PubMed] [Google Scholar]
- Craniofacial and upper airway morphology in pediatric sleep-disordered breathing: Systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2013;143:20-30.e3.
- [CrossRef] [PubMed] [Google Scholar]
- Craniofacial morphological characteristics in children with obstructive sleep apnea syndrome: A systematic review and meta-analysis. J Am Dent Assoc. 2013;144:269-77.
- [CrossRef] [PubMed] [Google Scholar]
- Class II correction improves nocturnal breathing in adolescents. Angle Orthod. 2011;81:222-8.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in upper airway width associated with Class II treatments (headgear vs activator) and different growth patterns. Angle Orthod. 2011;81:440-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of twin-block and mandibular protraction appliance-IV in the improvement of pharyngeal airway passage dimensions in Class II malocclusion subjects with a retrognathic mandible. Angle Orthod. 2013;83:728-34.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of fixed functional therapy on tongue and hyoid positions and posterior airway. Angle Orthod. 2014;84:260-4.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of two-phase treatment with the herbst and preadjusted edgewise appliances on the upper airway dimensions. Sci World J. 2016;2016:4697467.
- [CrossRef] [PubMed] [Google Scholar]
- Upper airway changes following functional treatment with the headgear herbst or headgear twin block appliance assessed on lateral cephalograms and magnetic resonance imaging. Sci World J. 2019;2019:1807257.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in airway dimensions following functional appliances in growing patients with skeletal Class II malocclusion: A systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol. 2017;97:170-80.
- [CrossRef] [PubMed] [Google Scholar]
- Stability of pharyngeal airway dimensions: Tongue and hyoid changes after treatment with a functional appliance. Int J Orthod Milwaukee. 2012;23:9-15.
- [Google Scholar]
- Long-term changes in pharyngeal airway dimensions following activator-headgear and fixed appliance treatment. Eur J Orthod. 2008;30:598-605.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of fixed appliances in correcting angle Class II on the depth of the posterior airway space: FMA vs. Herbst appliance-a retrospective cephalometric study. J Orofac Orthop. 2011;72:301-20.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in the pharyngeal airway and position of the hyoid bone after treatment with a modified bionator in growint patients with retrognathia. J Exp Clin Med. 2011;3:93-8.
- [CrossRef] [Google Scholar]
- Evaluation of airway dimensions and changes in hyoid bone position following Class II functional therapy with activator. Acta Odontol Scand. 2014;72:917-25.
- [CrossRef] [PubMed] [Google Scholar]
- Cephalometric norms for the upper airway of 12-year-old Chinese children. Head Face Med. 2014;10:38.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt. Acta Odontol Scand. 1980;38:187-200.
- [CrossRef] [Google Scholar]
- Fifteen-year reproducibility of natural head posture: A longitudinal study. Am J Orthod Dentofacial Orthop. 1999;116:82-5.
- [CrossRef] [Google Scholar]
- Five-year reproducibility of natural head posture: A longitudinal study. Am J Orthod Dentofacial Orthop. 1990;97:489-94.
- [CrossRef] [Google Scholar]
- Statistical Methods for Medical and Biological Students London, United Kingdom: Allen and Unwin; 1940.
- [Google Scholar]
- Loess: A nonparametric, graphical tool for depicting relationships between variables. Elect Stud. 2000;19:577-613.
- [CrossRef] [Google Scholar]
- To Tip or Not to Tip, is that a Question? Netherlands: Erasmus School of Economics; 2013. p. :38.
- [Google Scholar]
- Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327-36.
- [Google Scholar]
- A cephalometric comparison of subjects with snoring and obstructive sleep apnoea. Eur J Orthod. 2000;22:353-65.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiology of upper airway obstruction: A developmental perspective. Sleep. 2004;27:997-1019.
- [CrossRef] [PubMed] [Google Scholar]
- Growth of the nasopharynx and adenoid development from one to eighteeen years. Angle Orthod. 1976;46:243-59.
- [Google Scholar]
- The headgear effect of the herbst appliance: A cephalometric long-term study. Am J Orthod Dentofacial Orthop. 1993;103:510-20.
- [CrossRef] [Google Scholar]
- Cervical headgear therapy as a factor in obstructive sleep apnea syndrome. Pediatr Dent. 1999;21:39-45.
- [Google Scholar]
- Upper airway dimensions in Class II malocclusion. Effects of headgear treatment. Angle Orthod. 2007;77:1046-53.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging of the upper airway structure of children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2001;164:698-703.
- [CrossRef] [PubMed] [Google Scholar]
- Changes of tongue position and oropharynx following treatment with functional appliance. J Clin Pediatr Dent. 2007;31:287-90.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional cone-beam computed tomography analysis of enlargement of the pharyngeal airway by the Herbst appliance. Am J Orthod Dentofacial Orthop. 2014;146:776-85.
- [CrossRef] [PubMed] [Google Scholar]
- Pharyngeal airway dimensions: A cephalometric, growth-study-based analysis of physiological variations in children aged 6-17. Eur J Orthod. 2014;36:331-9.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in dentofacial structures in untreated Class II division 1 and normal subjects: A longitudinal study. Angle Orthod. 1997;67:55-66.
- [Google Scholar]






