Translate this page into:
Mandibular Incisor Position Changes do not Explain Increase in Keratinized Gingiva Height after Periodontally Accelerated Osteogenic Orthodontics
Address for correspondence: Prof. Donald J. Ferguson, Dubai Healthcare City, Bldg 27, Block D, Office 302, PO Box 53382, Dubai, United Arab Emirates. E-mail: fergusonloud@gmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Purpose
This study aimed to reexamine the relationship between mandibular incisor inclination, prominence and vertical changes in position, and keratinized gingival tissue (KT) height changes labial to the mandibular incisors after orthodontic treatment with and without augmented corticotomy (Cort).
Materials and Methods
Two orthodontically treated groups of 35 individuals each, with (Cort) and without (conventional [Conv]) alveolar decortication and augmentation bone grafting (periodontally accelerated osteogenic orthodontics [PAOO]), were matched for sample size, gender, mandibular premolar extractions, pretreatment age, posttreatment observation period, and pretreatment KT height in this case–controlled retrospective study. Pre- and post-treatment lateral cephalometric radiographs were evaluated for mandibular incisor vertical, inclination, and prominence changes.
Results
As reported previously (Wilcko 2015), KT height had significantly increased by 0.78 mm (P = 0.001) in the Cort group and decreased by 0.38 mm (P = 0.002) in Conv on an average of 1.5 years after completion of active orthodontic therapy. In this study, Cort mandibular incisors proclined and protruded significantly during therapy while Conv incisors did not. Changes in mandibular incisor inclination and prominence explained neither the decrease in keratinized gingiva height in Conv nor the KT height gain in Cort.
Conclusions
In spite of mandibular incisor proclination and protrusion, orthodontic therapy combined with alveolar decortication and augmentation bone grafting resulted in a clinically significant increase in keratinized gingiva height 1.5 years’ posttreatment.
Keywords
Accelerated tooth movement
keratinized tissue height
PAOO
Introduction
A significant increase in keratinized tissue (KT) height labial to the mandibular incisors was recently described postorthodontic treatment following augmented corticotomy (Cort) therapy compared to a tissue height decrease following conventional (Conv) orthodontics. Wilcko et al.[1] reported 1.5 years’ posttreatment that KT height gained an average of 0.78 mm as a consequence of alveolar decortication and augmentation bone grafting and lost 0.38 mm in a matched orthodontic sample without surgery. The authors asserted that the value-added protection of KT height increase after decortication and augmentation bone grafting offsets the concerns of orthodontic proclination or expanding mandibular incisors facially.[1] Given the ongoing concern within the orthodontic and periodontal clinical communities about gingival recession (GR) defect relative to position of teeth within the alveolus,[2] further documentation of mandibular incisor position changes relative to KT height changes, including vertical heights, is warranted.
Importance of keratinized tissue
The historical importance of KT height surrounding the dentition has been controversial and was summarized by Wilcko et al.[1] The clinical significance of KT and/or attached gingiva diminished during the past five decades.[3] Prior to the 1970s, a height (width or zone) of attached gingiva of at least 1 mm was considered necessary to maintain gingival health.[4] However, the importance of a sufficiently wide band of KT has been refuted by evidence-based studies. Height of attached gingiva was deemed an insignificant, nonpathogenic factor in periodontal health irrespective of oral hygiene being satisfactory or unsatisfactory.[1] There is a general consensus in scholarly literature that a certain quantity of gingiva is not essential for the maintenance of periodontal health or for precluding a GR defect,[1] especially if plaque control is satisfactory.[5]
However, more recent consensus position statements have emerged. Prospective and retrospective studies have shown that, in the presence of suboptimal plaque control and clinical inflammation, attachment loss and recession may result unless there is a minimum amount of KT. A minimum amount of 2 mm of KT with 1 mm of attached gingiva has been recommended under these circumstances.[6]
Periodontal plastic surgery is not justified to increase the apico-coronal width of the gingiva to prevent the development of soft tissue recession defect,[7] but is advocated to correct GR defect apical to the cementoenamel junction.[3,8,9] If orthodontic tooth movement is anticipated to be outside the alveolar housing in a patient with thin tissue biotype thereby increasing the risk of GR defect, periodontal plastic surgical procedure may be indicated to increase KT height and/or marginal gingival thickness.[1,6,10]
Mandibular incisor inclination and prominence
Most investigators report that KT heights labial to mandibular incisors do not change with changes in tooth vertical position,[11,12] inclination, or prominence.[13,14] However, both Choi et al.[15] and Artun and Krogstad[16] reported decreased width of attached gingiva after proclination of the mandibular incisors for decompensation in Class III surgery patients. Coatoam et al.[17] found orthodontic treatment unrelated to KT height labial to mandibular incisor but reported that KT height might decrease when lateral incisors were moved from a lingual to a more labial position.
Mandibular incisor GR is unrelated to proclination was the conclusion of a recent 15-year postorthodontic treatment study by Morris et al.[18] Most investigators have expressed little or no concerns about marginal soft tissue gingival status or health when mandibular incisor proclination or prominence is increased[19-21] in the absence of preexisting GR defects or if there is an adequate height of KT.[1] Renkema et al.[22] compared patients without pretreatment GR who were orthodontically treated resulting in nonproclined (<95°) and proclined (>100.5°) mandibular incisors’ outcomes; there were no differences in the number of individuals (~12%) demonstrating GR 5 years after orthodontic treatment. The authors concluded that the amount of proclination of lower incisors at the end of treatment neither seemed to affect the development of labial GR nor the change of clinical crown heights. In another study, Renkema et al.[23] reported that proclination, retroclination and/or maintaining mandibular incisors in their original positions did not affect the development of recessions 5 years after orthodontic treatment.
Wilcko et al.[1] summarized risk factors in previous scholarly literature relating GR and biotype to mandibular incisor inclination and prominence as follows: (1) proclination may result in GR, especially if proclined excessively, i.e., decompensating retroclined incisors in Class III malocclusion is a risk for GR, (2) inflammation from plaque increases the risk for GR, especially when teeth are moved facially, (3) thin biotype is a risk factor for GR, especially if mandibular incisors are moved facially, and (4) proclination results in biotype thinning and greater crown lengthening but not GR.
Orthodontic retention phase
A recent periodontal consensus report stated that orthodontic treatment and/or the retention phase may contribute to increasing the risk of onset of recession, and the relationship between orthodontic tooth movement and GR needed to be reassessed.[24] This consensus report cited Renkema et al.[25] who observed 8 years postorthodontics that the proportion of individuals with at least one recession was twice as great in orthodontically treated compared to untreated controls (35.0% vs. 16.7%, respectively, P = 0.003), and according to the results, the mandibular incisors are especially prone to GR defect. Renkema et al.[25] concluded that orthodontic treatment and/or retention phase promotes the development of GRs. However, Slutzkey and Levin[26] also reported the same finding in young adults with a history of GR, i.e., twice the prevalence of GR (22.9% vs. 11.4%, respectively, P = 0.001). Length of retention phase appears to be the greater risk factor for GR as Morris et al.[18] recently described postorthodontic treatment GR as an aging phenomenon related to the length of retention time and not related to mandibular incisor position; the authors speculated that labial bone thinness may be related to recession.
Periodontally accelerated osteogenic orthodontics
Orthodontic therapy combined with selective alveolar corticotomy and augmentation bone grafting, named periodontally accelerated osteogenic orthodontics or PAOO, was introduced in 2001.[27] PAOO protocol includes facial and lingual full-thickness flaps and selective alveolar corticotomy combined with augmentation bone grafting typically comprised of demineralized freeze-dried bone allograft and bovine bone wetted with clindamycin phosphate antibiotic.[28] A sulcular-releasing incision is used followed by full-thickness mucoperiosteal flap reflection ideally extended 5–10 mm beyond the apices of the roots. Bone may be activated with circumscribing corticotomy cuts, localized intramarrow penetrations, or a combination; the surgical trauma to the cortices should be in juxtaposition with only the teeth desired to be moved. Following the facial and lingual placement of the particulate bone grafting material over the activated bone, the flap must be sutured in its original position; nonresorbable/nonwicking suture material is recommended. The sutures must be left in place for a minimum of 2 weeks or even longer if still functional. If the sutures are removed prematurely before the epithelial attachment is re-established on the root surface,[29] the flap can potentially retract apically and result in root exposure. This is especially an issue if there is preexisting bony dehiscence; the use of resorbable suture material can also contribute to this type of problem.[1]
The increased keratinized gingival height labial to the mandibular incisors averaging 0.78 mm after PAOO therapy as reported by Wilcko et al.[1] has not been thoroughly studied in relation to mandibular incisor position changes. The purpose of the study was to further assess the relationship of mandibular incisor inclination, prominence, and vertical position changes during orthodontic treatment as an explanation of labial keratinized gingival height change with and without augmented corticotomy. The null hypothesis tested was that incisor position changes do not affect the height of keratinized gingiva labial to mandibular incisors in postorthodontic treatment patients with and without a history of PAOO therapy.
Materials and Methods
The approval of the Institutional Review Board at European University College was obtained to conduct this research project.
Sample
The sample comprised seventy patients with healthy, intact periodontium without recession defect treated with comprehensive orthodontic therapy. Primary target variable for the present study was on mandibular incisor position changes (inclination, prominence, and vertical height) in relationship to KT height changes previously reported.[1]
Selection criteria for all patients in this case–control study included the following: (1) comprehensive orthodontic treatment in the permanent dentition using fixed, straight wire orthodontic appliances of 0.022” slot size with and without premolar extractions, (2) postorthodontic treatment retainer wear with removable thermoplastic and/or Hawley-type retainers, and (3) availability of intraoral frontal occlusion photographs showing mandibular keratinized gingiva at pretreatment and at least 1 year following active orthodontic therapy.
Individuals were excluded from the study on the basis of any of the following criteria: (1) an inability to measure the labial KT on the intraoral frontal photograph, (2) pretreatment open bite malocclusion, (3) congenitally absent or orthodontically extracted mandibular incisor (s), (4) diagnosis of any syndrome including cleft lip and palate, and (5) a history of orthognathic surgery.
The sample was divided equally based on orthodontic treatment history with and without PAOO. From the private practices of William M and M Thomas Wilcko, the records of all patients, with no exception, treated with mandibular anterior alveolar corticotomy and augmentation grafting therapy (Cort), were screened using the study selection criteria. Patients who had been treated by conventional orthodontics (Conv) were then matched to the Cort sample for sample size, gender, mandibular premolar extractions, pretreatment age, length of posttreatment observation period as well as pretreatment KT height. The conventional orthodontic patient records from European University College archives were reviewed starting with the most current available, extending back no more than 2 years, and continued until matched groups were achieved.
Both study groups comprised 35 individuals with 69% of females, and the Conv sample represented one fewer lower premolar extraction patient. Length of posttreatment observation time for Conv was 15.9 and 19.4 months for Cort (P > 0.05). Mean pretreatment KT heights were no different (P > 0.05) between the Conv and Cort (3.24 vs. 3.52 mm, respectively) groups [Table 1]. Minimal pretreatment KT heights recorded for Conv and Cort were 1.61 and 0.69 mm, respectively.
| Sample description | Code | Size | Gender | L premolar extraction | Active Tx Time (months) | Post-Tx (months) | Pre-Tx KT height (mm) | ||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | No | Yes | ||||||
| Conventional orthodontics (removable retainers) | Conv | 35 | 11 | 24 | 30 | 5 | 22.1 ±6.8 | 15.9±13.6 | 3.24±0.8 |
| Corticotomy + grafting + orthodontics (removable retainers) | Cort | 35 | 11 | 24 | 29 | 6 | 7.1 ±1.7 | 19.4±12.9 | 3.52±0.9 |
KT – Keratinized tissue; Conv – Conventional; Cort – Corticotomy; L – Mandibular or lower (from Wilcko 2015)
Procedures
Surgery
Alveolar decortication and bone grafting were performed in Cort patients as described by Wilcko et al.[28] within 1 week from the date of placement of the fixed orthodontic appliance. A sulcular-releasing incision was used and not releasing incisions made in the mucosal tissues apical to the zone of keratinized gingiva. The full-thickness mucoperiosteal flap reflection was extended 5–10 mm beyond the apices of the roots. The bone activation was accomplished with circumscribing corticotomy cuts and intramarrow penetration proximate to the area of desired tooth movement using a high-speed handpiece number 2 round bur with copious irrigation. Cortical bone overlying the roots was intentionally injured if thick enough without threat to entering the periodontal ligament space or injuring the root itself; interproximal cortical bone was scarred with penetrations and/or circumscribing cuts. Following the placement of the particulate bone grafting material over the activated bone, the flap was sutured in its original position with nonresorbable/nonwicking suture material. The sutures were left in place for a minimum of 2 weeks to prevent retraction apically and root exposure, especially when preexisting bony dehiscence was present.[1]
Cephalometric measurements
Pretreatment (T1) and posttreatment (T2) cephalometric radiographs were used to measure and compare mandibular incisor inclination (mandibular central incisor axis to mandibular plane, i.e. L1-MnPl), mandibular incisor position in the vertical plane (mandibular central incisor tip distance perpendicular to gonion-to-menton line, i.e. L1-GoMe), and protrusion (mandibular central incisor distance from nasion-to-pogonion line, i.e. L1-NPo) [Figure 1].

- (a) Three cephalometric measurements were used to describe pre- to post-treatment changes in mandibular incisor position: inclination (L1-MP) in degrees, vertical (L1-Me), and protrusion (L1-NPg) in millimeters. (b) Chart showing mandibular incisor increment of change for conventional (Conv) and corticotomy (Cort) groups. Note, Cort had significant intragroup change (*) pre- to post-treatment for inclination and protrusion; intergroup comparisons showed that Cort change was significantly greater than Conv increment for protrusion (#)
Data were collected and stored in Excel and later transformed for use with the Statistical Package for Social Services software package, (SPSS software v.15.0.1, IBM, Armonk, NY) for analysis. Intergroup differences were compared using the independent t-test. One-way ANOVA parametric testing with Tukey’s post hoc test was performed to determine intergroup differences in KT height mean scores. The 0.05 probability level of significance was used for all testing purposes. Intraoperator reliability testing was conducted by repeating KT height measurements on five individuals from each of the two subgroups weekly for 5 weeks. Paired t-tests revealed no differences in the means, and reliability was judged as satisfactory.
Results
In the present study of matched samples, Cort mandibular incisors were significantly more retroclined at pretreatment than in the Conv group as measured by mandibular incisor axis to the mandibular plane, i.e., L1-MP (96.3° vs. 100.7°, P = 0.015). Likewise, vertical distance between mandibular incisor incisal edge to menton, i.e., L1-Me, was greater in Cort than Conv (47.0 vs. 40.6 mm, P = 0.000) at T1. At posttreatment, Cort L1 to Me height remained significantly greater than Conv (46.9 vs. 40.1 mm, P = 0.000). For T1–T2 increment of change, Cort mandibular incisors protruded significantly more (1.7 vs. −0.2 mm, P = 0.002) compared to Conv [Table 2 and Figure 1].
| Cephalometric variables | T1 | T2 | ||||
|---|---|---|---|---|---|---|
| Cort | Conv | P | Cort | Conv | P | |
| L1-MP (°) | 96.3 | 100.7 | 0.015 | 100.3 | 102.0 | NS |
| Ll-GoMe (mm) | 47.0 | 40.6 | 0.000 | 46.9 | 40.1 | 0.000 |
| Ll-NPog (mm) | 4.1 | 5.3 | NS | 5.7 | 5.1 | NS |
| T1 to T2 change | |||
|---|---|---|---|
| Cort | Conv | P | |
| Ll-MP change (°) | 4.0 | 1.3 | NS |
| Ll-GoMe change (mm) | −0.2 | −0.5 | NS |
| Ll-NPog (mm) change | 1.7 | −0.2 | 0.002 |
NS – Not significant; L1-MP – Mandibular central incisor inclination; L1-GoMe – Mandibular incisor vertical position; L1-NPog – Mandibular incisor protrusion; T1 – Pretreatment; T2 – Posttreatment; Conv – Conventional; Cort – Corticotomy
Paired t-testing demonstrated significant intra-group Cort changes in 2 of 3 cephalometric study variables during therapy, i.e., from T1 to T2; mandibular incisors proclined (96.3 vs. 100.3, P < 0.006) and protruded (4.1 vs. 5.7, P < 0.001). In contrast, there were no significant changes due to orthodontic treatment in any of the measured variables in the Conv sample [Table 3 and Figure 1].
| Cephalometric variables | T1 | T2 | P |
|---|---|---|---|
| Cort | |||
| LI-MP (°) | 96.3 | 100.3 | 0.006 |
| Ll-GoMe (mm) | 47.0 | 46.9 | NS |
| Ll-NPog (mm) | 4.1 | 5.7 | 0.001 |
| Conv | |||
| Ll-MP (°) | 100.7 | 102.0 | NS |
| Ll-GoMe (mm) | 40.6 | 40.1 | NS |
| Ll-NPog (mm) | 5.3 | 5.1 | NS |
Note that two of the three study variables changed significantly in the Cort sample. NS – Not significant; Conv – Conventional; Cort – Corticotomy; T1 – Pretreatment; T2 – Posttreatment; L1-MP – Mandibular central incisor inclination; L1-GoMe – Mandibular incisor vertical position; L1-NPog – Mandibular incisor protrusion
Discussion
The purpose of the present study was to reexamine mandibular incisor position changes in relation to KT height changes in matched samples with and without PAOO. In a previous publication, Wilcko et al.[1] described KT changes of the sample used in the present study as follows:
At 1.5 years’ posttreatment, KT height averaged significantly more for the Cort sample (4.3 ± 0.74 mm) when compared to the Conv group (2.9 ± 0.98 mm, P < 0.000). Moreover, the posttreatment KT height of all individual mandibular incisors was significantly greater (P ≤ 0.003) in the Cort sample [Table 2][1]
Mean KT height change decreased significantly from pretreatment to 1.5 years’ posttreatment for Conv (−0.38 mm, P = 0.001) patients. In contrast, mean KT height increased significantly for the Cort (0.78 mm, P < 0.000) patients [Table 3 and Figure 1][1]
Cort and Conv study groups were further assessed by dividing each sample into two groups above and below the 50th percentile level of mean pretreatment KT height. The Conv group’s KT height decreased significantly (−0.51 mm, P = 0.006) during treatment when mean pretreatment KT height was above 50th percentile but not below 50th percentile (−0.26 mm, P = 0.10). In contrast, the Cort group’s KT height increased significantly (1.28 mm, P = 0.000) during therapy when mean pretreatment KT height was below 50th percentile, but above 50th percentile, mean KT height change posttreatment was not statistically significant (0.26 mm, P = 0.194) [Figure 2].
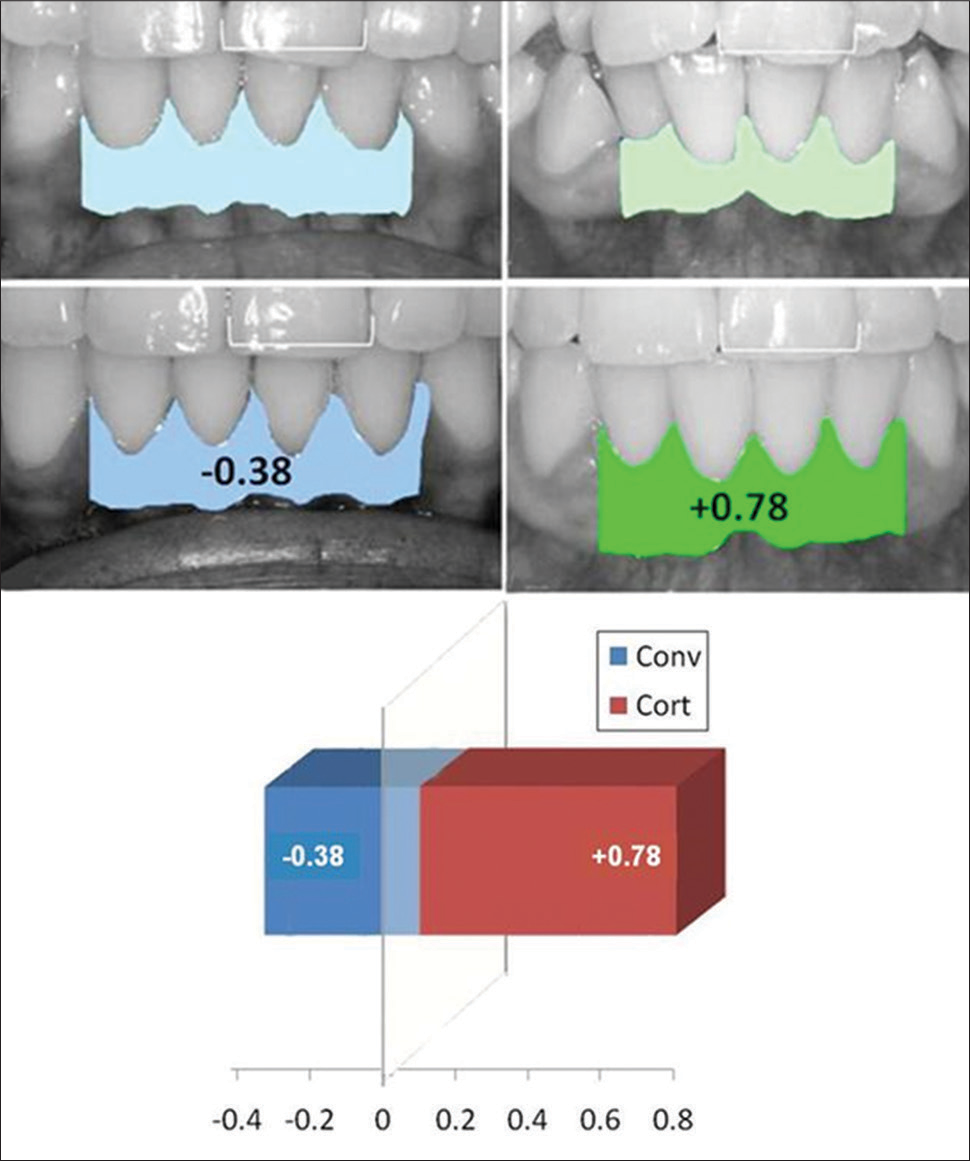 Figure 2
Figure 2- Keratinized tissue height of the four mandibular incisors decreased by 0.38 mm for the conventional (Conv) group and increased by 0.78 mm in the augmented corticotomy (Cort) group as measured after orthodontic treatment 15.9 and 19.4 months, respectively
The main finding of the present study is that mandibular position and/or changes appeared to have no effect whatsoever on KT height findings. Intuitively, increasing mandibular incisor proclination and prominence would seem to favor a KT height decrease, but the opposite was found when mandibular incisors became more prominent and proclined after augmented Cort. As described previously,[1] the likely explanation for increased KT height in the Cort group is the stretching of the full-thickness periosteal flap over the augmentation bone graft material.
Results of the present study differ from that of Wilcko et al.[1] in that the vertical positions of the mandibular incisors were assessed in the present study. Changes in vertical position were slight (P > 0.05) in both groups, and results of the present study are consistent with that of Wilcko et al.[1] for mandibular incisor inclination and prominence. Intragroup paired t-tests demonstrated in the Cort group significant proclination (96.3 vs 100.3 mm, P = 0.006) and protrusion (4.1 vs 5.7 mm, P = 0.001) during therapy; there were no significant (P > 0.05) treatment (T1 to T2) changes in the Conv group mandibular incisor positions.
In the present study, however, the Conv KT height was probably not influenced by labial orthodontic tooth movement as there was no significant change (P > 0.05) in either the proclination (L1-MP) or protrusion (L1-NPog) study variables. In contrast, the mandibular incisors in the Cort group increased significantly in proclination 4.0° (P = 0.006) and protrusion 1.7 mm (P = 0.001). Surprisingly, there was a significant increase in the Cort KT height which was opposite to what would be expected and counterintuitive.
Mandibular labial gingival biotype was not assessed in the present study and is a confounding factor. Zawawi et al.[30] reported that mandibular incisor proclination and protrusion are associated with thin gingival biotype; Cort group’s mandibular incisors were 3.4° less proclined than that of Conv group (96.3° vs. 100.7°, respectively, P = 0.015) at T1 but virtually the same at T2. Rasperini et al.[31] concluded that thin periodontal biotype and proclination movement were related to loss of KT height. Perhaps, the Conv group had thinner T1 biotype but the increase of 1.3° proclination T1–T2 likely did not influence the KT height loss for Conv patients found in the present study.
In the present study, the most logical explanation behind the significant increase in the KT height of the Cort group was the stretching of the full-thickness flap coronally over the labio-lingual bulk of augmentation grafting material. Although the main purpose of alveolar corticotomy and bone grafting is not to increase KT height, it would appear that the procedure results in this value-added outcome by reducing concerns about the development of GR defect after expanding mandibular incisors facially during orthodontic therapy.[1]
Conclusions
Two matched groups of orthodontically treated patients, with and without alveolar decortication and augmentation bone grafting, were compared. The samples were matched for sample size, gender, mandibular premolar extractions, pretreatment age, and posttreatment observation period as well as pretreatment KT height. Labial KT heights were increased on an average of 0.78 mm in Cort but decreased on an average of 0.38 mm in Conv. A summary of mandibular incisor inclination, prominence, and vertical position changes in relation to KT height changes is as follows:
Cort mandibular incisor position significantly proclined 4° and protruded 1.7 mm during orthodontic therapy but labial KT height increased on an average of 0.78 mm (P = 0.000)
Conv mandibular incisor position did not change significantly during orthodontic therapy but labial KT height deceased on an average of 0.38 mm (P = 0.002)
Mandibular incisor position changes explained neither the decrease in keratinized gingival height in Conv nor the KT height increase in Cort
Based on the conditions of this study, it may be concluded that PAOO therapy results in a clinically significant increase in KT height labial to mandibular incisors irrespective of mandibular incisor position changes. Moreover, the increase in KT height following PAOO is a value-added benefit of augmented Cort that eases concerns about mandibular incisor expansion.
Financial support and sponsorship
Nil.
Conflicts of interest
Authors D. Ferguson, U. Mazumder, and L. Makki claim no conflict of interest of any type related to the investigation entitled, “Mandibular incisor position changes do not explain keratinized gingiva height increase after PAOO.”
Authors W. Thomas Wilcko and William M. Wilcko have conflicts of interest related to the investigation entitled, “Mandibular incisor position changes do not explain keratinized gingiva height increase after PAOO;” they hold a patent related to the Accelerated Osteogenic Orthodontics and PAOO.
References
- Keratinized gingiva height increases after alveolar corticotomy and augmentation bone grafting. J Periodontol. 2015;86:1107-15.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between orthodontic treatment and gingival health: A retrospective study. Eur J Dent. 2014;8:373-80.
- [CrossRef] [PubMed] [Google Scholar]
- The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: Critical elements in design and execution. J Clin Periodontol. 2014;41(15):S123-42.
- [Google Scholar]
- The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43:623-7.
- [Google Scholar]
- Periodontal soft tissue non-root coverage procedures: A systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(2):S56-72.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontal soft tissue non-root coverage procedures: A consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(2):S73-6.
- [Google Scholar]
- Consensus report of session II In: Lang NE, Karring T, eds. Proceedings of the 1st European Workshop on Clinical Periodontology. Berlin: Quintessence; 1994. p. :210-4.
- [Google Scholar]
- Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J Clin Periodontol. 2014;41(15):S44-62.
- [Google Scholar]
- Indication and timing of soft tissue augmentation at maxillary and mandibular incisors in orthodontic patients. A systematic review. Eur J Orthod. 2014;36:442-9.
- [CrossRef] [Google Scholar]
- Gingival response to mandibular incisor intrusion. Am J Orthod Dentofacial Orthop. 2007;132:143.e9-13.
- [Google Scholar]
- The width of the attached gingiva during orthodontic treatment: A clinical study in human patients. Am J Orthod. 1985;87:224-9.
- [CrossRef] [Google Scholar]
- Periodontal status of mandibular incisors after pronounced orthodontic advancement during adolescence: A follow-up evaluation. Am J Orthod Dentofacial Orthop. 2001;119:2-10.
- [Google Scholar]
- Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop. 2006;130:6.e1-8.
- [Google Scholar]
- Periodontal consequences of mandibular incisor proclination during presurgical orthodontic treatment in Class III malocclusion patients. Angle Orthod. 2015;85:427-33.
- [Google Scholar]
- Periodontal status of mandibular incisors following excessive proclination. A study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofacial Orthop. 1987;91:225-32.
- [CrossRef] [Google Scholar]
- The width of keratinized gingiva during orthodontic treatment: Its significance and impact on periodontal status. J Periodontol. 1981;52:307-13.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of gingival recession after orthodontic tooth movements. Am J Orthod Dentofacial Orthop. 2017;151:851-9.
- [Google Scholar]
- A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Aust Orthod J. 2011;27:33-9.
- [Google Scholar]
- The effect of changes in lower incisor inclination on gingival recession. Scientific World Journal. 2015;2015:193206.
- [Google Scholar]
- Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatment. Angle Orthod. 2012;82:42-7.
- [Google Scholar]
- Gingival labial recessions and the post-treatment proclination of mandibular incisors. Eur J Orthod. 2015;37:508-13.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival recessions and the change of inclination of mandibular incisors during orthodontic treatment. Eur J Orthod. 2012;35:249-55.
- [Google Scholar]
- Clinical efficacy of periodontal plastic surgery procedures: Consensus report of Group 2 of the 10th European Workshop on Periodontology. J Clin Periodontol. 2014;41(15):S36-43.
- [Google Scholar]
- Gingival labial recessions in orthodontically treated and untreated individuals: A case-control study. J Clin Periodontol. 2013;40:631-7.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival recession in young adults: Occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134:652-6.
- [Google Scholar]
- Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9-19.
- [Google Scholar]
- Accelerated osteogenic orthodontics technique: A 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 2009;67:2149-59.
- [CrossRef] [PubMed] [Google Scholar]
- Biology of soft tissue wound healing and regeneration – Consensus report of Group 1 of the 10th European Workshop on Periodontology. J Clin Periodontol. 2014;41(15):S1-5.
- [Google Scholar]
- Gingival biotype in relation to incisors’ inclination and position. Saudi Med J. 2014;35:1378-83.
- [Google Scholar]
- Influence of periodontal biotype on root surface exposure during orthodontic treatment: A preliminary study. Int J Periodontics Restorative Dent. 2015;35:665-75.
- [CrossRef] [PubMed] [Google Scholar]






