Translate this page into:
Maxillary bone defects and their relationship to transverse maxillary discrepancies
Address for correspondence: Prof. Rafael Rivas-Gutierrez, Morelos 248 poniente Centro 63000 Tepic, Nayarit, Mexico. E-mail: rafarivas_8@hotmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Peña-Montero CA, Rivas-Gutierrez R, Sierra- Rosales E, Diaz-Peña R. Maxillary bone defects and their relationship to transverse maxillary discrepancies. APOS Trends Orthod 2016;6:251-5.
Abstract
Objectives
The relationship between the presence of bone defects (fenestrations and dehiscences) observed in lateral slices in computerized axial tomography (CAT) images and maxillomandibular transverse discrepancies was determined.
Methods
The sample was composed of 160 CAT scan files, corresponding to 9–25-year-old patients, which had been taken prior to orthodontic treatment at a radiology center in Guadalajara, México, from 2009 to 2012. They were grouped by age, and we identified bone defects in maxillary teeth (first and second premolars and first molars). The maxillary (JL-JR) and mandibular (GA-AG) widths were measured, and the maxillomandibular discrepancy ([GA-AG]-[JL-JR]) was calculated. Chi-square and t-tests were performed.
Results
The values of maxillomandibular discrepancies increased with the age of the patient. There was no association between the magnitude of the maxillomandibular discrepancy and the presence of bone defects. The gender of the individual was not a decisive factor in whether bone defects were present.
Conclusion
Bone defects occur in the vast majority of patients pretreatment regardless of the magnitude of the maxillomandibular discrepancy.
Keywords
Dehiscence
fenestration
maxillomandibular discrepancy
tomography
INTRODUCTION
Orthodontic tooth movement is a permanent physiological phenomenon that takes place between teeth and the alveolar bone to enable the teeth to adapt to skull-facial growth and development.[1] To produce dental mobilization, the bone surrounding the tooth must be remodeled, selectively disappearing in some areas while growing in others.[2] One of the desired orthodontic objectives is posttreatment stability, which highly depends on correct assessment in three planes during diagnosis. The assessment of the skeletal transverse discrepancy between the maxillary and the mandibular widths helps clinicians diagnose crossbites and relate them to periodontal responses, dental instability due to camouflage, and some dentofacial asymmetries.[3]
Excessive orthodontic forces, such as dental slope and expansion, can produce periodontal attachment loss, compromising such stability.[4,5]
There is literature available on adverse periodontal effects such as fenestrations and dehiscences, which affect tooth support and the close relationship with the transverse discrepancy, as well as the convenience of considering such a discrepancy at the moment of diagnosis.[6]
Dehiscences are defects present in the slot gingival margin that reflect the loss of buccal, lingual, or palatal cortical alveolar bone and affecting the margin of the alveolar bone by resulting in root denudation with or without a gingival recession. Fenestrations are those that are limited to the partial loss of alveolar cortical bone, where a part of the root tip is exposed without affecting the bone margin.[6-8]
It has been reported that bone defects are present in ~20% of the teeth, most often in the buccal bone and often bilaterally.[9] Several possible causes have been mentioned, such as developmental abnormalities, orthodontic movements, periodontal and endodontic diseases, trauma from occlusion, and size and position of teeth coupled with certain predisposing factors such as prominent contours of the root, malposition, protrusions, and pro-inclinations of the combined root with thin bone tables, which can complicate the outcome of any procedure either surgical or orthodontic.[10,11]
Through the posteroanterior (PA) cephalogram, one can assess and identify not only skeletal asymmetries but also transverse skeletal dysplasias.[8] For the identification of skeletal crossbites and the evaluation of the problem, the use of PA cephalograms is recommended. This allows the clinician to analyze skeletal discrepancies and to make a more accessible and reliable diagnosis of the patient’s problem.[12] Volumetric cone-beam computerized axial tomography (CAT) is one of the most valuable medical diagnostic imaging tools. The versatility of this technique makes the scan highly desirable for the precise study of images of a wide variety of maxillofacial structures, such as the maxilla, mandible, and temporomandibular joint and provides good-quality images of the state of cortical bone and the tooth roots.[13]
MATERIALS AND METHODS
This was a descriptive, observational, and cross-sectional study. It was conducted with CAT scan images obtained from radiographic files of a radiology center in the city of Guadalajara, Mexico, corresponding to patients in whom studies had been conducted prior to their undergoing orthodontic treatment from 2009 to 2012. All scans were from existing case files, and thus none was prescribed specifically for the purposes of this study.
Through stratified random sampling, 160 scans were selected, 20 TAC per age group. Inclusion criteria specified that patients were from 9 to 25 years of age with the premolars and/or maxillary first molars fully erupted and with the complete formation of the root. CAT scans of patients with evident transverse maxillomandibular skeletal discrepancy were excluded as were those TACs in which we observed late tooth eruption. We classified files of the population into eight age groups, from age 9 to a final group that included individuals from 16 to 25 years of age.
The following variables were considered: Age, gender, cross-maxillomandibular discrepancy, fenestrations (frequency and location), and dehiscence (frequency and location).
Observation and measurement were performed only by a researcher who was previously trained by an imaging expert on the tomographic image display, as well as on the software for managing and working with such images. Up to 30 TACs were analyzed per day, to avoid eyestrain for the examiner.
The maxillomandibular transverse measurement was conducted with image scan analysis software (Dolphin Imaging and Management Solution, Chatsworth, Cal. USA). Prior to the measurement, soft tissues were removed from the scan so that only bone tissue would be assessed. The image was taken from a side view, with the Frankfort horizontal plane parallel to the floor, and the vertebrae were erased by a software feature to the entrance of the meatus to facilitate the identification of anatomical landmarks in the measurement from a PA view. Figure 1 shows how the three-dimensional image was converted to a two-dimensional radiographic view, and we transversely measured the maxilla (jaw width, JR-JL) and the mandible (mandibular width, AG-GA), taking into account the reference points from the Ricketts frontal analysis.
The maxillomandibular discrepancy of each of the individuals was calculated according to the following formula: maxillomandibular discrepancy = mandibular width − maxillary width.

- Transverse measurement of the maxilla (JL-JR) and the mandible (AG-GA)
We used the analysis software Implant Viewer 2, (Anne Solutions. Sao Paulo, SP, Brasil) to identify bone defects in the images. We observed bone defects present in the maxillary first molars for the eight age groups, while for the last three age groups (14 years, 15 years, and 16–25 years old), we observed defects in premolars and maxillary first molars. Figure 2a shows how sagittal slices were made for every 2 mm and determined the presence of fenestrations when bone loss did not involve the alveolar crest, while Figure 2b shows the presence of dehiscence with bone loss >2 mm and involved the alveolar crest.

- Identification of bone defects. (a) Distal view of the upper first molar. The presence of a fenestration can be seen at the level of the middle third of the root. (b) Distal view of the upper first molar. The continuity of bone loss compromising the gingival margin is observed
Average values and standard deviations of the maxillary and mandibular width, as well as the maxillomandibular discrepancies, were calculated by age group. We also calculated the frequency of bone defects and the magnitudes of the cross-maxillomandibular discrepancies by age group and gender. Finally, the association between the presence of bone defects and the magnitudes of the maxillomandibular transverse discrepancies was analyzed by t-test, Chi-square, and ANOVA.
RESULTS
Of the 160 scans analyzed, 59% were from females. Table 1 and Figure 3 show how the average values of the maxillary and mandibular width increased with age, with the most significant increase in width in the mandible, which caused the cross-maxillomandibular discrepancy to increase with age.
| Age | JL-JR | AG-GA | Discrepancy | SD± |
|---|---|---|---|---|
| 9 | 61.21 | 72.44 | 11.08 | 3.07 |
| 10 | 63.78 | 76.135 | 12.355 | 3.67 |
| 11 | 63.985 | 76.7 | 12.715 | 3.62 |
| 12 | 65.97 | 79.09 | 13.12 | 3.65 |
| 13 | 66.81 | 80.04 | 13.23 | 3.65 |
| 14 | 67.9 | 81.7 | 13.88 | 2.87 |
| 15 | 68.24 | 82.45 | 14.205 | 4.98 |
| 16-25 | 69.235 | 84.4 | 14.655 | 3.48 |
| Total average | 65.9 | 79.12 | 13.16 | 3.74 |
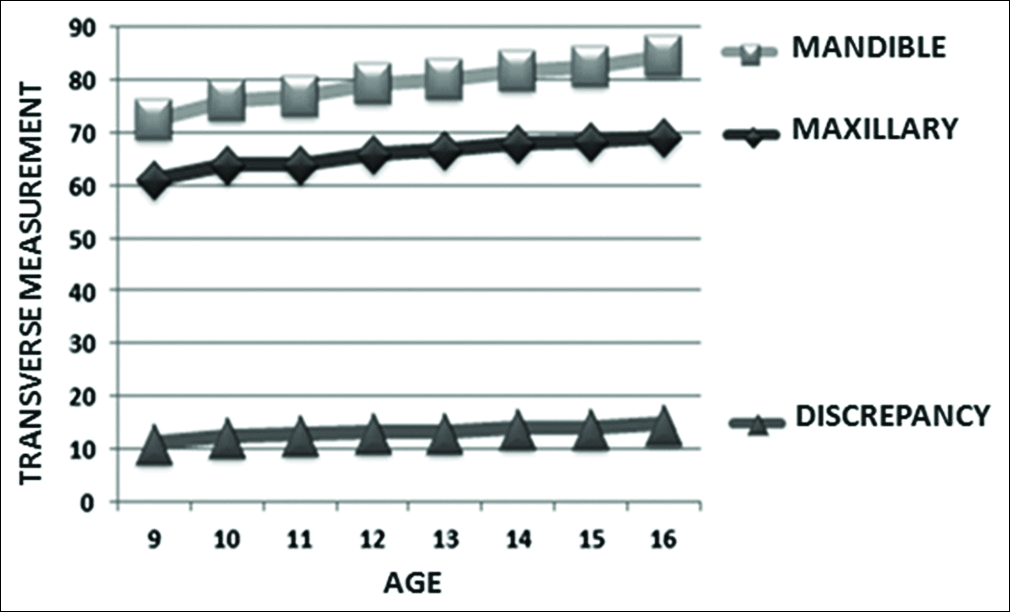
- Transverse maxillomandibular growth (mm)
Figure 4 shows the distribution according to the magnitude of transverse discrepancy, we can see that in 72% of cases, the value of the discrepancy was smaller than one standard deviation (central value of the discrepancy range), with the remaining 28% distributed symmetrically toward the ends, away from the average value, and with both 13.5% and 14.5% having a discrepancy value.

- Distribution according to the magnitude of the transverse discrepancy
Figure 5 shows the prevalence of dehiscences and fenestrations. Eighty percent of the sample had some type of bone defect (fenestration or dehiscence), with the group presenting only one dehiscence or fenestration being the largest.
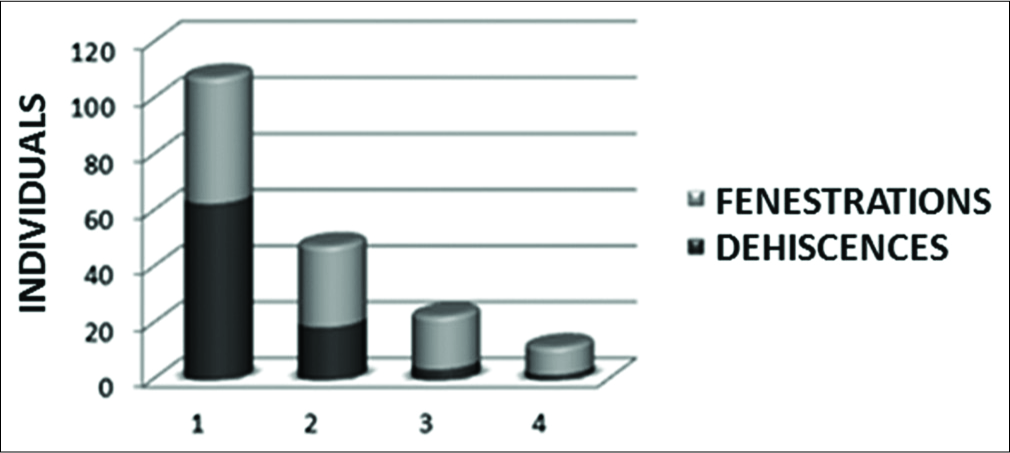
- Prevalence of dehiscences and fenestrations
We used a Chi-square test to determine whether there was a correlation between the presence of bone defects and the magnitude of the maxillomandibular discrepancy. We found no relationship whatsoever between the two variables (R2 = 0.008). Both the TACs of individuals with altered maxillary-mandibular discrepancies and those of individuals who had no alterations presented similar percentages of bone defects (fenestrations or dehiscences).
Figure 6 shows the prevalence of bone defects by age group; there is an increase in the number of fenestrations with the age of the individuals.

- Prevalence of bone defects by age group
We also analyzed the prevalence of bone defects according to the magnitude of the discrepancy and the specific tooth. Figure 7 shows how (where we observed only the upper first molars) there is no relationship between the magnitude of the maxillomandibular transverse discrepancy and the presence of bone defects (Chi-square test) in the eight groups. This was consistent with the results observed in the last three groups, in which first molars and first and second maxillary premolars were analyzed.

- Prevalence of bone defects by type of maxillomandibular discrepancy and by tooth
Finally, Figure 8 shows the correlation between the presence of bone defects with the gender of the study population, noting that there were no statistically significant differences, and we concluded that there was no relationship between the presence of bone defects and gender.

- Relationship between bone defects and type of maxillomandibular discrepancy by gender
DISCUSSION
Dehiscences and fenestrations are two defects commonly present where the root is devoid of bone, and the root surface is covered only by the periosteum and overlying gum. The prevalence of bone defects is of great interest to orthodontists since one can alert patients to the fact that such defects are common in the population and that they are not caused only by orthodontic movement. The treatment of these defects has focused on the repair or regeneration of lost structures by different techniques, materials, or substances. [11,14]
Studies on transverse changes have reported significant differences in facial width, maxillary width, and mandibular width for each age group and gender.[15-23] This is consistent with the results of this study relative to the increase in maxillary transverse dimensions as age increases in periods of high growth.
Melsen and Allais mentioned that the presence and severity of dehiscence increase with age, unlike our study population, in whom fenestration defects were more prevalent in the older age groups.[24]
In his studies, Vanarsdall emphasized the critical importance of skeletal differences between maxillary and mandibular width, highlighting that an undiagnosed transverse bone discrepancy results in an adverse periodontal response, unstable dental camouflage, and reduced dentofacial esthetic.[25] In our study, we found no relationship between the magnitude of the discrepancy and the presence of bone defects.
CONCLUSION
Bone defects occur in the vast majority of patients pretreatment regardless of the magnitude of the maxillomandibular discrepancy. Maxillary and mandibular transverse discrepancies and fenestrations tend to increase with age. The gender of the individual was not a decisive factor in whether bone defects were present. We suggest that clinicians keep these findings in mind since they often go unnoticed during diagnosis and treatment planning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Influence of maternal and infant formula in mandibular growth in neonates. (Bachelor Thesis) Lima, Peru. School of Dentistry. National University of San Marcos
- [Google Scholar]
- Effects of mandibular orthognathic treatment on mucogingival tissues. J Periodontol. 1985;56:727-33.
- [Google Scholar]
- The effect of orthodontic tilting movements on the periodontal tissues of infected and non-infected dentitions in dogs. J Clin Periodontol. 1977;4:278-93.
- [Google Scholar]
- Treatment of labial fenestration of maxillary central incisor. Endod Dent Traumatol. 1996;12:104-8.
- [Google Scholar]
- Prevalence of dehiscences and fenestrations in modern American skulls. J Periodontol. 2001;72:722-9.
- [Google Scholar]
- Clinical Periodontology (8th ed). Mexico City: Mc Graw Hill; 1988. p. :70-6.
- Cephalometrics in orthodontic diagnosis (1st ed.). Buenos Aires, Argentina: Ed. La Medica; 1956.
- Follow-up study of apicoectomized teeth with total loss of the buccal bone plate. Oral Surg. 1985;59:78-81.
- [Google Scholar]
- Endodontology (2nd ed). Philadelphia: Lea and Febiger; 1988. p. :81-117. Ch. 4
- Perspectives in the clinical application of cephalometrics. The first fifty years. Angle Orthod. 1981;51:115-50.
- [Google Scholar]
- Dehiscence and fenestration in patients with class I and class II division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138:133.e1-7.
- [Google Scholar]
- A longitudinal cephalometric study of transverse and vertical craniofacial growth. Am J Orthod Dentofacial Orthop. 1993;104:471-83.
- [Google Scholar]
- New posteroanterior cephalometric norms: A comparison with craniofacial measures of children treated with palatal expansion. Angle Orthod. 2001;71:285-92.
- [Google Scholar]
- Mathematical correlations between linear skeletal transverse dimensions obtained from Ricketts frontal computerized cephalometric analysis. Rev Odontol Cienc. 1998;13:115-32.
- [Google Scholar]
- Data and patterns of transverse dentofacial structure of 6-to 15-year-old children: A posteroanterior cephalometric study. Am J Orthod Dentofacial Orthop. 1992;101:465-71.
- [Google Scholar]
- Landmark identification in computerized posteroanterior cephalometrics. Am J Orthod Dentofacial Orthop. 1987;91:57-61.
- [Google Scholar]
- Posteroanterior cephalometric norms in Turkish adults. Am J Orthod Dentofacial Orthop. 2005;127:324-32.
- [Google Scholar]
- Transverse growth of the maxilla and mandible in untreated girls with low, average, and high MP-SN angles: A longitudinal study. Am J Orthod Dentofacial Orthop. 2005;128:716-23.
- [Google Scholar]
- Growth in width of the maxilla studied by the implant method. Scand J Plast Reconstr Surg. 1974;8:26-33.
- [Google Scholar]
- Transverse development of the human jaws between the ages of 8.5 and 15.5 years, studied longitudinally with use of implants. J Dent Res. 1990;69:1298-306.
- [Google Scholar]
- Factores que intervienen en las dehiscencias durante la protrusión de incisivos inferiores. Am J Orthod. 2005;127:552-61.
- [Google Scholar]






