Translate this page into:
Orthodontic management of impacted maxillary canines

*Corresponding author: Krister Bjerklin, Department of Orthodontics, The Institute for Postgraduate Dental Education, Jönköping, Sweden, Europe. krister.bjerklin@mau.se
-
Received: ,
Accepted: ,
How to cite this article: Bjerklin K. Orthodontic management of impacted maxillary canines. APOS Trends Orthod 2020;10(2):64-71.
Abstract
The prevalence of impacted maxillary canines is 2–3%. In Caucasian populations, it is reported to be more palatally displaced than buccally, with the opposite trend seen in Asian populations. At the ages of 9–11 years, the position of the canine germ should be diagnosed, for most children through clinical supervision. In 7–10% of children, the clinical investigation must be supplemented with radiographic investigation, in most cases with intraoral radiographs. About 50% of impacted canines cause root resorption of the adjacent teeth. To detect the severity of resorption, cone-beam computed tomography is necessary. Root resorptions on incisor roots occur most often at 11–12 years of age. Early diagnosis of ectopically positioned maxillary canines is very important. In cases with palatally displaced canines and no root resorptions, extraction of the primary canines has been found in different studies to give good results. If the permanent canine has not started to normalize its position within 12 months, orthodontic treatment must be taken in consideration. Often, this is done by surgical exposure and orthodontic traction of the canine out into the dental arch.
Keywords
Maxillary canine
Impaction
Orthodontics
INTRODUCTION
The maxillary canine is, after the maxillary first permanent molar, the most important tooth for occlusion, because of its anatomy and its position in the dental arch where “cuspid protection” is fundamental to its function. It is also important to keep an individualized and appropriate intercanine distance with a view to having good esthetics.
The canine is diagnosed as impacted when its normal eruption time is significantly exceeded compared to the contralateral canine or the premolars. The canine can be impacted because of an eruption obstacle or ectopic position. Other reasons for canine impaction can be that the maxillary canine follows a more difficult and tortuous path of eruption than any other tooth. It starts high up in the maxilla at the age of 3–4 years, and then it comes with its crown directed mesially and somewhat lingually. It moves toward the occlusal plane, gradually up-righting itself until it seems to strike the distal aspect of the root of the lateral incisor. It then seems to be deflected to a more vertical position.[1]
The etiology is not stated, but two theories are discussed in the literature. The guidance theory suggests that the canine lacks guidance along its normal eruption path. An association has been shown between agenesis or small size of the lateral incisors and palatally displaced canines.[2-4] The genetic theory is based on familial factors. A strong genetic influence in cases with small teeth, or peg-shaped, and missing lateral incisors has been shown in different studies.[5-7] The maxillary permanent canine is, after the third molar, the most frequently impacted tooth. When impacted maxillary canines are undiagnosed and untreated, there is a risk for resorption of the adjacent teeth. The maxillary lateral incisor root is the tooth most commonly affected by ectopic position of the canine [Figure 1].
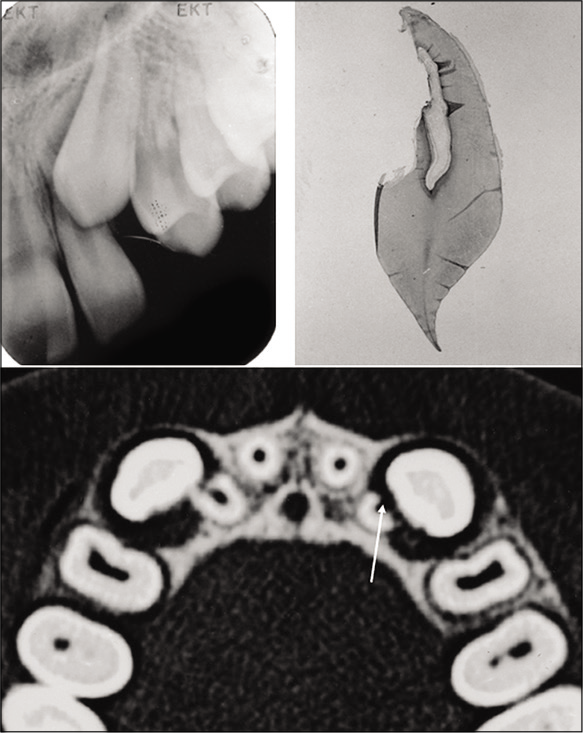
- A 12-year-old boy with the canine overlapping the lateral incisor root. Severe root resorption can be seen on the 3D radiograph, white arrow, as well as on the extracted lateral incisor.
Early detection of an impacted maxillary canine is important as resorption of adjacent incisor roots often starts at 11–12 years of age.[8]
IMPACTION
The prevalence of impacted maxillary canines is 2–3%; it is more common in females than in males. Bilateral impactions are seen in about 8% of patients with impacted canines.[9-12]
In 1983, Jacoby[13] published an article where 46 maxillary unerupted canines had been treated during the past 6 years. Forty were palatally impacted and six were labially unerupted. He stated that 85% of impacted maxillary canines are palatally displaced and he also concluded that labially unerupted canines frequently present different degrees of arch-length deficiency.[13] Later studies showed that the palatally displaced frequency is between 40% and 60%.[8] There are, however, ethnic variations of the prevalence. It seems like children from Asia have more buccally displaced maxillary canines than palatally impacted. In a Korean study of 148 children, the authors found 3 times more buccally displaced than palatally displaced canines.[14] Among 215 Chinese children with impacted maxillary canines, the ratio between the buccal and palatal location was 2.1:1.[15] In 533 Southern Chinese children and adolescents, 624 impacted maxillary canines were found in a population of 26,039. In the 442 subjects with unilateral impactions, 49.8% were buccally displaced and 43.9% were palatally displaced. The remaining 6.3% were found in the middle of the arch.[16] Oliver et al.[17] found that the Asian population had more buccally impacted maxillary canines than the Caucasian population.
The total frequency of impaction of maxillary canines is, however, equal between Caucasian and oriental populations at 2–3%.
DIAGNOSTICS
The diagnosis of impaction or an ectopic position of maxillary canines is usually made by the general practitioner after clinical and radiographic examination. For most children, a clinical supervision including digital palpation at the age of 9–11 years is enough to settle the position of the canine. There are cases reported with severe resorptions as early as the age of 7, as well as resorptions in cases with normal eruption of the maxillary canines.
The canine bulge should be palpable apical to the primary canine. Signs indicating that the canine position is ectopic or impacted are as follows:[1,18]
Absence of a normal labial canine bulge or a marked difference in the canine bulge between the right and the left sides at the palpation
Presence of a palatal bulge
Delayed eruption of a permanent canine or prolonged retention of a primary canine
Distal tipping or migration of the lateral incisor
A widened canine dental follicle, as seen on periapical intraoral or panoramic radiographs.
Most children with suspicious maxillary canines should be identified and the position of the maxillary canines checked during the period of 9–11 years of age.[10] In 7–10% of children, the clinical investigation must be supplemented with a radiographic investigation. This radiographic investigation includes, in most cases, intraoral radiographs.
Impacted maxillary canine has a close association with other tooth and eruption disturbances.[3,4,19-24] Ectopic eruption of the maxillary first permanent molar is normally diagnosed at the age of 6–7 years. The prevalence for impacted maxillary canines, in groups of children with ectopic eruption of maxillary first permanent molar or small sized maxillary lateral incisors is far higher than 2%; these patients can be considered at risk in this respect.[19,23]
EARLY MANAGEMENT
Early diagnosis of impacted maxillary canines is very important. When encountering a palatally displaced canine in a child 9–11 years of age, the first step is to analyze if there is root resorption of the adjacent teeth or not. If no resorption or any suspicious resorption can be seen, extraction of the primary canine is recommended to try to prevent impaction of the permanent canine [Figure 2]. Several studies have reported the effectiveness of extraction of the primary canine only or in combination with other treatments such as headgear, transversal expansion, or a transpalatal arch.[25-31] The ectopically positioned canines should normalize or at least start the normalization of eruption direction within a 12-month period. If not, some other treatment should be taken into consideration.
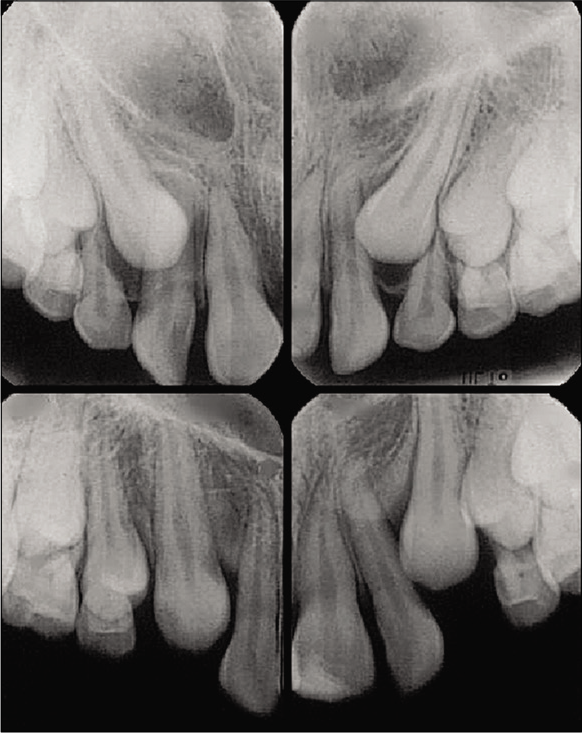
- At the age of nine, the canines were not palpable buccally, but there was suspicion of palatal displacement. Intraoral radiographs were taken and the primary canines were extracted. Nine months later, a favorable change in the eruptive pathway was seen, leading to uneventful eruption.
Ericson and Kurol[25] introduced a method to evaluate and measure the position of the canine on a panoramic radiograph in five vertical sectors and an alpha angle, i.e., the angle between the long axis of the canine and a vertical midline [Figure 3]. This method has since been used in a great number of studies.
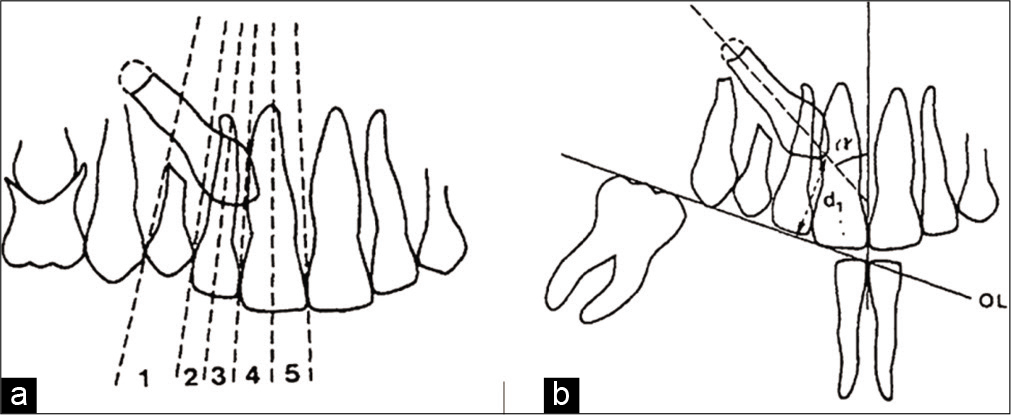
- (a) Reference lines for the sectors of the canine crown on panoramic radiography. (b) Distance from the canine crown to occlusal plane d, and canine inclination to midline (alpha angle) also measured by panoramic radiography (Ericson and Kurol 1988).
Studies have shown that the alpha angle and sector position of the crown are good predictors of which palatally displaced canines can be extracted with successful results. The best result of extraction of the primary canine can be expected when the canine crown is in sectors 2 or 3, the alpha angle is between 20 and 30°, and the patient is 11–13 years of age. Older patients have less successful results.[32]
RESORPTIONS
About 50% of impacted maxillary canines cause resorption of the adjacent lateral incisor or sometimes on both lateral and central incisors.
Resorption of incisor roots due to ectopically positioned maxillary canines occurs most often in the age groups between 11 and 12 years, but can occur earlier. In most cases, it occurs in combination with ectopically positioned maxillary canines, but can occur when the canine erupts normally as well. With limited apical resorption, good healing can be seen and the tooth can function without any further problems [Figure 4].
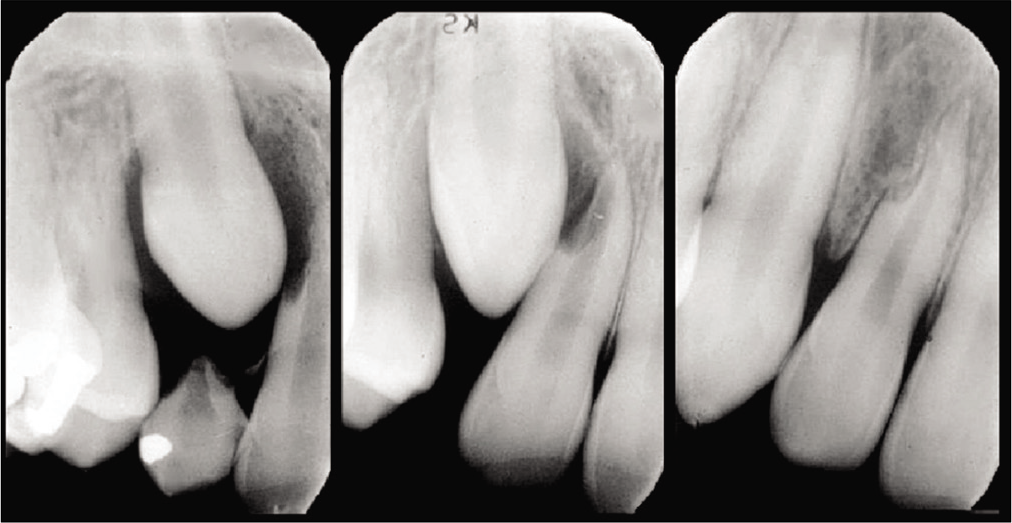
- Normal eruption path of the maxillary right canine, but with a rare instance of resorption of the lateral incisor root. Subsequently, some repair was evident, and the lateral incisor functioned as a normal healthy tooth.
After extraction of severely resorbed lateral incisors or in cases with agenesis of a lateral incisor, close check-up is important. Although there is space enough in these cases, there is a risk of root resorption of the central incisors [Figure 5].

- Even when there are congenitally missing lateral incisors and no crowding, canines can be in ectopic position and cause resorption of the central incisor roots. Severe root resorptions on both central incisors are evident on the 3D radiographs. On the intraoral photo, we can see that there is space enough for the canines between the central incisor and the first premolar. The intraoral radiographs show normal resorption only on the left primary canine.
It has been said, in the literature, that an enlarged dental follicle to an impacted maxillary canine can cause root resorption of the neighboring incisor and that there is a risk of cystic degeneration. There is no evidence confirming this; in fact, the opposite has been shown.[33] The resorption of the permanent maxillary incisor is caused by physical contact between the crown of the canine and the incisor root. An enlarged dental follicle only tells us that the canine is out of its normal position, i.e., it is palatally or buccally displaced.[34]
RADIOGRAPHY
When the clinical examination cannot settle the position of an unerupted maxillary canine at the age of 9–11 years, the investigation must be supplemented by a radiographic investigation. This is the case in 7–10% of these children. In most cases, intraoral radiographs or panoramic radiographs are enough. It is, however, often difficult to detect resorptions buccal or palatal to the roots with intraoral radiographs, because of overlapping of the impacted canine. Even resorptions to the pulp may be overlooked on intraoral films.[9] A study showed that lingual resorptions in the middle third of incisor roots were not detected until they reached a level of reduction corresponding to 3.5 mm.[35] In these cases, cone-beam computed tomography (CBCT) must be used to detect resorption [Figure 1].
Several studies have clearly demonstrated significant advantages with 3D imaging in the management of impacted canines.[36-41] With the use of 3D investigation, 50% more incisor root resorptions can be detected than with intraoral and panoramic radiography.[42] In a CBCT study, where all patients 8–17 years of age (mean 12.2 years) whowere referred to a department of dental radiology because of impacted maxillary canines, during a 6-year period, root resorption on at least one adjacent tooth was detected in 67.5%.[43]
The treatment plans without 3D radiograph information were changed in 35 (43.7%) of the 80 children after obtaining information in the 3D investigation. Even severe root resorptions were often difficult to detect on intraoral and panoramic radiographs.[44]
In a study of 156 impacted maxillary canines, 39% were positioned labially or distolabially, 50% palatally or distopalatally, 5% apically, and 6% between the central and lateral incisors. There were resorptions on 58 lateral incisors, 14 central incisors adjacent, and in 8 patients on both central and lateral incisors. The resorptions on the lateral incisors were found on the middle third of the root in 43% and 60% of the resorptions were severe, i.e., to or through the pulp.[11]
Similar results have been presented.[14] In a study performed in China, resorptions on the adjacent premolars were also found and resorptions to the pulp were more common on the central incisors than on the lateral incisors.[15]
There are very few long-term follow-up studies of incisor root resorptions induced by impacted maxillary canines. When the canine can be distanced from the incisor root before there is a severe resorption, it seems to be a good long- term prognosis for the resorbed incisor.[45-48]
LATE MANAGEMENT
When extraction of the primary canines or a combination of extraction and cervical headgear, rapid maxillary expansion or a transpalatal bar has failed, or the canine is impacted buccally, the next step is surgical exposure of the canine and fixed orthodontic appliances.
Late management means 13–15 years of age. The right time to start with exposure depends on the dental development and the risk of resorption of the incisor roots. It is important to know if there are root resorptions involving the neighboring incisors. Especially in extraction cases, it is not a high quality treatment to extract premolars and leave severely resorbed incisors. The radiographic examination is very important, as without CBCT examinations, there is a high risk of leave severely resorbed incisors and removing healthy premolars.[8]
Surgical exposure
Two treatment strategies of surgical exposure are most often used, i.e., closed exposure and open exposure.
In the closed technique, a mucoperiosteal flap is surgically opened, the bone to the tooth is removed, and a metal pad with a gold chain is bonded to the tooth. The flap is then sutured back with the chain or the ligature, coming out in the proper place for the best attachment to a fixed appliance system.
In the open exposure technique, the soft tissue and the bone are removed, followed by placing the canine in its right position in the dental arch by orthodontic treatment. It is important that the bone is removed to the broadest prominence of the crown with healing around the crown under surgical dressing. Sometimes, it can be valuable to make a composite build-up to ensure that the gum will not cover the tooth.
There are, however, considerable variations in both of these modalities. Almost all articles comparing open and closed techniques study palatally displaced maxillary canines. Variables studied include surgery time, total orthodontic treatment time, complications, patient perceptions, periodontal outcomes, and esthetics. There have been very few or no differences between the two groups reported. Becker et al.,[49] stated that because of the wide spectrum of factors, it is difficult to show a preference for one surgical technique over another. In a systematic review performed in 2018,[50] the authors concluded that there were no differences between the two techniques regarding post-operative pain, periodontal outcome, and esthetic appearance. The surgical procedure is, however, shorter in the open exposure group. Comparison between the two techniques in an RCT (2018)[51] showed that regarding unilateral impacted canines, there were no differences in surgery time or post-operative complications. However, in the open group with bilateral impacted canines, the patients reported more post-operative pain.[51] Forced-eruption time can be significantly reduced using ostectomy-decortication [Figure 6]. For a detailed description of the ostectomy-decortication technique see Wilcko et al.[52] and Ferguson et al.[53] In a study with 118 patients, 57 treated with ostectomy-decortication and 61 with open-closed surgical exposure, forced-eruption time was on average 6.6 months for the ostectomy-decortication group and 21.0 months for the open-closed surgical exposure group.[53] Forced-eruption time is the time between surgery date and date the canine which was tied into the orthodontic arch wire in a position similar to the adjacent teeth.
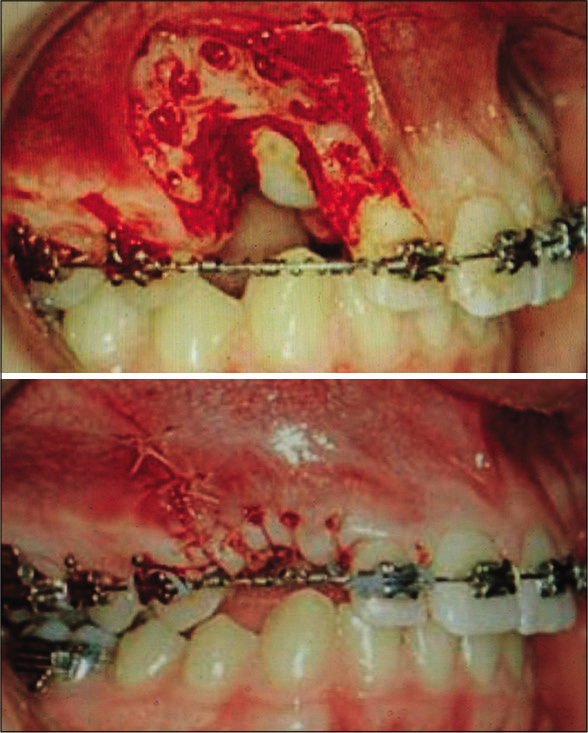
- (Top) Ostectomy-decortication. A full-thickness flap is opened, bone is removed and cortical bone penetrations (decortication) surrounding the impacted canine. (Bottom) Flap closure over the surgical exposure (Ferguson et al., 2019).
Orthodontic treatment
Before orthodontic traction starts, it is important to know if there is any resorption of the neighboring roots. When there is root resorption or a high probability of root resorption, it must be taken in consideration if the resorbed tooth must be extracted or if it is possible to keep it. If the tooth is allowed to remain, the canine must first be moved from the incisor, before traction can start in the alveolar crest. There are a number of different ways to move the canine away from the incisor; for examples, [Figure 7].
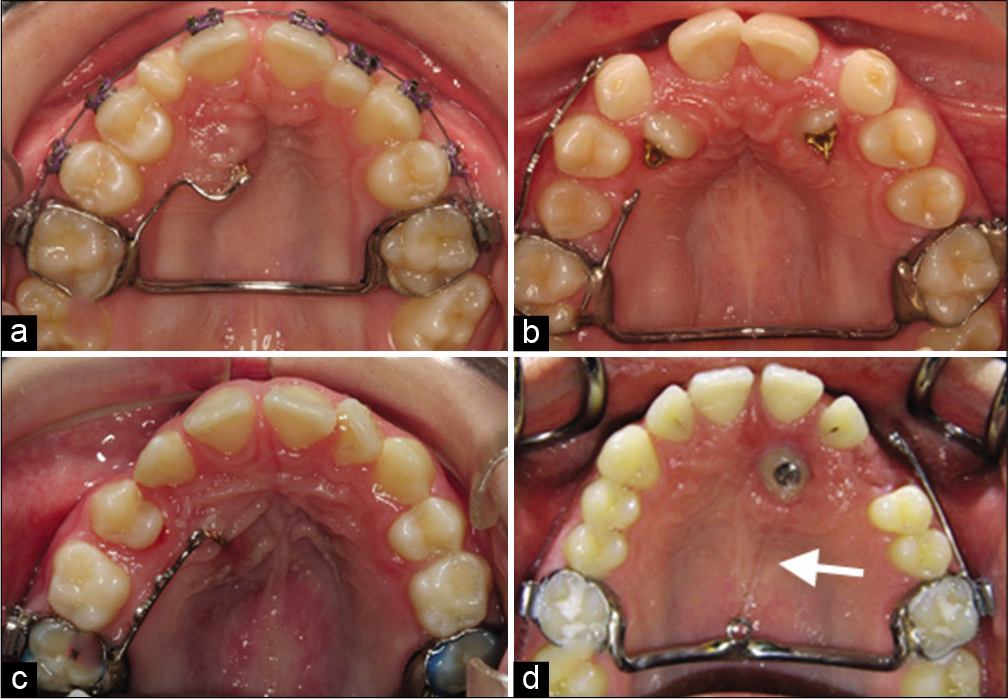
- Different ways to distance the canine from the incisor before one can start traction out in the alveolar crest. One-way is to start with a transpalatal arch for anchorage and solder a sectional arch with a loop for an elastic band (a) or place heavy wires soldered to the bands. These wires can be 0.8 or 0.9 mm and provided with eyelets. With this appliance, it is easy to change the direction of the traction with an elastic band (b and c). For the direction straight backwards, solder a loop directly on the transpalatal arch and add an elastic band, white arrow (d).
After distancing of the ectopically positioned maxillary canine, we believe that the resorption process is halted and the affected tooth is not susceptible to further damage. Now, comprehensive orthodontic treatment can start.
In 66 patients treated with fixed appliances, 32 had unilateral impacted maxillary canines. When these impacted canines first were distanced from the incisor roots before bonding, there was no increased risk for root resorptions.[54] In buccally impacted canines, the mechanics must be carefully selected to try to get the canine to erupt as much as possible in the center of the alveolar crest. This to avoid or at least to minimize gingival recession. A canine that has been exposed high up and drawn down to its normal position in the alveolar ridge may give a bad esthetic result.
Kokich[55] has presented three techniques for uncovering buccally impacted maxillary canines to get the best periodontal and esthetic result. These techniques are the excisional uncovering, apically positioned flap, and closed eruption techniques.
ADULT PATIENTS
Sometimes, you may encounter adult patients with impacted canines. It could be a patient where the general practitioner says that the canine has started to move or the primary canine is bad and must be removed and the position of the impacted canine makes it impossible to install an implant. In many cases, there is no dental follicle with the canine and the bone is very close to the tooth. This indicates a long treatment time to pull the canine down to the dental arch. Side effects such as intrusion of adjacent teeth are more common in adults than in young patients.
There are several case reports in the literature describing the successful treatment of impacted canines, but there is also a systematic review showing a success rate of 70% in patients between 20 and 47 years of age; those who failed were older patients.[56]
CONCLUSIONS
After the third molar, the maxillary permanent canine is the most frequently impacted tooth. The prevalence of impacted maxillary canines is 2–3%, and it is more common in females than in males.[6-9] Buccally displaced impacted canines are more common than palatally displaced in Asian populations, while the opposite is true in Caucasian populations.
In about 50% of impacted maxillary canines, resorption of the adjacent incisor roots. Resorption often starts at the age 11–12 years. Thus, it is essential to make an early diagnosis of impacted maxillary canines. At the age 9–11 years, the position of the maxillary canines must be settled. In most cases, this is done by clinical investigation including digital palpation buccally above the primary canine. In about 10% of children of this age, the clinical investigation must be supplemented with an intraoral radiographic investigation. When a suspicion of incisor root resorption arises with intraoral radiographs, these must be supplemented by a CBCT investigation.
When the general practitioner diagnoses ectopic eruption of the maxillary first permanent molar, normally at 6–7 years of age, they must consider this patient as being at risk of having impacted maxillary canines some years later.
There have been a number of studies on the extraction of primary canines in cases with palatally displaced canines with no suspicion to root resorption of the incisors. Most of these studies reported successful treatment that was even better in combination with cervical traction or a transpalatal arch or, if applicable, a rapid maxillary expansion. An improved eruption direction should be seen within a 12-month period or another orthodontic treatment must be taken into consideration.
When starting comprehensive orthodontic treatment, it is important to first distalize the canine away from the incisor root before pulling in out into the dental arch. Depending on the position of the canine, the optimal type of surgical exposure (closed or open) can be selected. The treatment of impacted canines has very limited impact on periodontal status and the long-term stability prognosis is good.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Malposition of single teeth In: Thilander B, Bjerklin K, Bondemark L, eds. Essential Orthodontics. Oxford: Wiley Blackwell; 2018. p. :104.
- [Google Scholar]
- The incidence of anomalous maxillary lateral incisors in relation to palatally displaced cuspids. Angle Orthod. 1981;51:24-9.
- [Google Scholar]
- Maxillary palatal canine impaction displacement in subjects with congenitally missing maxillary lateral incisors. Am J Orthod Dentofacial Orthop. 2011;140:81-6.
- [CrossRef] [PubMed] [Google Scholar]
- The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994;64:249-56.
- [Google Scholar]
- Familial trends in palatal canines, anomalous lateral incisors, and related phenomena. Eur J Orthod. 1990;12:135-9.
- [CrossRef] [PubMed] [Google Scholar]
- Resorption of incisors after ectopic eruption of maxillary canines: A CT study. Angle Orthod. 2000;70:415-23.
- [Google Scholar]
- A survey of 3, 874 routine full mouth radiographs. II. A study of impacted teeth. Oral Surg Oral Med Oral Pathol. 1961;14:1165-9.
- [CrossRef] [Google Scholar]
- The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81:12-20.
- [CrossRef] [PubMed] [Google Scholar]
- Resorption of maxillary lateral incisors caused by ectopic eruption of the canines. A clinical and radiographic analysis of predisposing factors. Am J Orthod Dentofacial Orthop. 1988;94:503-13.
- [CrossRef] [Google Scholar]
- Investigation of impacted permanent teeth except the third molar in Chinese patients through an X-ray study. J Oral Maxillofac Surg. 2010;68:762-7.
- [CrossRef] [PubMed] [Google Scholar]
- The etiology of maxillary canine impactions. Am J Orthod. 1983;84:125-32.
- [CrossRef] [Google Scholar]
- The position of maxillary canine impactions and the influenced factors to adjacent root resorption in the Korean population. Eur J Orthod. 2012;34:302-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical investigation of impacted maxillary canine. Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41:483-5.
- [Google Scholar]
- Prevalence and characteristics of impacted maxillary canines in southern Chinese children and adolescents. J Investig Clin Dent. 2014;5:38-44.
- [CrossRef] [PubMed] [Google Scholar]
- Morphology of the maxillary lateral incisor in cases of unilateral impaction of the maxillary canine. Br J Orthod. 1989;19:9-16.
- [CrossRef] [PubMed] [Google Scholar]
- Palatally displaced Canines: Diagnosis and interceptive treatment. J Orthod Craniofac Res. 2019;1:1-11.
- [Google Scholar]
- Ectopic eruption of maxillary first permanent molars and association with other tooth and developmental disturbances. Eur J Orthod. 1992;14:369-75.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary canine anomalies and tooth agenesis. Eur J Orthod. 2005;27:450-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dental anomalies as a microsymptom of palatal canine displacement. J Orofac Orthop. 2003;64:108-20.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal displacement of canine is genetic and related to congenital absence of teeth. J Dent Res. 1996;75:1742-6.
- [CrossRef] [PubMed] [Google Scholar]
- Association between ectopic eruption of maxillary canines and first molars. Eur J Orthod. 2005;27:186-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tooth anomalies associated with failure of eruption of first and second permanent molars. Am J Orthod Dentofacial Orthop. 2000;118:608-10.
- [CrossRef] [PubMed] [Google Scholar]
- Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10:285-95.
- [CrossRef] [Google Scholar]
- Two interceptive approaches to palatally displaced canines: A prospective longitudinal study. Angle Orthod. 2004;74:581-6.
- [Google Scholar]
- A randomized clinical study of two interceptive approaches to palatally displaced canines. Eur J Orthod. 2008;30:381-5.
- [CrossRef] [PubMed] [Google Scholar]
- Interceptive treatment of palatal impaction of maxillary canines with rapid maxillary expansion: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136:657-61.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of RME and headgear treatment on the eruption of palatally displaced canines: A randomized clinical study. Angle Orthod. 2011;81:370-4.
- [CrossRef] [PubMed] [Google Scholar]
- A RCT on treatment of palatally displaced canines with RME and/or a transpalatal arch. Eur J Orthod. 2011;33:601-7.
- [CrossRef] [PubMed] [Google Scholar]
- Extraction of the deciduous canine as an interceptive treatment in children with palatal displaced canines-Part I: Shall we extract the deciduous canine or not? Eur J Orthod. 2015;37:209-18.
- [CrossRef] [PubMed] [Google Scholar]
- The use of panoramic radiographs to decide when interceptive extraction is beneficial in children with palatally displaced canines based on a randomized clinical trial. Eur J Orthod. 2018;40:565-74.
- [CrossRef] [PubMed] [Google Scholar]
- The dental follicle in normally and ectopically erupting maxillary canines: A computed tomography study. Angle Orthod. 2001;71:333-42.
- [Google Scholar]
- Does the canine dental follicle cause resorption of permanent incisor roots? A computed tomographic study of erupting maxillary canines. Angle Orthod. 2002;72:95-104.
- [Google Scholar]
- Detection of lingual root resorptions in the intraoral radiographs. An experimental study. Swed Dent J. 2005;29:35-42.
- [Google Scholar]
- Guided eruption of palatally impacted canines through combined use of 3-dimensional computerized tomography scans and the easy cuspid device. World J Orthod. 2007;8:109-21.
- [Google Scholar]
- The role of digital volume tomography in the imaging of impacted teeth. World J Orthod. 2004;5:120-32.
- [Google Scholar]
- Incisor root resorptions due to ectopic maxillary canines imaged by computerized tomography: A comparative study in extracted teeth. Angle Orthod. 2000;70:276-83.
- [Google Scholar]
- Unerupted and displaced teeth in CT-scan. Int J Oral Maxillofac Surg. 1989;18:184-6.
- [CrossRef] [Google Scholar]
- Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2005;128:418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur J Orthod. 2011;33:93-102.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic examination of ectopically erupting maxillary canines. Am J Orthod Dentofacial Orthop. 1987;91:483-92.
- [CrossRef] [Google Scholar]
- Prevalence and risk factors of root resorption of adjacent teeth in maxillary canine impaction, among untreated children and adolescents. Eur J Orthod. 2019;41:447-53.
- [CrossRef] [PubMed] [Google Scholar]
- How a computerized tomography examination changed the treatment plans of 80 children with retained and ectopically positioned maxillary canines. Angle Orthod. 2006;76:43-51.
- [CrossRef] [Google Scholar]
- Root resorption-long-term outcome. Am J Orthod Dentofacial Orthop. 1997;112:119-23.
- [CrossRef] [Google Scholar]
- Long-term follow-up of severely resorbed maxillary incisors after resolution of an etiologically associated impacted canine. Am J Orthod Dentofacial Orthop. 2005;127:650-4.
- [CrossRef] [PubMed] [Google Scholar]
- Incisor root resorption due to ectopic maxillary canines: A long-term radiographic follow-up. Angle Orthod. 2008;78:778-85.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary incisor root resorption induced by ectopic canines. A follow-up study. 13 to 28 years posttreatment. Angle Orthod. 2011;81:800-6.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical exposure of impacted canines: Open or closed surgery. Semin Orthod. 2016;22:27-33.
- [CrossRef] [Google Scholar]
- Open versus closed surgical exposure of palatally impacted maxillary canines: Comparison of the different treatment outcomes-a systematic review. Eur J Orthod. 2018;40:11-22.
- [CrossRef] [PubMed] [Google Scholar]
- Closed vs. Open surgical exposure of palatally displaced canines: Surgery time, postoperative complications, and patients' perceptions: A multicenter, randomized, control trial. Eur J Orthod. 2018;40:626-35.
- [CrossRef] [PubMed] [Google Scholar]
- The contribution of periodontics to orthodontic therapy In: Dibart S, ed. Practical Advanced Periodontal Surgery. Ames, Iowa: Blackwell; 2007. p. :28-42.
- [Google Scholar]
- Forced-eruption time for palatally impacted canines treated with and without ostectomy-decortication technique. Angle Orthod. 2019;89:697-704.
- [CrossRef] [PubMed] [Google Scholar]
- Apical root resorption of incisors after orthodontic treatment of impacted maxillary canines: A radiographic study. Am J Orthod Dentofacial Orthop. 2012;141:427-35.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical and orthodontic management of impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2004;126:278-83.
- [CrossRef] [PubMed] [Google Scholar]
- Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2003;124:509-14.
- [CrossRef] [Google Scholar]






