Translate this page into:
Success rate of mini-implants based on side of insertion and type of jaw in adult patients undergoing orthodontic treatment – A systematic review and meta-analysis

*Corresponding author: Rutuja Sheshnarayan Devadkar, Department of Orthodontics and Dentofacial Orthopaedics, Sinhgad Dental College and Hospital, Pune, Maharashtra, India. devadkarrutuja@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Devadkar RS, Potnis S, Toshniwal N, Pharande S, Vinay V. Success rate of mini-implants based on side of insertion and type of jaw in adult patients undergoing orthodontic treatment – A systematic review and meta-analysis. APOS Trends Ortho 2022;12:295-305.
Abstract
Objectives:
To find out success rate of mini-implants based on side of insertion and type of jaw. The aim of orthodontic treatment is to maintain sufficient anchorage control to create appropriate force systems that provide the desired treatment effects. Implants have been used as skeletal anchorage devices for orthodontic purposes.
Material and Methods:
The following study is a systematic review of mini-screws as an intervention to evaluate the stability and different related clinical parameters to define the success rate (outcome) depending on the side of insertion (i.e., right side and left side) and type of jaw (i.e., maxilla and mandible following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
Results and Conclusion:
A total of 52 articles were extracted for qualitative synthesis among which 24 articles were reviewed for meta-analysis and the results showed that the maxilla is a better placement site for insertion of mini-implant (MI) than mandible with the odds ratio of 0.58, that is, the MI placement in the maxillary region is 58% more successful than mandibular region. The other parameter showed that the insertion of MI on the right side was more successful with the odds ratio of 0.50, that is, the insertion of MI on the right side of the jaw is 50% more successful than on the left side of the jaw.
Keywords
Success rate
Mini-implants
Orthodontics
INTRODUCTION
Anchorage control during tooth movement is one of the main factors for ensuring successful orthodontic treatment. Ottofy[1] defined anchorage as “the base against which orthodontic force or reaction of orthodontic force is applied.” Recently, Daskalogiannakis[2] defined anchorage as “resistance to unwanted tooth movement.” It can also be defined as the amount of allowed movement of the reactive unit. The aim of orthodontic treatment is to maintain sufficient anchorage control to create appropriate force systems that provide the desired treatment effects. Implants have been used as skeletal anchorage devices for orthodontic purposes.[3-6] Temporary anchorage devices (TADs),[7-9] including mini-plates, mini-implants (MI), and mini-screws, have been used for skeletal anchorage.[10-12] They can be fixed into the bone either biomechanically (osseointegration)[13] or mechanically (cortical stabilization).[12] Clinicians can better control anchorage using TADs in orthodontic treatment, thereby achieving more satisfactory treatment results than could be achieved with conventional mechanics.[10,14] Their clinical advantages consist of the versatility of the placement site, easy insertion and removal, minimal anatomic limitations, minor surgery, increased patient comfort, immediate loading, possible use in young patients, and low costs. The selection of inter-radicular insertion sites is determined by three factors: Biomechanics of the chosen appliance, patient’s anatomy, and dimensions of MI. MI as a source of anchorage in orthodontic procedures is excellent for adjunctive tooth movements such as en masse anterior retraction, molar distalization or mesialization, molar intrusion or extrusion; correction of canted or tilted occlusal plane; and vertical control.[15] The purpose of the following research was to conduct a systematic review in a view to summarize and update the actual knowledge about MIs in clinical practice, in particular about their stability and reliability.
MATERIAL AND METHODS
Study design
The following study is a systematic review of mini-screws as an intervention to evaluate the stability and different related clinical parameters to define the success rate (outcome) depending on the side of insertion (i.e., right side and left side) and type of jaw (i.e., maxilla and mandible). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The systematic review and meta-analysis had been registered in PROSPERO Cochrane database on July 5, 2020.
ID no. CRD42020188549.
Population
Adult patients undergoing orthodontic treatment.
Intervention
MIs.
Comparison
Left/right side of arch, MIs in maxilla and mandible.
Primary outcome
Success rate based on MI insertion side and jaw type.
Secondary outcome
Success rate is based on length, diameter, site of insertion, force of insertion, and various factors affecting the success of MIs.
Study design
This was a clinical study.
Focused question
To evaluate the success rate of MIs of the insertion side (i.e., right side and left side) and jaw type (i.e., maxilla or mandible) in adult patients undergoing orthodontic treatment.
Study inclusion criteria
It was as follows:
Studies that analyzed the success of MIs (inter-radicular implants) for orthodontic anchorage
Only human clinical studies with a minimum sample size of 10 MIs (inter-radicular implants)
Only studies that defined success rate
Only studies that define the duration of application of the force
Studies that measured implant success after 3 months
Studies that measured success either at a predetermined treatment time or after orthodontic anchorage objective
All the randomized control trials, controlled trials, retrospective studies, and clinical studies
Articles in the English language
Articles published between the periods of January 1, 2005, and November 30, 2020.
Exclusion criteria
Case reports, reviews, expert opinions, animal studies, laboratory, and in vitro studies are excluded from the study
Only abstracts to be excluded from the study
Studies in a language other than English
Studies having participants other than adults will be excluded from the study.
Search strategy
The search process was performed independently by two examiners under the guidance of a librarian. The databases were searched for articles published until November 30, 2020, in English. The electronic and manual database was searched for the study. Journals that were scanned and searched were the American Journal of Orthodontics and Dentofacial Orthopaedics, Angle’s Orthodontist, and Seminars in Orthodontics. Electronic databases such as Google Scholar and PubMed were screened. Appropriate changes in the keywords were done to follow the syntax rules of each database. The main terms used were “MI AND Success AND Orthodontics” and “Mini-screws AND Success AND Orthodontics.”
The authors in the study played a crucial role in the concept and design of the study, data extraction, searching the electronic and manual databases, statistics of the study, and reviewing and cross-examining the articles included in the study. The two examiners assessed the titles and the abstracts of all studies displayed. If the abstract lacked information to allow decision-making about selection, the full article was obtained and evaluated before decision-making. Several articles appeared in more than 1 database but they were considered once. Any doubt about inclusion or exclusion was solved with a discussion. Screening the reference lists of the selected articles complemented the search. The selected articles were then carefully read for the quality assessment and control of bias and data extraction.
Screening articles
Free full-text articles were screened. Study selection was done on basis of the inclusion and exclusion criteria. Data extraction was done by two reviewers and recorded in separate Excel sheets. Any discrepancies in the study selection were resolved by the third reviewer. The interexaminer agreement was measured through Cohen kappa test, which concluded to be almost perfect. Risk of bias was conducted with Cochrane tool of collaboration. Meta-analysis was done using RevMan software version 5.3. (The Nordic Cochrane Centre, Copenhagen, Denmark).
Data extraction
Two examiners extracted and tabulated the following issues from the selected articles:
Author, year of publication, journal, geographic location, and study design
Number of patients
Number of MIs
Total success rate
Mean age and standard deviation
Length of the MIs
Success rate related to the length of the MIs
Number of MIs on insertion side, that is, right and left side
Number of MIs placed in the mandible
Number of MIs placed in the maxilla
Success rate in the mandible
Success rate in the maxilla
Odds ratio
Conclusion.
RESULTS
Study selection
The extensive search across various databases retrieved 4850 references. After the removal of duplicates, 3915 titles/ abstracts were screened and 3863 were excluded because they did not fit the selection criteria. Out of the lot, with the application of our stringent (inclusion/exclusion) criteria, 52 studies were finally included for qualitative assessment. The included articles were further subjected to intricate evaluation and 24 studies that reported data that could be analyzed were included for quantitative assessment (meta-analysis).
Characteristics of studies
The included studies were published between 2005 and 2019. The studies were belonging to clinical trials,[16-31] retrospective studies,[30-36] and randomized controlled trials (RCTs).[3-8,10-12,14,15,37-46] The studies included a cumulative number of 3687 participants with an age interval from approximately 12 to 38 years. Few of the studies[19-24,26,27] did not mention the age group. The studies were carried all across the globe belonging to Japan,[17,22,25-27] Korea,[16,18,23,32] Turkey,[45,47] Egypt,[46,48] European region,[24,28,29,30,35] Asia,[19,20,31,34,37] and Poland.[33,49]
Patients
Participants treated with MIs
Intervention
MIs.
Comparison (Control)
Left/right side of arch, MIs in maxilla and mandible.
Outcome (success rate out of total events)
Primary outcomes were stated as success rate based on the insertion side, that is, right side or left side and based on the jaw type, that is, maxilla or mandible.
Study design
This study was clinical trials and RCTs.
The outcome of the qualitative synthesis was as follows:
The length of MIs varied from 5 to 17 mm with an average of 8 mm with a most common used diameter of 1.3 mm
The position of insertion for MIs was between second premolars and first molars in both the maxilla and mandible
Two studies[40,41] reported that MIs are the primary results with the use of MIs which were anchorage and molar distalization[42,45-47,49] in orthodontic treatment
The force of insertion for MIs was averaged with a torque of 4–10 Ncm. Bone density and quality as an important contributing factors for the success of MI
The operative protocol and clinician skills which result in conservative flap incision and controlled inflammation are responsible for better success rate of MI, especially in mandible was reported by three studies[17,45,46]
Four studies[40,43,49,45] said factors which contributed to failure of MI are the placement site, the loading time and proximity of the MI to the root and three studies advocated for bone density and length. The factors such as root proximity and surface characteristics of MI were important for the success of the anchorage device
Another significant factor contributes to the success in patient compliance which is dependent on the pain, comfort, and inflammation after the placement partially where the orthodontist skills are responsible
Wang and Liou, Park et al., and Son et al. stated that irrespective of pre-drilled and self-drilled or the surface texture of being machine or acid etched the success rate is not dependent on it
Majority of the studies[17-21,25,26,29,31,35-37] considered MI as an effective TAD in orthodontic patients due to the gradual osseointegration and better anchorage effects which can be long lasting
For better results long-term hygiene care was necessary according to Wu et al., MIs were considered an alternative to surgery[20] and easy to perform for clinicians[34]
Sex, age, and ANB angle are also factors contributing to the success of MI according to some studies[17,23]
Immediate loading[28,30] can also influence the success of MI along with the insertion site[36] of the implant.
For backing the clinical significance of the insertion site and arch, we conducted a quantitative synthesis accompanying the qualitative assessment.
For supporting the qualitative evidence, we further carried out the quantitative analysis by meta-analysis.
Synthesis of results (Meta-analysis)
The meta-analysis was conducted on 24 studies that reported the outcome that could be analyzed under the two consistent parameters: Insertion side and type of jaw. A blobbogram of respective outcomes was plotted to compare the MI based on the insertion site and arch. The meta-analysis was carried out in Review Manager software (RevMan, version 5.3; Nordic Cochrane Centre [Cochrane Collaboration], Copenhagen, Denmark; 2014).
Insertion side
A total of nine studies were included in the meta-analysis for this outcome parameter. A pooled odds ratio of 0.58 (CI: 0.33, 1.00) on application of random effect model was observed with the heterogeneity of I2 = 82% (significant), thus indicating that the success rate was higher on the right side for insertion of MI as compared to its contralateral side [Figure 1].

- Forest plot of comparison: 1 Success rate, outcome: 1.1 Insertion side.
Arch/jaw
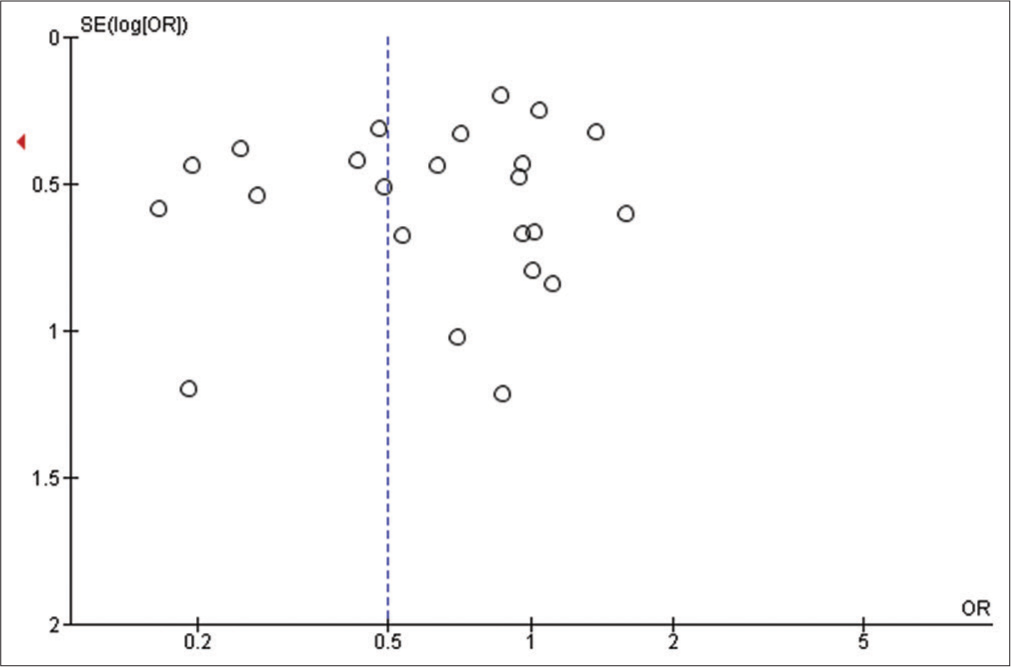
A total of 24 studies were included in the meta-analysis for this outcome parameter. A pooled odds ratio of 0.50 (CI: 0.30, 0.84) on application of random effect model was observed with the heterogeneity of I2 = 88% (significant), indicating that when MI was placed in the maxilla which had higher odds of success rate than the mandible [Figure 2].

- Funnel plot of comparison: 1 Success rate, outcome: 1.2 Type of jaw.
Publication bias
Publication bias was assessed for these outcomes to detect funnel plot asymmetry. The funnel plot indicated that the majority of the studies had less publication bias and higher quality of reporting results [Figures 3 and 4].
- Funnel plot of comparison: 1 Success rate, outcome: 1.2 Insertion side.

- Funnel plot of comparison: 1 Success rate, outcome: 1.2 Type of jaw.
Risk of bias
The risk of bias was assessed by the two independent reviews for RCTs included in the review and discrepancies were resolved by discussion and appropriate consultation with a third reviewer. The domains for risk assessment were graded as high, uncertain or low risk, based on selection bias (random sequence generation and allocation concealment), performance bias (blinding), detection bias (assessor blinding), attrition bias (incomplete outcome data), and reporting bias (selective reporting). Thus, the overall risk for individual studies was assessed as low, moderate, or high risk based on the domains and criteria. The study was assessed to have a low overall risk only if all domains were found to have low risk and high overall risk if one or more of the six domains were found to be at high risk. A moderate risk assessment was provided to the studies when one or more domains were found to be uncertain, with none at high risk [Figures 5 and 6].

- Risk of bias summary: Review authors’ judgments about each risk of bias item for each included study.

- Risk of bias summary of the articles included in the study.
DISCUSSION
As of November 30, 2020, 24 studies were selected by computerized and manual searches to provide data on the success rate of MIs.
The goal of any orthodontic treatment is to achieve desired tooth movement with a minimum number of undesirable side effects. Anchorage is one of the important factors for the treatment of dental and skeletal malocclusion with fixed appliances and is a critical factor in determining the success of orthodontic treatment. The difficulty in establishing a stable anchorage system has always been a great concern to the orthodontist because the success of orthodontic treatment generally relies on the anchorage protocol planned for that particular case.
In general, in the studies, where the distinction of success rate according to the sex of patients has been made, no significant differences are noted. Manni et al.[38] found a success rate higher in male patients (88.1%) than females (76.4%) (P < 0.05). It could be registered as a general trend of direct proportionality between success rate and age. In the study by Motoyoshi et al., immediate loading of MIs showed success rates significantly (P < 0.05) higher in adults than adolescents.[22] This finding probably indicates that the bone density of adolescents is not sufficient to support immediate loading with orthodontic forces. The screws with a diameter of 1.2 mm or more are used worldwide with a success rate of above 70%. The MIs with a smaller diameter are easier to be placed between the roots, but a small reduction in this dimension decreases significantly the torsional strength and, therefore, increases the risk of fracture of the implant. It is advisable to avoid implants smaller than 1.3 mm in diameter, especially when placed in the thick cortical bone in the lower jaw. There were also reported fractures in two studies with implants of this size.[42] Another significant factor is the length of a MI, determined based on several characteristics such as the depth and quality of bone, the angle of the screw, the transmucosal thickness, and adjacent vital structures. Short screws in regions with thick soft tissues, such as the mucosa of the palate, could easily become unstable. In these sites it was recommended to use longer screws. The minimum depth of placement of a MI is at least 5–6 mm, but it is recommended a deeper insertion when the bone quality is low. It should be emphasized that by increasing the diameter and length of the screw, the risk of damaging the roots during placement increases. The mini-screws with a diameter of 1.2 mm and a length of at least 8 mm have sufficient stability with minimal risk of radicular damage.[43] The flapless method is less expensive in terms of time but can reduce the chances of accurate placement of the mini-screw. An advantage of the flapless method is the better comfort for the patients. For both flap and flapless protocols, conflicting success rates have been published. Only Herman et al. reported a significantly higher success rate (100%) for mini-screws (n = 10) placed with flap surgery.[50]
Care must be taken to place the MI away from the root apices and the inferior alveolar nerves. The improper placement could lead to tooth damage or permanent nerve injury and complications such as fracture of the MI on insertion, iatrogenic damage to teeth causing loss and bony sequestra around the area of MI placement. Hence, a thorough clinical and radiographic three-dimensional assessment of the teeth adjacent to the site for MI placement is necessary. Due to the wide variation in root morphology, post-operative radiography must be used to screen for any evidence of impingement of the root or nerve.
Factors related to the maintenance of the implants, including the control of peri-implantitis, antibiotic prophylaxis, rinsing with chlorhexidine, and oral hygiene instructions, are also important; even if the possible relationship between the stability of the implants and the use of antibiotics or chlorhexidine has not been analyzed in any study. Park et al. related the control of peri-implantitis with the success of orthodontic treatment, but they did not find any correlation between oral hygiene measures and the primary outcomes.[25]
A total of nine studies were included in the meta-analysis for the success based on insertion side parameter and 24 studies for the success based on type of jaw parameter.
The stability of mini-screws immediately following their placement (primary stability) and during orthodontic treatment is important for clinicians in terms of achieving their desired treatment results. The primary factors for stability are the quality and quantity of the bone,[15,29] as well as the thickness, type, and health of the soft tissue.[9]
Clinical evaluation revealed successful dental movements when implants remained stable during the orthodontic therapy.
CONCLUSION
A total of 52 articles were extracted for qualitative synthesis among which 24 articles were reviewed for meta-analysis and the results showed that the maxilla is a better placement site for insertion of MI than mandible with the odds ratio of 0.58. The MI placement in the maxillary region is 58% more successful than mandibular region.
The other parameter showed that the insertion of MI on the right side was more successful with the odds ratio of 0.50. The insertion of MI on the right side of the jaw is 50% more successful than on the left side of the jaw.
It can be concluded that MIs represent effective TADs.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
PRISMA FLOW DIAGRAM

*Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71
PRISMA CHECKLIST
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71
| Section and Topic | Item # | Checklist item | Location where item is reported |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review. | Pg 1 |
| ABSTRACT | |||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist. | Pg 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge. | Pg no: 1 and Pg no: 3 |
| Objectives | 4 | Provide an explicit statement of the objective (s) or question (s) the review addresses. | Pg no: 1 and Pg no: 3 |
| METHODS | |||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | Pg no: 3 |
| Information sources | 6 | Specify all databases, registers, websites, organizations, reference lists, and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted. | Pg no: 3 and 4 |
| Search strategy | 7 | Present the full search strategies for all databases, registers, and websites, including any filters and limits used. | Pg no: 3 and 4 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process. | Pg no: 3 and 4 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process. | Pg no: 4 and pg no: 5 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, and analyses), and if not, the methods used to decide which results to collect. | Pg no: 5,6 and 7 |
| 10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information. | Pg no: 5,6 and 7 | |
| Study risk of bias assessment | 11 | Specify the methods used to assess the risk of bias in the included studies, including details of the tool (s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | Pg no: 6 |
| Effect measures | 12 | Specify for each outcome the effect measure (s) (e.g., risk ratio and mean difference) used in the synthesis or presentation of results. | Pg no: 5 and 6 |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)). | Pg no: 5 and 6 |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions. | Pg no: 5 and 6 | |
| 13c | Describe any methods used to tabulate or visually display the results of individual studies and syntheses. | Pg no: 5 and 6 | |
| 13d | Describe any methods used to synthesize results and provide a rationale for the choice (s). If meta-analysis was performed, describe the model (s), method (s) to identify the presence and extent of statistical heterogeneity, and software package (s) used. | Pg no: 5 and 6 | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis and meta-regression). | Pg no: 5 and 6 | |
| 13f | Describe any sensitivity analyses conducted to assess robustness of the synthesized results. | Pg no: 5 and 6 | |
| Reporting bias assessment | 14 | Describe any methods used to assess the risk of bias due to missing results in a synthesis (arising from reporting biases). | Pg no: 6 |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | Pg no: 6 |
| RESULTS | |||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | Pg no: 9 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded. | Pg no: 3,4,5 and 6 | |
| Study characteristics | 17 | Cite each included study and present its characteristics. | Pg no: 5 and 6 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each included study. | Pg no: 6 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) Summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | Pg no: 2,3,4,5 and 6 |
| Results of syntheses | 20a | For each synthesis, briefly summarize the characteristics and risk of bias among contributing studies. | Pg no: 5 and 6 |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/ credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect. | Pg no: 5 and 6 | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results. | Pg no: 5 and 6 | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results. | Pg no: 5 and 6 | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed. | Pg no: 6 |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed. | Pg no: 5 and 6 |
| DISCUSSION | |||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence. | Pg no: 6 and 7 |
| 23b | Discuss any limitations of the evidence included in the review. | Pg no: 6 and 7 | |
| 23c | Discuss any limitations of the review processes used. | Pg no: 6 and 7 | |
| 23d | Discuss implications of the results for practice, policy, and future research. | Pg no: 6 and 7 | |
| OTHER INFORMATION | |||
| Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered. | Pg no: 2 |
| 24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared. | Pg no: 2 | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol. | Pg no: 2 | |
| Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review. | Pg no: 7 |
| Competing interests | 26 | Declare any competing interests of review authors. | Pg no: 7 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review. | Pg no: 2,3,4 and 5 |
References
- Glossary of Orthodontic Terms United States, Leipzig: Quintessence Publishing Co.; 2000.
- [Google Scholar]
- Handbook of Orthodontics for the Student and General Practitioner United States, Chicago: Year Book Medical Publishers Inc.; 1973.
- [Google Scholar]
- A study of orthodontic anchorage possibilities in basal bone. Am J Orthod. 1945;31:406-17.
- [CrossRef] [Google Scholar]
- En masse space closure In: Burstone CJ, ed. Modern Edgewise Mechanics and the Segmented Arch Technique. Glendore: Ormco Corp; 1995. p. :50-60.
- [Google Scholar]
- Temporary anchorage devices in orthodontics: Mini implants. Semin Orthod. 2005;11:32-9.
- [CrossRef] [Google Scholar]
- Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005;20:769-76.
- [Google Scholar]
- Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86:95-111.
- [CrossRef] [Google Scholar]
- The Orthosystem-a new implant system for orthodontic anchorage in the palate. J Orofac Orthop. 1996;57:142-53.
- [CrossRef] [PubMed] [Google Scholar]
- Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007;131:S68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Miniscrews as orthodontic anchorage: A preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201-9.
- [Google Scholar]
- Biomechanical and histomorphometric analyses of monocortical screws at placement and 6 weeks postinsertion. J Oral Implant. 2006;32:110-6.
- [CrossRef] [PubMed] [Google Scholar]
- Efficiency of a skeletonized distal jet appliance supported by miniscrew anchorage for noncompliance maxillary molar distalization. Am J Orthod Dentofac Orthop. 2009;136:578-86.
- [CrossRef] [PubMed] [Google Scholar]
- Survival analysis of orthodontic mini-implants. Am J Orthod Dentofac Orthop. 2010;137:194-9.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate loading of orthodontic mini-implants: A histomorphometric evaluation of tissue reaction. Eur J Orthod. 2009;31:21-9.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101-6.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between vertical skeletal pattern and success rate of orthodontic mini-implants. Am J Orthod Dentofac Orthop. 2010;138:51-7.
- [CrossRef] [PubMed] [Google Scholar]
- Tapered orthodontic miniscrews induce bone-screw cohesion following immediate loading. Eur J Orthod. 2006;28:541-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implants. Int J Oral Maxillofac Implants. 2007;22:779-84.
- [Google Scholar]
- The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int J Oral Maxillofac Surg. 2009;38:13-8.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary sinus perforation by orthodontic anchor screws. J Oral Sci. 2010;57:95-100.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofac Orthop. 2006;130:18-25.
- [CrossRef] [PubMed] [Google Scholar]
- Miniscrews for upper incisor intrusion. Eur J Orthod. 2009;31:412-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of the primary stability of self-drilling and self-tapping orthodontic miniscrews. Am J Orthod Dentofac Orthop. 2014;145:480-5.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical study of temporary anchorage devices for orthodontic treatment-stability of micro/mini-screws and mini-plates: Experience with 455 cases. Bull Tokyo Dent Coll. 2010;51:151-63.
- [CrossRef] [PubMed] [Google Scholar]
- Mini-implant anchorage for en-masse retraction of maxillary anterior teeth: A clinical cephalometric study. Am J Orthod Dentofac Ortho. 2008;134:803-10.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanics of incisor retraction with mini-implant anchorage. J Orthod. 2014;41:S15-23.
- [CrossRef] [PubMed] [Google Scholar]
- Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofac Orthop. 2009;136:29-36.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am J Orthod Dentofac Orthop. 2007;131:9-15.
- [CrossRef] [PubMed] [Google Scholar]
- Accurate pre-surgical determination for self-drilling miniscrew implant placement using surgical guides and cone-beam computed tomography. Eur J Orthod. 2010;32:735-40.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between miniscrew stability and bone mineral density in orthodontic patients. Am J Orthod Dentofac Orthop. 2009;136:243-50.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the loading behavior of self-drilling and predrilled miniscrews throughout orthodontic loading. Am J Orthod Dentofac Orthop. 2008;133:38-43.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with the stability of mini-implants for orthodontic anchorage: A study of 414 samples in Taiwan. J Oral Maxillofac Surg. 2009;67:1595-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of optimal length and insertion torque for miniscrews. Am J Orthod Dentofac Orthop. 2013;144:251-9.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eur J Orthod. 2011;33:388-95.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical and histological evaluation of titainium mini-implants as anchors for orthodontic intrusion in the beagle dog. Am J Orthod Dentofacial Orthop. 2001;119:489-97.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of low-intensity laser therapy on the stability of orthodontic mini-implants: A randomised controlled clinical trial. J Orthod. 2018;45:149-56.
- [CrossRef] [PubMed] [Google Scholar]
- Success rate and risk factors associated with mini-implants reinstalled in the maxilla. Angle Orthod. 2008;78:895-901.
- [CrossRef] [PubMed] [Google Scholar]
- Patient's perception on mini-screws used for molar distalization. Rev Odonto Ciência. 2010;25:266-70.
- [Google Scholar]
- Influence of surface characteristics on survival rates of mini-implants. Angle Orthod. 2008;78:107-13.
- [CrossRef] [PubMed] [Google Scholar]
- DES design: Theoretical advantages and disadvantages of stent strut materials, design, thickness, and surface characteristics. J Interv Cardiol. 2009;22:S3-17.
- [CrossRef] [Google Scholar]
- Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate. Head Face Med. 2017;13:14.
- [CrossRef] [PubMed] [Google Scholar]
- Cone-beam computed tomography evaluation of mini-implants after placement: Is root proximity a major risk factor for failure? Am J Orthod Dentofac Orthop. 2010;138:264-76.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome of mini-screws used as orthodontic anchorage. Clin Implant Dent Relat Res. 2008;10:174-80.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of 2 distalization systems supported by intraosseous screws. Am J Orthod Dentofacial Orthop. 2007;131:161.e1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anchorage value of surgical titanium screws in orthodontic tooth movement. Int J Oral Maxillofac Surg. 2007;36:588-92.
- [CrossRef] [PubMed] [Google Scholar]
- Mini-implant anchorage for maxillary canine retraction: A pilot study. Am J Orthod Dentofac Orthop. 2006;130:228-35.
- [CrossRef] [PubMed] [Google Scholar]






