Translate this page into:
The past and present research at the University of Sydney’s Discipline of Orthodontics

*Corresponding author: M. Ali Darendeliler, Department of Orthodontics and Paediatric Dentistry, The University of Sydney School of Dentistry, Sydney Dental Hospital, Sydney Local Health District, New South Wales, Australia. ali.darendeliler@sydney.edu.au
-
Received: ,
Accepted: ,
How to cite this article: Gandedkar NH, Dalci O, Darendeliler MA. The past and present research at the University of Sydney’s Discipline of Orthodontics. APOS Trends Orthod 2021;11(2):90-9.
Abstract
The University of Sydney’s Discipline of Orthodontics has been actively pursuing research in the areas of root resorption, sleep apnea, magnets in orthodontics, implants, acceleration of orthodontic tooth movement (OTM), and remote monitoring (RM). Our research has shed light on many specific factors that influence orthodontically induced inflammatory root resorption (OIIRR). We also explored the effects of some of the most discussed acceleration interventions on OTM and OIIRR, such as vibration, micro-osteoperforations, piezocision, low-level laser therapy, light emitting diode, light amplification by stimulated emission of radiation, and pharmacological substances. Further, we have researched into maximizing orthopedic treatment outcomes of maxillary deficient children with use of intraoral force application with utilization of miniscrew-assisted rapid palatal expander. We are currently trialing use of RM to facilitate orthodontic services in the public dental clinics.
Keywords
University of Sydney
Root resorption
Sleep apnea
Magnets in orthodontics
Acceleration of orthodontic tooth movement
MARPE
Class III elastics
Remote orthodontic monitoring
INTRODUCTION
The University of Sydney’s Discipline of Orthodontics has been actively pursuing research in the area of orthodontic root resorption, sleep apnea, magnets in orthodontics, mini-implants, acceleration of orthodontic tooth movement (OTM), teleorthodontics, and remote monitoring (RM). Furthermore we have been investigating efficacy of various treatment modalities in the management of skeletal malocclusions. In this paper, the authors have divided the main areas of research, carried out over three decades, in four main domains, and they are; [Figure 1].
Orthodontically induced inflammatory root resorption (OIIRR) and OTM
Biomaterial applications in orthodontics
Maximizing orthopedic treatment outcomes
RM in orthodontics
OTM AND BIOLOGICAL RESPONSES
Influence of orthodontic forces on the dentoalveolar apparatus [Figure 2] and acceleration of OTM has played a key interest to OTM researchers to counter one of orthodontic treatment’s major deterrents, the treatment duration. Several methods have been proposed to accelerate OTM encompassing biological, mechanical, and surgical interventions aimed or targeted at enhancing the biological processes (rate of alveolar bone and PDL remodeling) that are responsible for OTM. Some of the most common interventions are; vibration, micro-osteoperforations (MOPs), piezocision, low-level laser therapy (LLLT), light emitting diode (LED), pharmacological substances, and so on, which intend to enhance cellular metabolism and proliferation which are suggested to have the potential to accelerate OTM. Our department is actively testing the modalities of accelerated OTM to determine if there is any real benefit to using the aforementioned interventions in routine orthodontic practice.
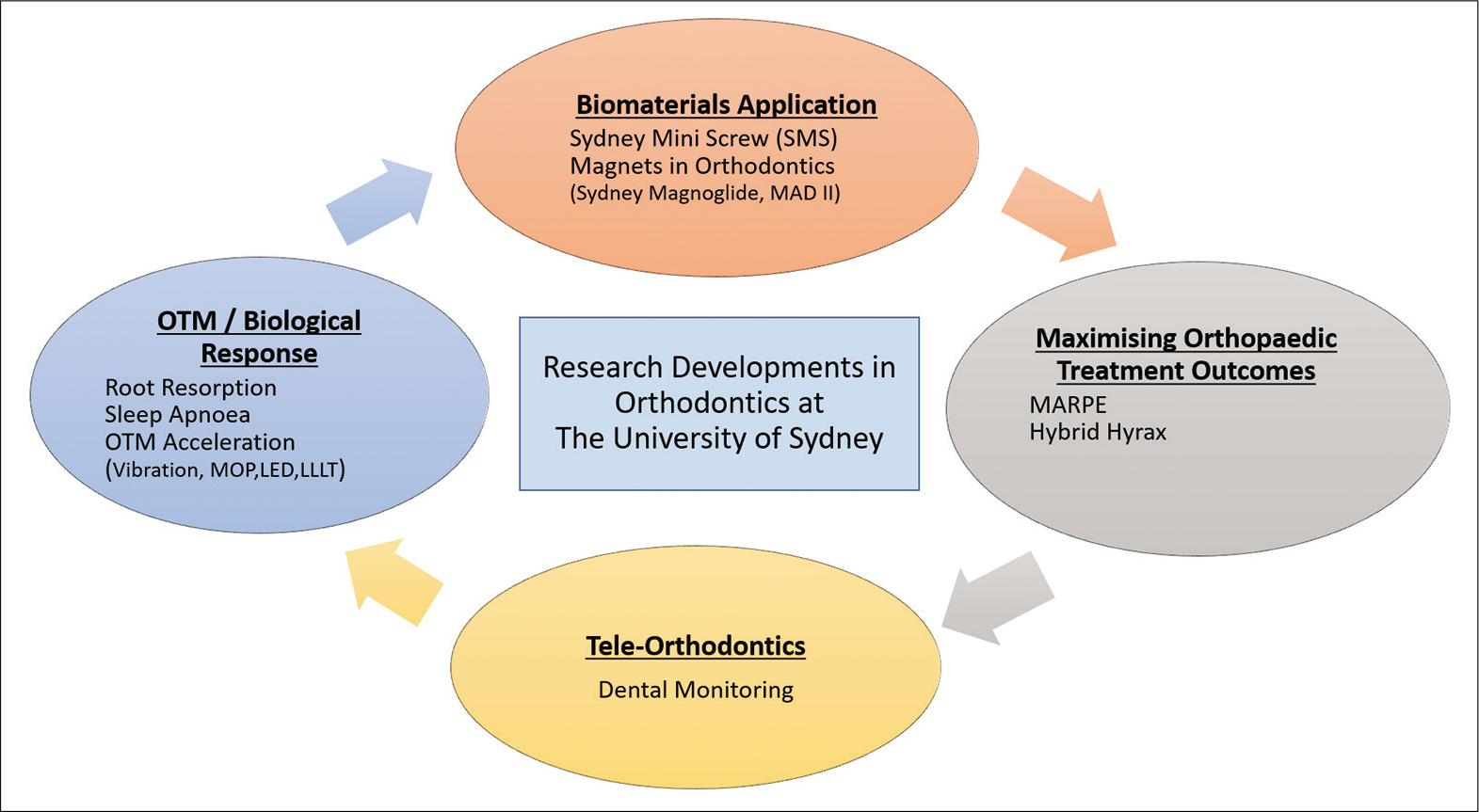
- Flowchart describing the research developments in orthodontics at the University of Sydney’s Department of Orthodontics.
![A three-dimensional finite element model aimed to explore the biomechanical response of the periodontal ligament [first principal (tensile) and third principal (compressive) stresses] and maxillary alveolar bone (von Mises stress) under purported “heavy” (300 g) and “light” (50 g) continuous orthodontic forces. The study highlights that stress within the periodontium can occur with both heavy and light orthodontic forces.](/content/9/2021/11/2/img/APOS-11-090-g002.png)
- A three-dimensional finite element model aimed to explore the biomechanical response of the periodontal ligament [first principal (tensile) and third principal (compressive) stresses] and maxillary alveolar bone (von Mises stress) under purported “heavy” (300 g) and “light” (50 g) continuous orthodontic forces. The study highlights that stress within the periodontium can occur with both heavy and light orthodontic forces.
Some of our studies on acceleration of OTM are as follows; Mistry et al. performed a split-mouth randomized controlled trial (RCT) to investigate the effect of LLLT on the amount of maxillary canine distalization when applied every 4 weeks over 12 weeks, to resemble a more realistic “real-life” application frequency to go hand in hand with normal orthodontic adjustments. The gallium aluminum arsenide diode laser with a mean wavelength of 808 ± 5 nm of 0.20 W and irradiance of 1.97 W/cm2 in continuous wave mode were used in this study in comparison to sham laser on the contralateral side (Thor Photomedicine, Buckinghamshire, United Kingdom). There was no difference in OTM between LLLT and control group, and also, no significant differences were noted in the rate of OTM with applying LLLT every 4 weeks at 13 J/session.[1] This was followed by our split-mouth RCT using the OrthoPulse device (Biolux Research Ltd., Vancouver, British Columbia, Canada) which is a LED-mediated photobiomodulation (PBM) device with 850 nm wavelength, 60 mW/cm2 power. The device was used at home for 5 min/d by patients. One side of the OrthoPulse device was covered by thick tape to block the light on the control side. The study concluded that daily 5 min application of LED PBM did not result in clinically meaningful differences during extraction space closure compared with no LED over the 12-week study period.
OIIRR
OIIRR is an untoward shortcoming of OTM. In general, OIIRR is a pathological progression that is associated with the local insults of the periodontal ligament (PDL) and resorption of cementum and dentine which occurs in association with the removal of hyalinized tissue during OTM.[2-5] The University of Sydney’s Orthodontic Department has carried out some of the pioneering work (published in 27 parts, so far) on OIIRR; from the initial years of OIIRR research that focussed on establishing mineral composition of human premolar cementum after the application of orthodontic forces, and effects of different types of OTM methods to modern-day acceleration of OTM applications such as LLLT, MOP, LED, and piezocision on OIIRR.[5-32] Few of our au fait advances with respect to OIIRR research are reckoned below;
The extent of root resorption and the amount of tooth movement between continuous orthodontic force (150 g for 15 weeks) and intermittent orthodontic force (150 g for 28 days on, 7 days off) was studied using microcomputed tomography (micro-CT) scan of 50 maxillary first premolars from 25 orthodontic patients (14 boys and 11 girls; age range, 13.08–17.58 years; mean, 14.77 years). Intermittent force significantly reduced the amount of root resorption compared with continuous force.[32]
A micro-CT study was performed to assess the influence of piezocision, a flapless corticotomy procedure to accelerate OTM, on root resorption when 150 g buccal tipping forces were applied to maxillary first premolars for a 4-week period. The study concluded that in the first 4 weeks following force application and piezocision, there was an increase in OIIRR and more importantly highlighted the risk of iatrogenic damage when piezocision is applied close to the roots[27] [Figure 3].
Following on from the previous study, another micro-CT study evaluated the effects of MOP on orthodontic root resorption using the Propel appliance (Propel Orthodontics, San Jose, Calif) with 5 mm MOPs on the mesial and distal aspects in the midroot region of maxillary first premolars. This trial showed that MOPs also resulted in greater orthodontic root resorption following a 28-day period.[14] Both studies suggested these results to be investigated on patients undergoing full course of orthodontic treatment.
A 2-arm-parallel split-mouth RCT studied the effect of LLLT using a continuous beam 660 nm, 75 mW aluminum-gallium-indium-phosphorus laser on the repair of OIIRR. The study concluded that there were no significant differences between LLLT and sham control groups in OIIRR repair.[22]
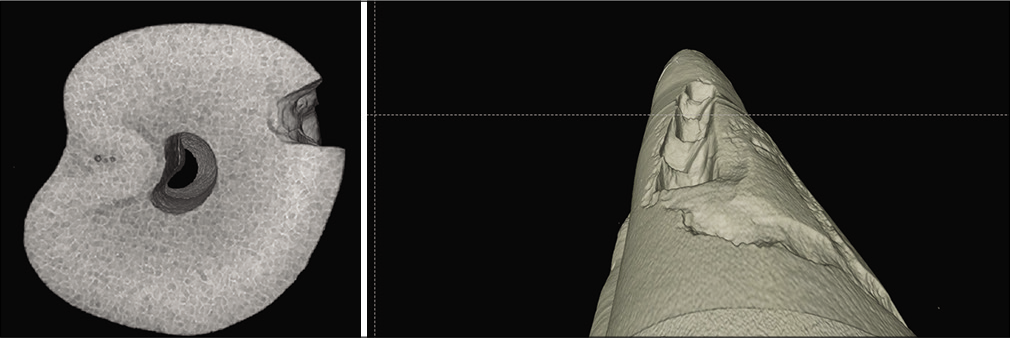
- Images showing micro-CT piezocision study showing risk of iatrogenic damage when piezocision is applied close to the roots.
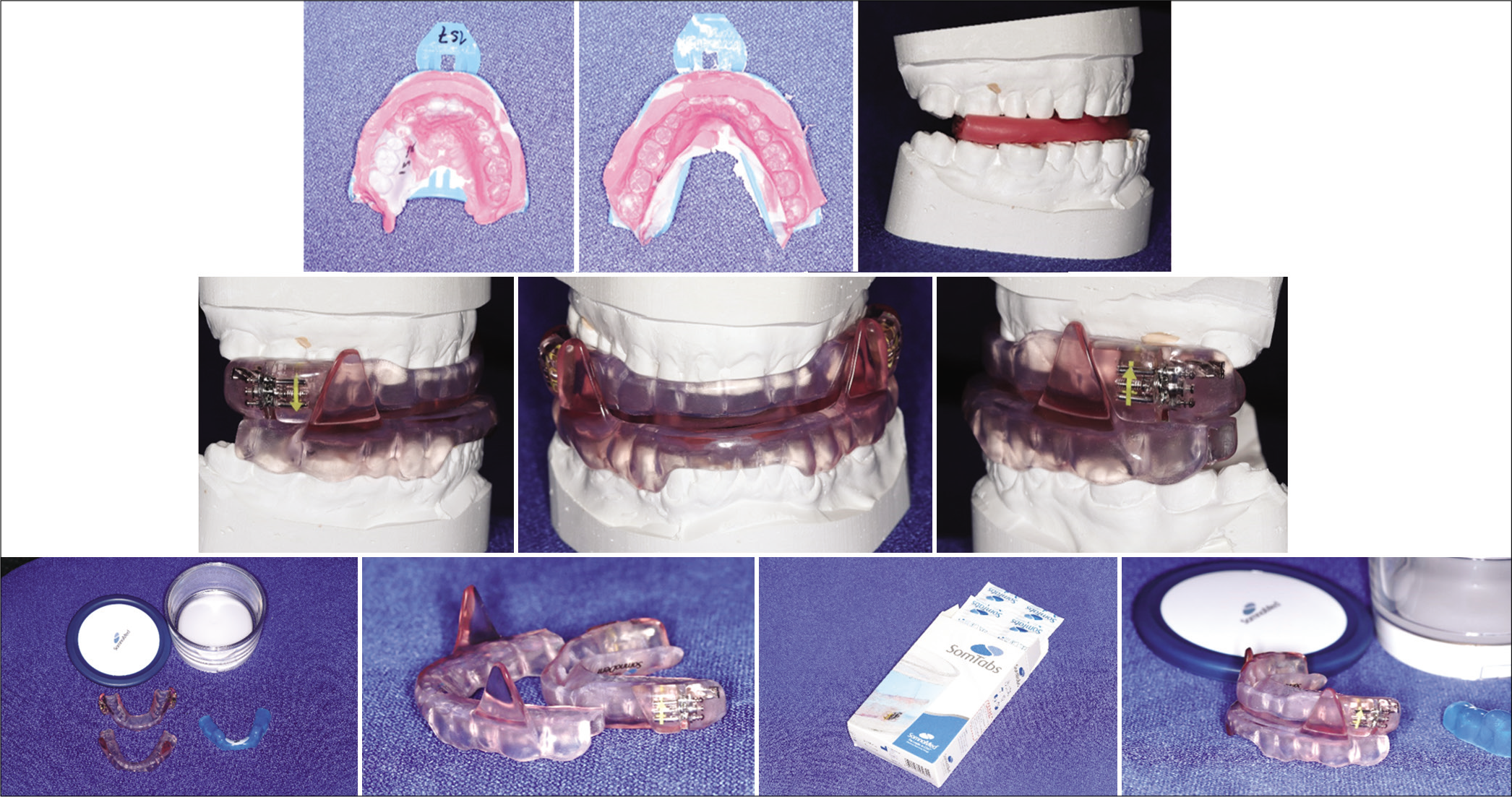
- A bite registration is made for the fabrication of mandibular advancement splint (MAS). The MAS, like SomnoMed (SomnoMed, SomnoDent MAS; SomnoMed Ltd, Crows Nest, Australia), is convenient to adjust as it is fitted with an adjustment screw that aids the patient to locate the best possible jaw position to control the symptoms of obstructive sleep apnea.
- Mandibular advancement splints fitted in an obstructive sleep apnea patient.
OBSTRUCTIVE SLEEP APNEA (OSA)
Although continuous positive airway pressure (CPAP) remains as the main modality of treatment for OSA, mandibular advancement splints (MASs) are increasingly used in the treatment of OSA as an effective alternative to CPAP.[33-35] According to the American Academy of Sleep Medicine, MAS is recommended for mild-to-moderate OSA, and for severe OSA, when CPAP is not tolerated [36,37] There are many different designs of MAS, the custom-made 2-piece adjustable appliances being the most efficient and comfortable. Example shown in [Figures 4 and 5] (SomnoDent MAS; SomnoMed Ltd., Crows Nest, Australia). MAS’s mechanism of action is through protrusion of the mandible resulting in an increase in the upper pharyngeal airway space caliber and reduced collapsibility.[33] For patients that do not tolerate CPAP and have compromised dental support for MAS, another appliance that was also studied by University of Sydney is the tongue stabilizing device (TSD). It was the prefabricated version that did not need any dental retention support whose mechanism of action is based on directing the tongue forward in a protrusive position by suction mechanism, and thereby improving upper airway structure and function.[35] Our department has been actively pursuing research on dental management of OSA by collaborating with multidisciplinary teams. Some of the key findings of our OSA collaborative studies are enumerated below;
Our pioneering work in 2001, which was the first prospective randomized placebo-controlled crossover trial on MAS aimed to assess the efficacy of an adjustable MAS and check for predictors of success. The comparator/ placebo appliance did not have any advancement of the mandible and the results showed it had no impact on the AHI or oxygen saturation. The MAS, similar to other research studies, provided partial or complete response in 62% of the sample, complete response in 37.5%, reduced snoring frequency and intensity, and improved sleep quality and daytime sleepiness, whereas the placebo appliance did not. The following four predictors of success were identified: Neck circumference, baseline AHI, and retropalatal airway space and mandibular plane angle.[34]
One of our studies using magnetic resonance imaging aimed to evaluate the mechanism of action of MAS in patients with OSA by assessing their effect on upper airway structure during wakefulness. One of the key finding of this study was that MAS improves the caliber of the upper airway by increasing the volume of the velopharynx in its lateral dimensions. Other novel findings of this study were that between responders and non-responders to MAS therapy, there were no significant differences in baseline cephalometric measurements or the volumes of the airway and soft tissue structures, but the effect of MAS on the caliber of the upper airway appeared to differ.[33]
The influence of nasal airway resistance (NAR) on MAS response was studied on patients with OSA, using posterior rhinomanometry in both sitting and supine positions, with and without MAS. The study concluded that not only NAR is an important predictive factor for MAS treatment outcome but also higher levels of NAR may negatively impact on MAS treatment outcome.[38]
The differences in three-dimensional upper airway morphology and overall skeletal configuration between responders and non-responders to MAS treatment in OSA were studied. The study revealed that there are no significant differences in upper airway morphology and in anatomical structures surrounding the upper airway between responders and non-responders to MAS treatment[39] [Figure 6].
Our RCT with the crossover design, comparing the efficacy of MAS and TSD in OSA individuals, showed that both appliances reduced (AHI) and improved sleep pattern.[35] Results also highlighted that there were higher complete response rate, overall acceptance, and compliance with MAS suggest, suggesting it to be a superior treatment for OSA. Nevertheless in patients that do not have enough periodontal support and that tolerate TSD, it is still a viable treatment option.
BIOMATERIALS APPLICATIONS IN ORTHODONTICS
Sydney miniscrew (SMS)
Orthodontic miniscrew (MS) failure rate is reported to be as high as 50% in some studies,[40] mainly due to lack of initial or primary stability. To counter failure rate and to promote primary stability of MSs, we designed and developed the SMS (SMS, Patent number: PCT2009014) which can be used with injectable bone graft substitutes (iBGS) in patients lacking the cortical bone thickness [Figure 7]. The SMS, a hollow cylindrical screw with lateral exit holes, was introduced with the aim of addressing the failure rates and improving the efficacy in application of MS in orthodontics. Bakopoulou et al. showed, in a rabbit model, that a combination of SMS and iBGS increased the primary stability.[41,42] iBGS is a composite of calcium sulfate (CaSO4) and dicalcium phosphate dihydrate (CaSO4-DCPD) forming a matrix (CaSO4-DCPD) with a distributed phase of β-tricalcium phosphate (β-TCP) granules in glycolic acid. The histomorphological and micro-CT showed uniform integration of SMS-iBGS with bone tissues. Furthermore, the study, through microtomography and histological analysis, revealed insights of biological integration between the hollow SMS and osseous structures of the alveolar bone.[41]
Magnets in orthodontics
In orthodontics, rare earth magnets, such as samarium-cobalt (SmCo5) and neodymium-iron-boron (Nd2Fe14B), have been applied successfully in both research and clinical practice, as the magnets have the ability to push, pull, or rotate a tooth or move the skeletal structures without the need for the magnet to be in direct contact with specific area of interest.[43-45] The University of Sydney’s contribution in regard to application of rare earth magnets in orthodontics is diverse, some of them are;
Magnetic Activator Device II (MAD II), a removable functional magnetic appliance, introduced by Darendeliler and Joho, was designed for severe Class II problems with repulsive posterior and attractive anterior magnets.[46] Adding magnets to the functional orthopedic treatment espouse several advantages, such as; (1) provide active functioning on a full time basis, (2) less bulky and cause lesser muscle fatigue as opposed to the conventional functional appliance, (3) delivers continuous force delivery system in comparison to conventional method’s intermittent rigid propulsion, and (4) offers better and faster adaptation for patients.[46,47]
Sydney Magnoglide is a refined designed to its predecessor MAD II. A fixed compliance-free minimal obstructive design having buccal placement of magnets encased in nickel and copper coated with a Signum metal bond (Heraeus, Hanau, Germany) to enhance acrylic resin retention. Moreover, the cobalt-chromium alloy framework allows removal of blocks in toto post-treatment. Phelan et al. conducted a prospective study in Class II division I malocclusion to evaluate the skeletal and dental outcomes of Sydney Magnoglide with untreated Class II controls. The study concluded that the appliance brings favorable skeletal mandibular changes with limited breakages and easy, chair-side repair.[48]
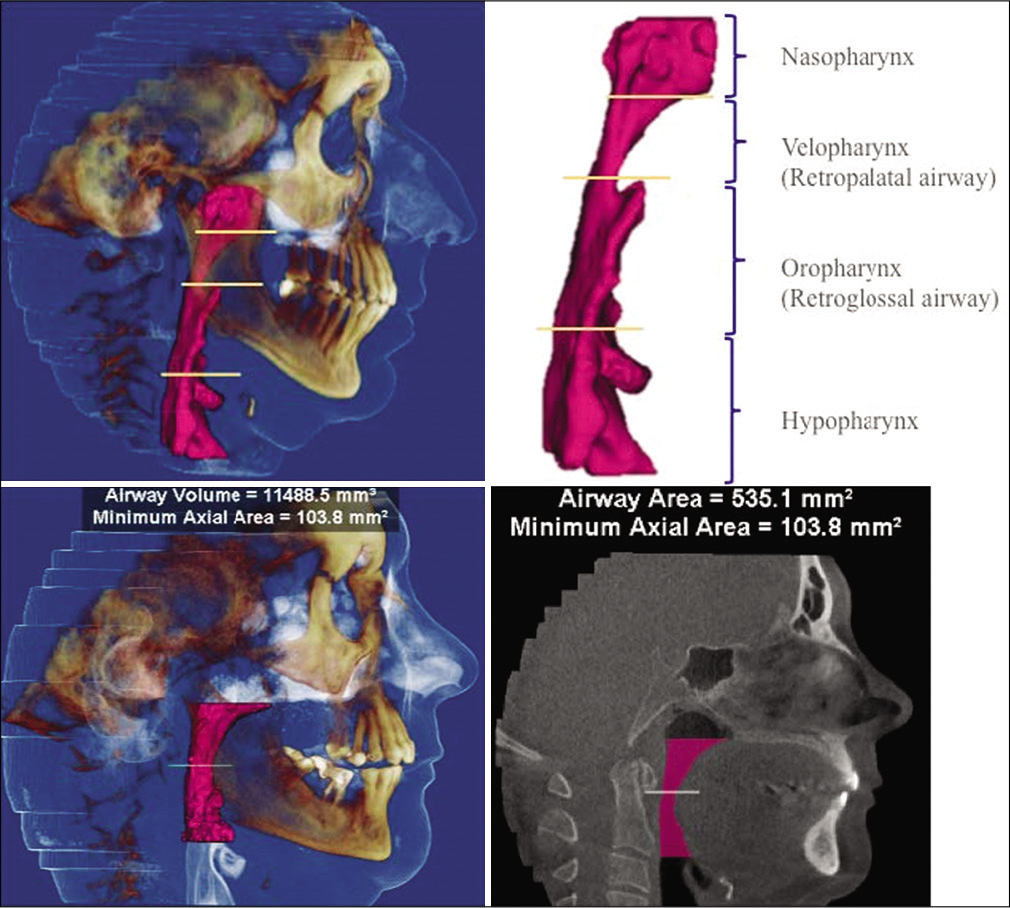
- Cone beam CT images of pharyngeal airway space studied in the responders and non-responders to mandibular advancement splints treatment.
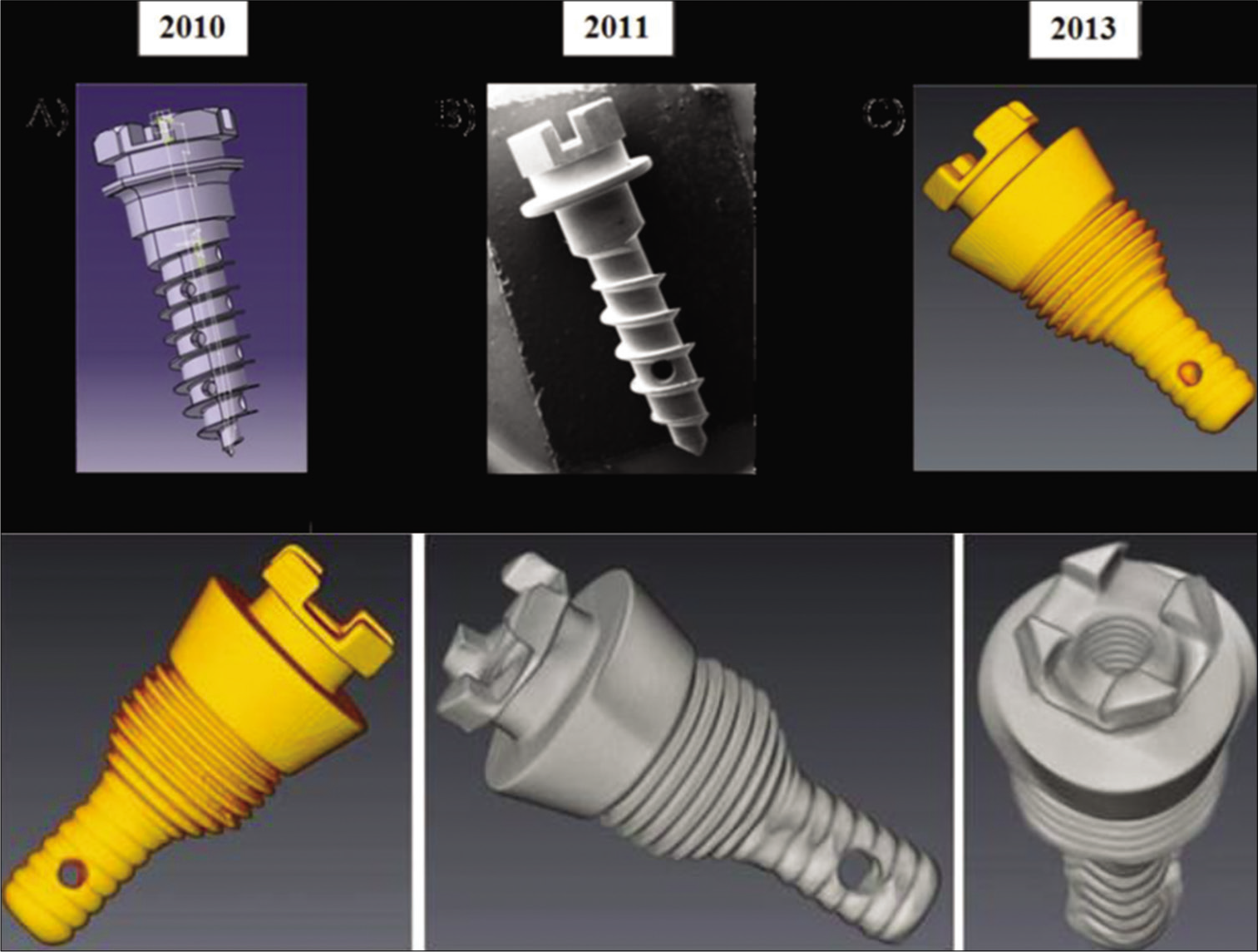
- The Sydney Mini Screw (SMS, Patent number: PCT2009014). The initial implant design introduced in 2010, the SMS has seen several refinements with the current design having a dispersion capacity of an injectable bone graft.
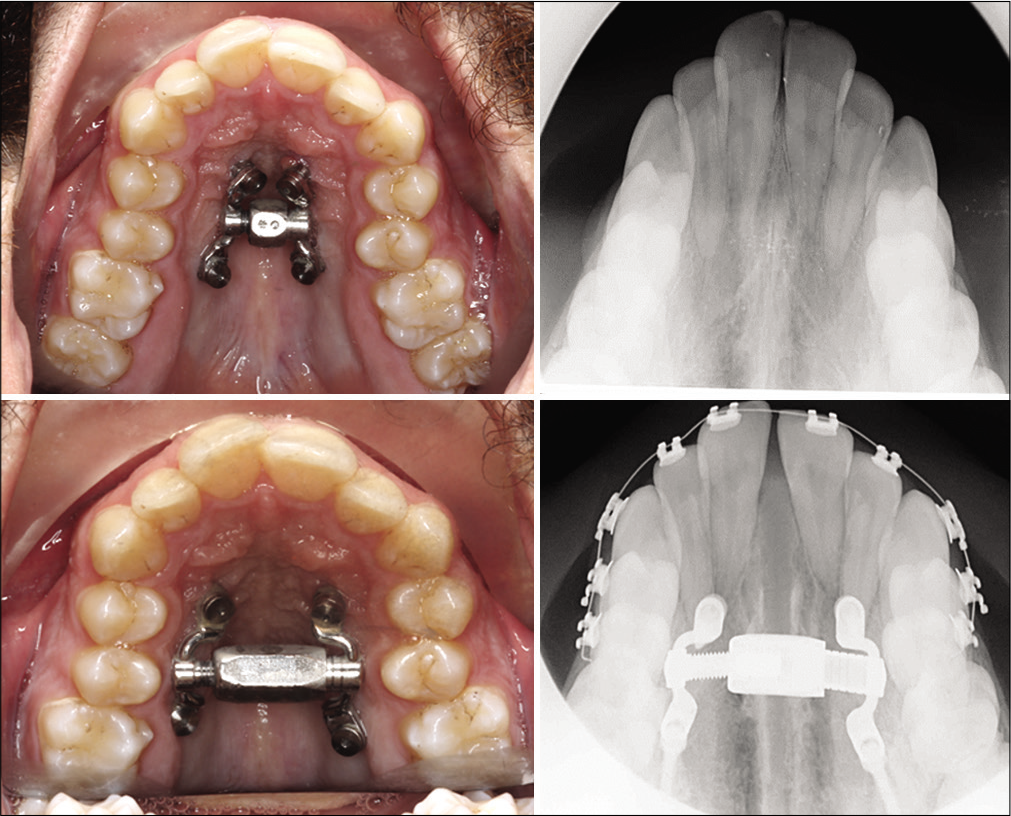
- Miniscrew-assisted rapid palatal expander could be an alternate for those individuals that do not prefer surgical intervention or is contraindicated for the correction of constricted maxillary arch.
MAXIMIZING ORTHOPEDIC TREATMENT OUTCOMES
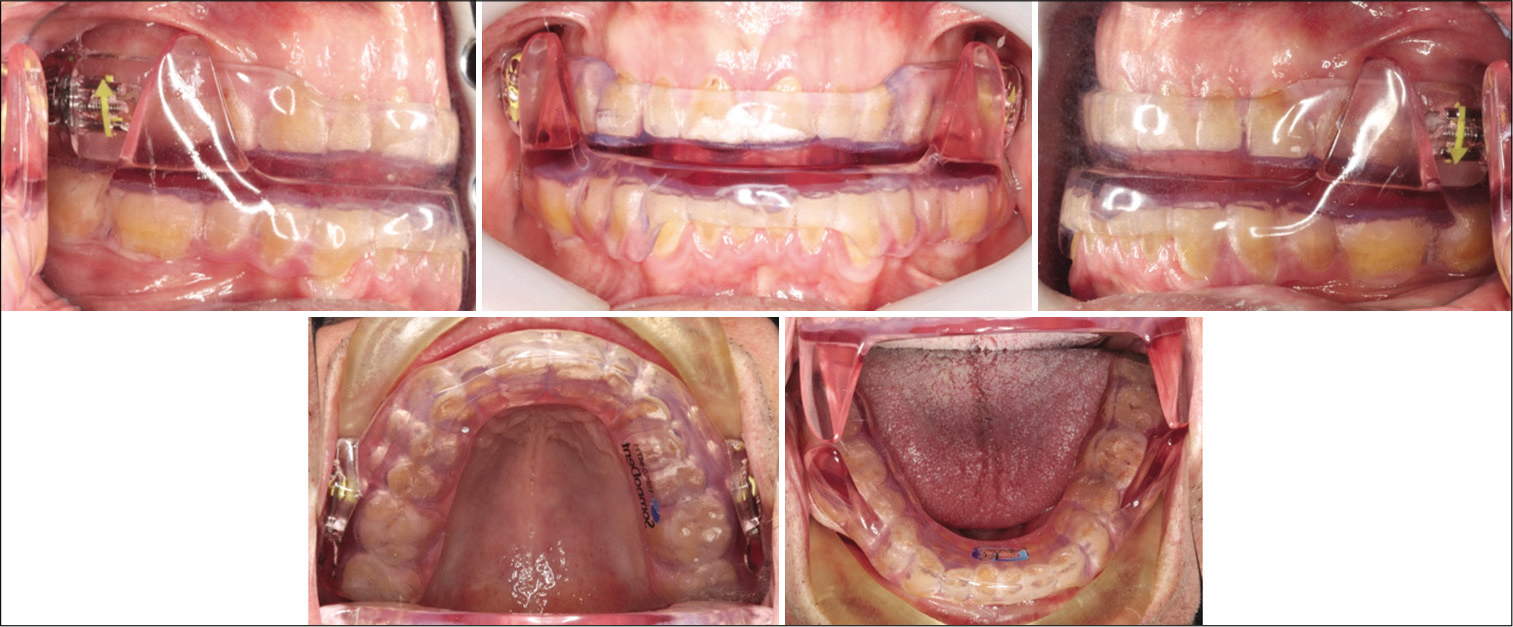
Incorporation of newer modalities of treatment and protocols has always been a highlight of our department. We would like to maximize the outcomes of orthopedic treatment of our patients that are especially suffering from a small maxilla by utilizing miniscrew-assisted rapid palatal expander (MARPE) [Figure 8] and alternating rapid maxillary expansion and constriction (Alt-RAMEC) protocol when needed, as well as intraoral force application methods in the management of maxillary retrusive children. MARPE when used in conjunction with Alt-RAMEC protocol (9 weeks) in the management of Class III malocclusion together with miniscrew supported lower lingual arch and heavy Class III elastics has shown to very effectively correct Class III in patients that are even at the later stages of their growth in significantly shorter time without the need to use face mask [Figure 9].[49] These results were also evaluated 4 years post-treatment and results remained stable indicating long-term success with this treatment modality without the need for face-mask.[50]
TELEORTHODONTICS AND RM IN ORTHODONTICS
Incorporation of teleorthodontics into routine care of patients is inevitable, as sooner or later, technology-driven health care will be omnipresent. RM, a part of teleorthodontics, is steadfastly allowing clinicians to distantly monitor patients with virtual consultations and management. RM is proposed to be a valuable adjunct in supplanting the chairside appointment time, especially, for the following reasons; (1) ability to do RM of sequential clear aligner therapy as well as compliance and oral hygiene, (2) decreased non-essential clinic visits thereby, not only enhancing dedicated chairside time for conventional treatment but also curb on the financial burden incurred from the clinic visits, especially for distantly placed patients that cannot frequently attend clinics.[51-53]
Dental monitoring (DM) (Paris, France) is one such artificial intelligence (AI)-assisted application designed for RM of dental treatment and management. The DM system (AI motion tracking algorithm) consists of three integrated platforms: A patient app, an analysis platform, and a Doctor Dashboard. DM calculates and quantifies 3-dimentional (3D) tooth movements through photographs or videos that patients capture using a smartphone camera. The aforementioned information amalgamated with AI-generated parameters of individual patient’s treatment progress are communicated to the orthodontist through a web-based Doctor Dashboard [Figure 10].
At the University of Sydney, we are [Figure 10] checking the applicability of this system in utilizing the dental workforce in the public system, to reduce the extensively long waiting times to get orthodontic treatment and its financial benefits if any.

- Intraoral images showing miniscrew-assisted rapid palatal expander with alternating rapid maxillary expansion and constriction protocol (9 weeks) used in conjunction with heavy Class III elastics in the management of Class III malocclusion.
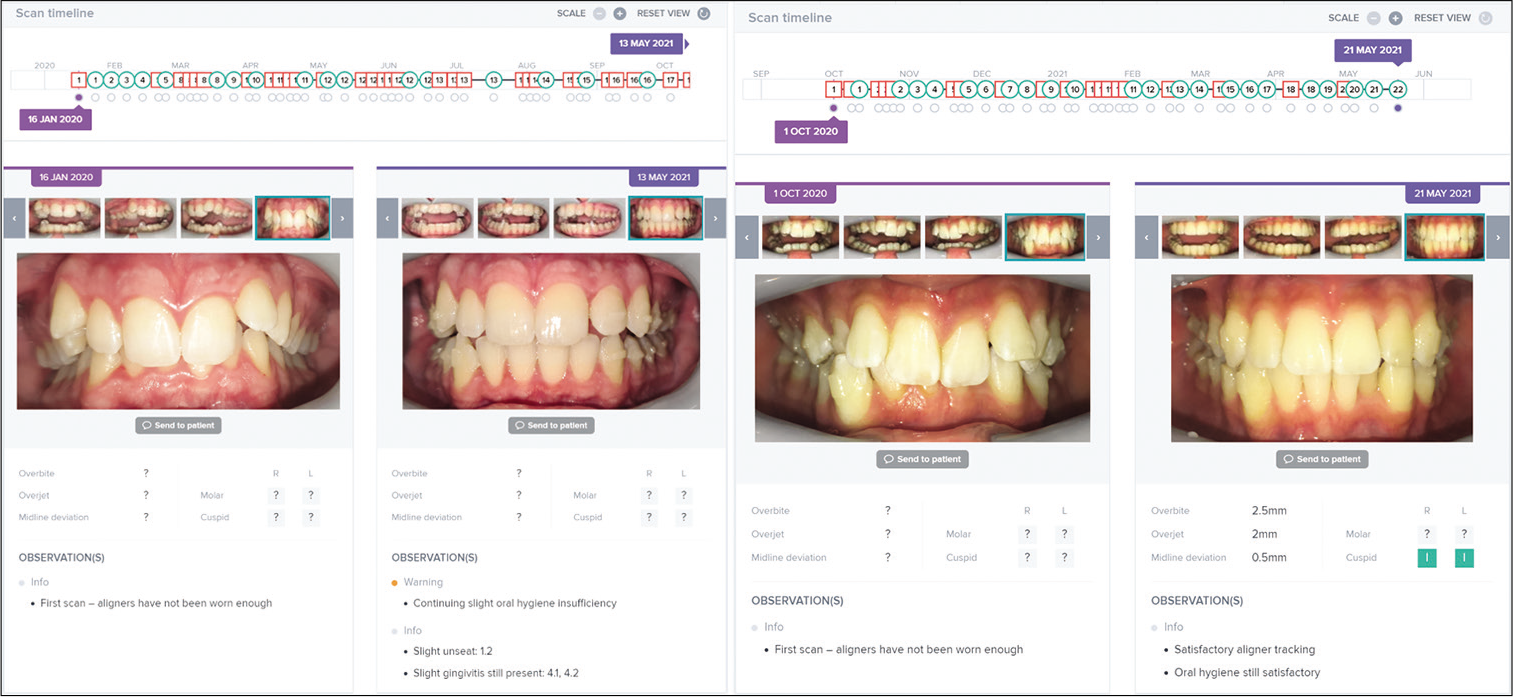
- Dental monitoring (Paris, France) utilizes artificial intelligence application designed for remote monitoring of dental treatment and management.
CONCLUSION
An outline of some of the main research interests at the University of Sydney Discipline of Orthodontics is provided. Our research on acceleration of OTM methods most importantly identified risks related to piezocision that if applied close to the roots it may cause iatrogenic damage and should be used carefully. MOP and piezocision were shown to result in greater root resorption after 4 weeks, and the studies conducted on LLLT study showed that there were no significant differences between LLLT and sham control groups in OIIRR repair. Further, protocols utilizing MARPE, Alt-RAMEC, and heavy Class III elastics through miniscrew supported lower lingual arch show promising results in short and long term management of skeletal class III patients, eliminating the need for face mask in non-compliant patients. With more research on, teleorthodontics along with technologies used for 3D diagnosis and management, 3D intra-extra oral scans and 3D printed appliances may become an integral part of routine orthodontics in the future.
Acknowledgment
The authors wish to thank Drs. Hui Theng Chong, Matthew T. Wong, and Nessa Finlay for their contribution during the preparation of this manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consents.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The effects of a clinically feasible application of low-level laser therapy on the rate of orthodontic tooth movement: A triple-blind, split-mouth, randomized controlled trial. Am J Orthod Dentofacial Orthop. 2020;157:444-53.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontically induced inflammatory root resorption (OIRR). Part I: Biological risk factors In: Forum Ortodontyczne/Orthodontic Forum: 2019. Poland: Termedia; 2019. p. :27-38.
- [Google Scholar]
- Root resorption and its association with alterations in physical properties, mineral contents and resorption craters in human premolars following application of light and heavy controlled orthodontic forces. Orthod Craniofac Res. 2004;7:79-97.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 12. The incidence of physiologic root resorption on unerupted third molars and its comparison with orthodontically treated premolars: A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:148.e1-9. discussion 148-9
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 9. Effect of systemic fluoride intake on root resorption in rats. Am J Orthod Dentofacial Orthop. 2007;131:34-43.
- [CrossRef] [PubMed] [Google Scholar]
- The extent of root resorption and tooth movement following the application of ascending and descending magnetic forces: A prospective split mouth, microcomputed-tomography study. Eur J Orthod. 2017;39:547-53.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 14. The amount of root resorption after force application for 12 weeks on maxillary and mandibular premolars: A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:492.e1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 23.Effects of 2 or 3 weekly reactivated continuous or intermittent orthodontic forces on root resorption and tooth movement: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2012;141:e29-37.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 11. Continuous vs intermittent controlled orthodontic forces on root resorption. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:8.e1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 10. Comparison of the effects of invisible removable thermoplastic appliances with light and heavy orthodontic forces on premolar cementum. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2008;133:218-27.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 17. Root resorption after the application of 2.5 and 15 of buccal root torque for 4 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;139:e353-60.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 24. Root resorption of the first premolars after 4 weeks of occlusal trauma. Am J Orthod Dentofacial Orthop. 2014;145:617-25.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 26. Effects of micro-osteoperforations on orthodontic root resorption: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2018;153:204-13.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 5. Volumetric analysis of root resorption craters after application of light and heavy orthodontic forces. Am J Orthod Dentofacial Orthop. 2005;127:186-95.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 7. Extent of root resorption under areas of compression and tension. Am J Orthod Dentofacial Orthop. 2006;129:504-10.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 13. Repair of root resorption 4 and 8 weeks after the application of continuous light and heavy forces for 4 weeks: A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:320.e1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 25. Extent of root resorption after the application of light and heavy buccopalatal jiggling forces for 12 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2015;147:738-46.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 8. Volumetric analysis of root resorption craters after application of controlled intrusive light and heavy orthodontic forces: A microcomputed tomography scan study. Am J Orthod Dentofacial Orthop. 2006;130:639-47.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 19. Comparison of the amounts of root resorption between the right and left first premolars after application of buccally directed heavy orthodontic tipping forces. Am J Orthod Dentofacial Orthop. 2011;140:e49-52.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 20. Effect of fluoride on orthodontically induced root resorption with light and heavy orthodontic forces for 4 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;140:e199-210.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 27. Effect of low-level laser therapy on the repair of orthodontically induced inflammatory root resorption: A double-blind, split-mouth, randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 2018;154:326-36.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 21. Extent of root resorption after the application of 2.5 and 15 tips for 4 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;140:e299-305.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 15. Analysis of elemental composition by using proton-induced x-ray and gamma-ray emissions in orthodontically induced root resorption craters of rat molar cementum after exposure to systemic fluoride. Am J Orthod Dentofacial Orthop. 2011;139:e193-202.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 22. Root resorption after the application of light and heavy extrusive orthodontic forces: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2012;141:e1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 16. Comparisons of root resorption and resorption craters after the application of light and heavy continuous and controlled orthodontic forces for 4.8 and 12 weeks. Am J Orthod Dentofacial Orthop. 2011;139:e279-84.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of piezocision on root resorption associated with orthodontic force: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2017;151:53-62.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 3. Hardness and elastic modulus after application of light and heavy forces. Am J Orthod Dentofacial Orthop. 2005;127:168-76.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 18. The extent of root resorption after the application of light and heavy controlled rotational orthodontic forces for 4 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;139:e495-503.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of root cementum: Part 2. Effect of different storage methods. Am J Orthod Dentofacial Orthop. 2003;124:561-70.
- [CrossRef] [Google Scholar]
- Physical properties of root cementum: Part 6. A comparative quantitative analysis of the mineral composition of human premolar cementum after the application of orthodontic forces. Am J Orthod Dentofacial Orthop. 2006;129:358-67.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of continuous versus intermittent orthodontic forces on root resorption: A microcomputed tomography study. Angle Orthod. 2018;88:733-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65:726-32.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163:1457-61.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of mandibular advancement splint and tongue stabilizing device in obstructive sleep apnea: A randomized controlled trial. Sleep. 2009;32:648-53.
- [CrossRef] [PubMed] [Google Scholar]
- CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med. 2014;10:943-9.
- [CrossRef] [PubMed] [Google Scholar]
- Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep. 2005;28:499-523.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Sleep. 2008;31:543-7.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in three-dimensional craniofacial anatomy between responders and non-responders to mandibular advancement splint treatment in obstructive sleep apnoea patients. Eur J Orthod. 2019;41:308-15.
- [CrossRef] [PubMed] [Google Scholar]
- Mini-implants in orthodontics: A systematic review of the literature. Am J Orthod Dentofacial Orthop. 2009;135:564.e1-19.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative histomorphological and micro computed tomography study of the primary stability and the osseointegration of The Sydney Mini Screw; a qualitative pilot animal study in New Zealand rabbits. Eur J Orthod. 2019;41:360-9.
- [CrossRef] [PubMed] [Google Scholar]
- An injectable bone graft substitute to enhance the primary stability of a novel miniscrew-The Sydney Mini Screw. Australas Orthod J. 2018;34:179-87.
- [Google Scholar]
- Rare earth magnets in orthodontics: An overview. Br J Orthod. 1999;26:29-37.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical application of magnets in orthodontics and biological implications: A review. Eur J Orthod. 1997;19:431-42.
- [CrossRef] [PubMed] [Google Scholar]
- Use of magnetic forces in growth modification In: Semin Orthod. Amsterdam: Elsevier; 2006. p. :41-51.
- [CrossRef] [Google Scholar]
- Class II bimaxillary protrusion treated with magnetic forces. J Clin Orthod. 1992;26:361-8.
- [Google Scholar]
- Magnetic activator Device II (MAD II) for correction of Class II, Division 1 malocclusions. Am J Orthod Dentofacial Orthop. 1993;103:223-39.
- [CrossRef] [Google Scholar]
- Skeletal and dental outcomes of a new magnetic functional appliance, the Sydney Magnoglide, in Class II correction. Am J Orthod Dentofacial Orthop. 2012;141:759-72.
- [CrossRef] [PubMed] [Google Scholar]
- A novel method for treatment of Class III malocclusion in growing patients. Prog Orthod. 2017;18:40.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of hybrid-Hyrax, Alt-RAMEC and miniscrew reinforced heavy Class III elastics in growing maxillary retrusive patients. A four-year follow-up pilot study. Australas Orthod J. 2017;33:199-211.
- [Google Scholar]
- Role of Virtual Reality (VR), Augmented Reality (AR) and Artificial Intelligence (AI) in tertiary education and research of orthodontics: An insight In: Semin Orthod. Amsterdam: Elsevier; 2021.
- [CrossRef] [Google Scholar]
- Teledentistry, doit-yourself orthodontics, and remote treatment monitoring. J Clin Orthod. 2016;50:718-26.
- [Google Scholar]
- Clinical outcomes and patient perspectives of Dental Monitoring® GoLive® with Invisalign®-a retrospective cohort study. Prog Orthod. 2020;21:16.
- [CrossRef] [PubMed] [Google Scholar]






