Translate this page into:
Three-dimensional craniofacial changes with maxillary expansion in young adult patients with different craniofacial morphology

*Corresponding author: H. Hong, Department of Orthodontics, Wuhan University, Wuhan, Hubei, China. drhehong@whu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Almaqrami BS, Ngan P, Alhammadi MS, Al-Somairi MA, Xiong H, Hong H. Three-dimensional craniofacial changes with maxillary expansion in young adult patients with different craniofacial morphology. APOS Trends Orthod 2022;12:187-201.
Abstract
Objectives:
Skeletally mature patients with transverse deficiency are best treated with surgically assisted rapid palatal expansion (RPE) procedure. Recent studies have shown that microimplant-assisted RPE (MARPE) appliances can be effective in achieving skeletal expansion in young adults. This retrospective study aimed to evaluate the skeletal and dental alveolar changes in response to treatment with MARPE appliances in three types of anteroposterior skeletal malocclusions using cone-beam computed tomography (CBCT) scans.
Material and Methods:
Seventy-eight subjects diagnosed with maxillary transverse deficiency and treated with the MARPE appliance (mean age of 22.9 ± 4.2 years) were divided into skeletal Class I, II, and III malocclusions with 26 subjects in each group. Pre- and post-treatment CBCT scans were used for superimposition to examine the skeletal and dentoalveolar changes following maxillary expansion treatment.
Results:
Significant lateral separation of the maxilla was found at the levels of the nasal floor, interzygomatic bones, and the inferior palatine margin of the alveolar process (P < 0.05) in the whole sample. Most of the sagittal and vertical variables change significantly in the whole sample and each studied group separately. Intergroup comparisons revealed no significant differences among the three skeletal classes except for the left frontozygomatic angle, left maxillary inclination angle, and torque in the first and second premolars. In Class III patients, the maxilla moved forward significantly in most of the cases (eight of 26 cases) (0.88°, P < 0.05) and the mandible moved downward and backward improving the anteroposterior skeletal relationship. Significant differences were also found in the vertical measurements (N-Me, MMP, and MP/SN, P < 0.05) in all three types of anteroposterior malocclusions.
Conclusion:
Maxillary expansion with the MARPE appliance in young adult patients induced different skeletal and dentoalveolar changes in the anteroposterior and vertical dimensions in each skeletal malocclusion with no significant difference among the three skeletal classes.
Keywords
Maxillary expansion in young adults
Cone-beam computed tomography microimplant-assisted rapid palatal expansion appliances
Types of malocclusions
Skeletal and dentoalveolar changes
INTRODUCTION
Maxillary transverse deficiency is a common problem in daily orthodontic practice.[1,2] Based on a recent systematic review,[3] the global prevalence of this malocclusion is around 9.4% and 11.7% in the permanent and mixed dentition stages, respectively. Patients with relative maxillomandibular transverse discrepancy can be treated non-surgically using various types of skeletally induced maxillary expansion appliances, orthodontic tooth movement, as well as orthognathic surgical correction. Conventional rapid palatal expansion (RPE) has proven to be a reliable treatment method for correcting transverse skeletal jaw disharmony in pre-pubertal patients.[4,5] However, interlocking of the midpalatal suture after puberty can cause unwanted side effects with RPE treatment[6] that may be detrimental to periodontal support.[7,8] Skeletally mature patients are best treated with surgically assisted RPE (SARPE) procedure. However, the high cost, complex treatment process, surgical morbidity,[9,10] and the invasiveness of the SARPE procedure can result in lateral rotation of the two palatal bones with minimal horizontal translation[11-13] that may discourage patients to undergo this surgical procedure. To ensure the expansion of the basal bone without surgical intervention and maintain the separated bone in consolidation, Lee et al.[14] and Wilmes et al.[15] introduced the microimplant-assisted RPE (MARPE) appliance and reported successful expansion of the maxilla with mid-palatal suture separation. Miniscrews have been added to RPE devices, as proposed by Wilmes et al.[15] in the hybrid hyrax appliance to enhance the orthopedic effects of maxillary expansion and to minimize the buccal tipping of teeth and the negative consequences on their periodontal support. Recently, much attention has been given to the use of MARPE and its use as a non-surgical treatment option for correcting maxillary transverse deficiency in young adult patients.[16-18] Choi et al.[16] conducted a larger study using the MARPE appliance in 69 young adult patients and reported success in opening the mid-palatal sutures in 86.96% of the subjects. Park et al.[17] reported success in obtaining sutural expansion in 14 young adult patients treated with the MARPE appliance. Cantarella et al.[19] reported success in opening the mid-palatal suture and a significant lateral displacement of the zygomaticomaxillary complex in 15 late adolescent patients treated with a bone-anchored maxillary expander. Zong et al.[18] also demonstrated success in obtaining sutural expansion with minimal dentoalveolar side effects in 22 young adult patients treated with MARPE appliance.
Maxillary skeletal expansion not only separates the midpalatal suture but also affects the circumzygomatic and circummaxillary sutural system.[20,21] It has been reported that opening of the mid-palatal suture has effects on both jaws in the vertical and sagittal dimensions.[20] Haas[22] and Davis and Kronman[23] reported forward and downward movements of the maxilla with the use of the Haas expansion appliance. However, Wertz[24] and Wertz and Dreskin[25] showed that the maxilla can move downward and backward in some cases and downward and forward in others after RPE treatment. Chung and Font[26] and Habeeb et al.[27] found that the maxilla was displaced downward and forward after RPE. However, the amount of forward movement was small and might not be clinically significant. Few studies in the literature reported on the skeletal and dentoalveolar response on different types of malocclusion with the MARPE appliance.[17,18]
Three-dimensional (3D) analysis using 3D scan offered several advantages over 2D radiographs; this includes but not limited to (1) 2D radiographs lack superimposition of anatomical areas in complex region; (2) 3D scans produced 1:1 images that are without magnification and distortion errors present in 2D radiographs; (3) the precise identification of the selected maxillofacial landmarks in the three orthogonal planes[28,29] making measurements more accurate and valid; (4) 3D scans allow clinicians to assess the third dimension such as determining the dental side effects of using MARPE appliance, especially buccal dental tipping and the loss of buccal bone thickness immediately after expansion; and (5) 3D scans allow clinicians to determine the mediolateral directional changes in cases where either skeletal separation of the maxillary sutures was not possible or when the expansion was not symmetric in sagittal or transverse direction.[30]
Limited information was available regarding the sagittal and vertical effects of this appliance after expansion in young adults. The aim of this investigation was to evaluate the skeletal and dentoalveolar response of different types of anteroposterior malocclusions after treatment with the MARPE appliance.
MATERIAL AND METHODS
Study design
The present retrospective study was approved by the Ethics Committee of the Hospital of Stomatology, Wuhan University (No 2020-B62).
Participants and intervention
Eighty-four patients consecutively treated with the MARPE appliance, six patients failed to obtain mid-palatal suture opening, and they were excluded from the study (success rate of 92.85%). The final sample included 78 cases (21 males and 57 females), consecutively treated with the MARPE appliance (Snap Lock Expander Forestadent, German) with a mean age of 22.9 ± 4.2 years and a range of 18.1–30.9 years. Of the 78 patients, 37 had bilateral posterior crossbite, 26 had unilateral posterior crossbite, and 15 were diagnosed with maxillary transverse deficiency without a dental crossbite. All patients were treated at the Orthodontic Clinic of the School of Dentistry, Wuhan University. A pilot study of 45 cases (15 cases in each class of malocclusion) was used to determine the minimum required study sample. A power analysis of the left maxillary inclination angle and the left frontozygomatic angle data was designed considering a mean difference of 0.88 mm in the left maxillary inclination angle and 0.76 mm in the left frontozygomatic angle between groups. The alpha level was 0.05 (5%), the beta level was 0.20 (20%) (i.e., power 80%). Accordingly, a sample size of 24 and 26 subjects was obtained based on a left maxillary inclination angle and the left frontozygomatic angle, respectively. The maximum calculated sample was considered during data collection. Pre-treatment cone-beam computed tomography (CBCT) scans of 78 young adult patients were obtained, these patients were subdivided into three groups; skeletal Class I (n = 26), skeletal Class II (n = 26), and skeletal Class III (n = 26). Subjects were classified as Class I if ANB angle was between 0° and 4°; Class II, it was >4°; and Class III, if it was <0°. There is no significant difference in the growth pattern across studied groups.
Inclusion criteria
The inclusion criteria were as follows: (1) Adult patients with mid-palatal suture maturation Stage D or E,[31] (2) skeletal transverse maxillary discrepancy; (3) treatment with MARPE as part of the overall treatment; (4) CBCT images were taken before and within 3 weeks after active expansion with the MARPE appliance; (5) absence of congenital facial anomalies and previous orthodontic treatment; and (6) presence of complete medical record and/or examination reports. The transverse discrepancy was measured by analyzing the relationship between the maxillary and the mandibular base width [Figure 1]. To determine the width of the mandible, the multiplanar view (MPV) image was opened, oriented in true frontal position, and scrolled down through the image until the furcation of the first molar was located. Then, the MPV image was scrolled posteriorly through the scan until the coronal cross-section through the center of the mandibular first molars was located. Through the axial view, the width of the mandible from the intersection of the cut line with the most buccal portion of the cortical plate on both the right and left sides was measured. For the maxilla, a similar method was employed; the only difference was that the axial and coronal cuts were taken at the position J-J “the depth of the concavity of the lateral maxillary contours, at the junction of the maxilla and the zygomatic buttress,” as shown in [Figure 1]. To calculate the amount of expansion required to achieve an ideal transverse jaw relationship, the measured difference between both jaws was subtracted from 5 mm.[32-34]

- Method used to diagnose transverse maxillary skeletal deficiency. Measurement of (a) mandibular and (b) maxillary widths; (c) frontal view of the relationship between maxillary and mandibular widths. In this patient, maxillary width is 59.32 mm, and mandibular width is 65.14 mm, for a maxillary transverse deficiency of 5.82 mm.
CBCT was used to evaluate palatal hard tissue thickness and to identify a suitable implant placement site, after determining the suitable implantation sites on the CBCT scan, it was drawn on the study model of the patient, 3D digital printing of pre-treatment study cast can enable the best fit and accuracy of the custom-made appliances. The 3D stereolithographic file was sent directly to the dental laboratory and the patient-specific casting mold was created.
Expander design and activation protocol
The MARPE appliance consisted of a jackscrew unit, four insertion slots for microimplants, a casting base, and a teeth retention device. The insertion slots, casting base, and the teeth retention device were connected as integral casting units and the jackscrew expander was welded into the casting body [Figure 2]. Following cementation of the appliance to the maxillary first premolars, second premolars, and first molars, four orthodontic miniscrews (A1, SYNTEC SCIENTIFIC CORPORATION, Taiwan, China), with a collar diameter of 2 mm and length of either 8 mm, 11 mm, or 14 mm (according to the thickness of the cortical bone and masticatory mucosa in the hard palate), were positioned [Figure 2]. The longer length of microimplants allowed bicortical engagement of the palatal and nasal floor, reducing the force transmitted to the anchored teeth during expansion.[35]

- Miniscrew-assisted palatal expander, intraoral occlusal view.
Subjects were instructed to activate the expansion screw at the rate of two turns (0.25 mm per turn) per day until interincisal diastema appeared and then one activation per day was applied until the required expansion was achieved. After completion, the MARPE was kept in place without further activation for at least 3 months to retain the expansion. The mean duration of expansion was 27 days (range, 18–35 days), and the mean amount of expansion was 6.7 mm (range, 4.5–8.8 mm).
3D analysis and measurements
The CBCT images were acquired before treatment (T1) and within 3 weeks of completion of expansion (T2) using the NewTom VGi 9 (Imola, Italy) at the Hospital of Stomatology, Wuhan University, using the following acquisition parameters: Large field of view (20 × 25 cm), 110 kV, 8.8 mAs, and 18 s exposure time. The selected voxel dimension was 0.3 mm and the slice thickness was 2 mm. Frankfort horizontal (FH) plane was made parallel to the floor with a crossing laser guide. According to the imaging protocol, the patient was instructed not to swallow or move during the scanning process.
To analyze skeletal changes induced solely by the MARPE appliance, post-expansion scans were obtained before patients received any other orthodontic appliances. Superimposition of the pre- and post-expansion CBCT scans was performed utilizing the fusion module of OnDemand3D (Cybermed, Daejeon, Korea) software using the anatomic structures of the entire anterior cranial as proposed by Cevidanes et al.[36] for non-growing patients. The accuracy of this method has been validated by Weissheimer et al.[37]
The 3D coordinated superimposition system was constructed by common X, Y, and Z planes. The X plane passed through the nasion, parallel to the FH plane as an axial plane. The Y plane was perpendicular to the X plane, passing through the nasion and sella points as a mid-sagittal plane. The Z plane was perpendicular to the other two planes, passing through the nasion as a coronal plane [Figure 3]. The skeletal and dental changes in the sagittal and vertical planes evaluated using cephalometric image constructed from the CBCT images, CBCT volume data were exported in Digital Imaging and Communications in Medicine format and imported in Dolphin 3D, orthogonal lateral cephalometric radiographs were created from 3D virtual models.
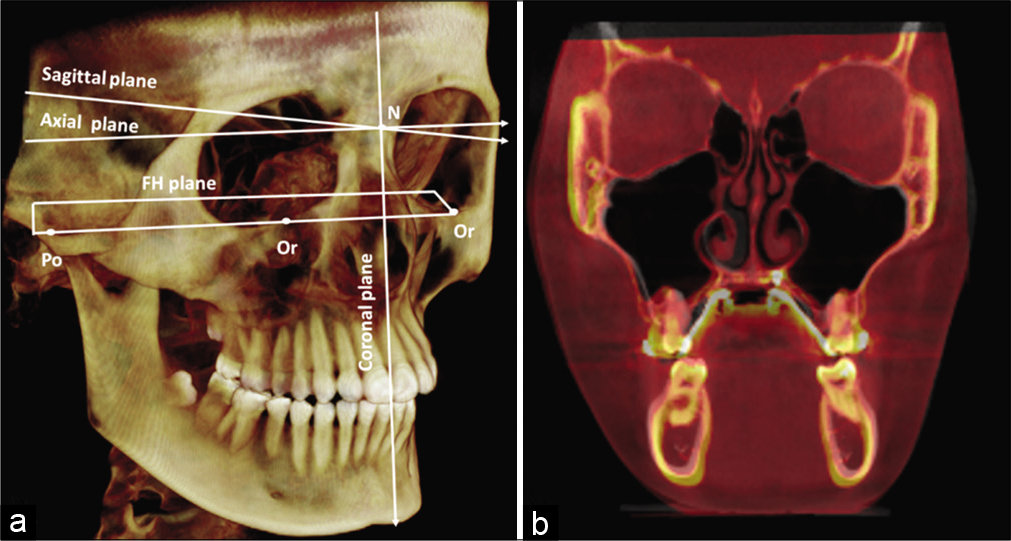
- (a) Lateral view of 3D rendering coordinated by three reference planes with zero point (0, 0, and 0) at the nasion. (b) Pre-treatment and post-treatment superimposed image of a MARPE patient.
The skeletal and dental changes were evaluated three dimensionally; nine skeletal and four dental measurements assessed changes in the transverse plan, six skeletal evaluated measurements in the sagittal plan, and six skeletal measurements measured the changes in the vertical plan. Detailed definitions of skeletal and dental measurements are presented in [Table 1] and [Figures 4-7].
| ABB | Measurements | Definition |
|---|---|---|
| Transverse measurements | ||
| Coronal measurements | ||
| FZA | Frontozygomatic angle | The angle formed by the lowest point of crista galli, the most external point of the frontozygomatic suture, and the most external point of the zygomaticomaxillary suture |
| MIA | Maxillary inclination angle | The angle between two lines: One that connects the most lateral point of the maxillary bone and the point where the cortical bones that form the floor of the nasal cavity and maxillary sinus merge, and the other line represented by the mid sagittal plane |
| LZD | Lower interzygomatic distance | Distance that extends from the most external point of the right zygomaticomaxillary suture to the most external point of the left zygomaticomaxillary suture |
| NCW | Nasal cavity width | The transverse width between the lateral most points of each nasal cavity |
| MW1 | Maxillary width between the alveolar crests | Maxillary width at inferior palatine margin of alveolar process of maxilla |
| MW2 | Maxillary basal bone width | Distance that extends from the depth of the concavity of the lateral maxillary contours, at the junction of the maxilla and the zygomatic buttress |
| 1st IPMW | First inter-premolar width | The distances between the most occlusal points of the mesiopalatal cusp of the first premolars. |
| IMW | Intermolar width | The distances between the most occlusal point of the mesiopalatal cusp of the first molars |
| APT | Torque of maxillary first premolar | The intersection angle between the Frankfort plane and the line connecting the central pit of the premolar crown to the furcation of the roots |
| AMT | Torque of maxillary first molar | The intersection angle between the Frankfort plane and the line connecting the central pit of the molar crown to the furcation of the roots |
| Axial measurements | ||
| RANS-LANS | Anterior mid-palatal suture opening | Distance between the right and left half of anterior nasal spine |
| Middle mid-palatal suture opening | Distance between the right and left half in the middle area of palate | |
| RPNS-LPNS | Posterior mid-palatal suture opening | Distance between the right and left half of posterior nasal spine |
| Sagittal measurements | ||
| SNA | SNA angle | The angle between 3-point landmarks sella, nasion and A points |
| SNB | SNB angle | The angle between 3-point landmarks sella, nasion and B points |
| ANB | ANB angle | The angle from A point, N point, and B point |
| A-Nperp | A-nasion vertical line | The linear distance measured between point B and nasion vertical line |
| B-Nperp | B-nasion vertical line | The linear distance measured between point B and nasion vertical line |
| AB diff/Nperp | AB diff/nasion vertical line | The linear differences between A-NV and B-NV |
| Vertical measurements | ||
| PP/SN | Palatal plane angle | The angle between sella-nasion (SN) and ANS-PNS (PP) |
| MMP | Maxillomandibular plane angle | The angle between the palatal plan and mandibular plan |
| MP/SN | Mandibular plane angle | The angle between sella-nasion (SN) and Go-Me (MP) |
| N-ME | Nasion-menton distance | The distance between the nasion and menton points |
| S-G | Sella-gonion distance | The distance between the sella and gonion points |
| J RATIO | S-G/N-ME | It is the ratio of posterior to anterior facial height |

- Skeletal angular measurements in the coronal zygomatic section: Frontozygomatic angle and maxillary inclination. Rt: Right, Lt: Left, MSP: Maxillary sagittal plane.

- Skeletal linear measurements in the coronal zygomatic section: Maxillary width was measured at level of nasal floor (1), lower interzygomatic distance (2), and maxillary width at inferior palatine margin of alveolar process of maxilla.

- Opening of mid-palatal suture in the axial section.

- Dental analysis in the coronal molar section: Intermolar distance and molar torque (a), inter-premolar distance and premolar torque (b).
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences software, version 26 (IBM Corp., Armonk, NY, USA) for Windows. To determine the reliability of results, random selection of 20% of the total examined sample was measured twice within a 2-week interval with the same observer and by another observer.
Absolute and relative technical error of measurements (TEM and rTEM) and intra- and inter-class correlation were calculated to assess the reliability and reproducibility of the measurements. To calculate the reliability of cranium orientation, 25% of the CBCT scans were reoriented based on the landmarks of basion and posterior clinoid process of sella turcica,[38] and intraclass correlation coefficient was calculated. Descriptive statistics, including the mean and standard deviation of each variable, were calculated. Data were checked for normal distribution using the Kolmogorov–Smirnov test. Intragroup comparison of skeletal and dentoalveolar measurements before and after MARPE was performed using paired t-tests or Wilcoxon signed-rank tests according to the normality of data distribution. For pairwise comparisons, one-way analysis of variance and Tukey’s honest significance or HSD test were used. Confidence level was set as P < 0.05.
RESULTS
The intra- and inter-examiner reliability analysis data are presented in [Table 2]. The mean maxillomandibular bone width discrepancy for the sample was 5.55 ± 1.53 mm. The mean total expansion was 6.7 mm with a range of 4.5–8.8 mm. The duration of expansion ranged from 18 to 35 days.
| Measurements | Intraexaminer reliability | Interexaminer reliability | ||||||
|---|---|---|---|---|---|---|---|---|
| ICC | TEM | rTEM | R | ICC | TEM | rTEM | R | |
| Right frontozygomatic angle | 0.959 | 0.024 | 3.63 | 0.99 | 0.940 | 0.08 | 13.4 | 0.99 |
| Left frontozygomatic angle | 0.956 | 0.026 | 4.008 | 0.99 | 0.977 | 0.05 | 7.84 | 0.99 |
| Right maxillary inclination | 0.967 | 0.03 | 4.26 | 0.99 | 0.970 | 0.06 | 8.48 | 0.99 |
| Left maxillary inclination | 0.962 | 0.034 | 5.69 | 0.99 | 0.963 | 0.05 | 9.15 | 0.99 |
| Lower interzygomatic distance | 0.937 | 0.07 | 7.68 | 0.99 | 0.962 | 0.09 | 10.14 | 0.99 |
| Nasal cavity width | 0.952 | 0.04 | 5.17 | 0.99 | 0.967 | 0.04 | 5.05 | 0.99 |
| Maxillary width between the alveolar crests | 0.972 | 0.32 | 32.25 | 0.96 | 0.977 | 0.22 | 22.4 | 0.98 |
| Maxillary basal bone width | 0.969 | 0.048 | 4.50 | 0.99 | 0.956 | 0.08 | 7.77 | 0.99 |
| 1st inter-premolar width | 0.963 | 0.25 | 16.3 | 0.98 | 0.976 | 0.09 | 6.15 | 0.99 |
| 2nd inter-premolar width | 0.973 | 0.10 | 9.11 | 0.99 | 0.971 | 0.05 | 4.90 | 0.99 |
| Intermolar width | 0.944 | 0.054 | 3.07 | 0.99 | 0.957 | 0.06 | 3.64 | 0.99 |
| Average torque of maxillary first premolar | 0.950 | 0.188 | 18.6 | 0.98 | 0.976 | 0.04 | 4.51 | 0.99 |
| Average torque of maxillary second premolar | 0.912 | 0.032 | 2.80 | 0.99 | 0.940 | 0.06 | 5.36 | 0.99 |
| Average molar torque | 0.968 | 0.047 | 4.68 | 0.99 | 0.955 | 0.05 | 5.05 | 0.99 |
| Anterior mid-palatal suture opening | 0.977 | 0.185 | 17.25 | 0.98 | 0.980 | 0.17 | 16.5 | 0.98 |
| Middle mid-palatal suture opening | 0.976 | 0.021 | 2.12 | 0.99 | 0.923 | 0.04 | 4.46 | 0.99 |
| Posterior mid-palatal suture opening | 0.978 | 0.026 | 2.54 | 0.99 | 0.956 | 0.04 | 4.31 | 0.99 |
| SNA | 0.980 | 0.022 | 45.6 | 0.99 | 0.977 | 0.02 | 42.72 | 0.99 |
| SNB | 0.972 | 0.021 | –9.28 | 0.99 | 0.978 | 0.10 | –46.73 | 0.99 |
| ANB | 0.950 | 0.022 | 8.12 | 0.99 | 0.979 | 0.08 | 28.90 | 0.99 |
| A-Nperp | 0.941 | 0.020 | –50.3 | 0.99 | 0.964 | 0.19 | –607.2 | 0.96 |
| B-Nperp | 0.980 | 0.034 | 29.9 | 0.99 | 0.973 | 0.28 | 211.2 | 0.99 |
| AB Diff/Nperp | 0.968 | 0.147 | 535.7 | 0.99 | 0.965 | 0.70 | 1037.6 | 0.95 |
| PP/SN | 0.971 | 0.023 | 9.40 | 0.99 | 0.929 | 0.03 | 12.19 | 0.99 |
| MMP | 0.952 | 0.034 | 5.95 | 0.99 | 0.935 | 0.04 | 7.18 | 0.99 |
| MP/SN | 0.979 | 0.024 | 4.28 | 0.99 | 0.979 | 0.04 | 7.64 | 0.99 |
| N-ME | 0.956 | 0.017 | 2.01 | 0.99 | 0.957 | 0.20 | 24.23 | 0.98 |
| S-G | 0.932 | 0.037 | –27.1 | 0.99 | 0.971 | 0.04 | –29.9 | 0.99 |
| J ratio | 0.955 | 0.003 | –74.8 | 0.98 | 0.937 | 0.006 | –164.6 | 0.95 |
ICC: Intraclass correlation coefficients, TEM and rTEM: Absolute and relative technical error of measurement
Transverse effects
Significant increase in transverse skeletal width was found with the measurements FZA and MIA for all types of malocclusions (P < 0.05). With linear measurements, significant increase was found with the measurements LZD, NCW, and maxillary width at inferior palatine margin and maxillary basal bone width with all types of malocclusions. The mid-palatal suture was separated in all patients, and the maxilla exhibited statistically significant lateral movement (P < 0.05) without significant difference between the various classes of malocclusions [Tables 3 and 4]. Regarding dental measurements, the measurements IPMW and IMW showed significant increase in width (P < 0.05), the torque of the maxillary premolars and molar was also significantly increased [Tables 5-7] in all classes of malocclusion. Intergroup comparisons revealed insignificant changes in all studied variables except for the left frontozygomatic angle, left maxillary inclination angle, and first and second average premolar torque [P < 0.05, Table 4].
| Measurements | Unit | Before expansion | After expansion | Treatment change | P value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Transverse measurements | ||||||||
| Coronal measurements | ||||||||
| Right frontozygomatic angle | ° | 78.9 | 3.87 | 80.8 | 4.05 | 1.88 | 1.08 | 0.000*** |
| Left frontozygomatic angle | ° | 78.0 | 4.14 | 80.12 | 4.23 | 2.04 | 1.05 | 0.000*** |
| Right maxillary inclination angle | ° | 94.04 | 3.51 | 95.98 | 3.53 | 1.93 | 1.10 | 0.000*** |
| Left maxillary inclination angle | ° | 93.8 | 4.45 | 95.8 | 4.54 | 1.95 | 1.23 | 0.000*** |
| Lower interzygomatic distance | mm | 92.6 | 4.41 | 95.6 | 4.50 | 2.95 | 1.46 | 0.000*** |
| Nasal cavity width | mm | 30.25 | 2.74 | 32.52 | 2.87 | 2.26 | 1.15 | 0.000*** |
| Maxillary width between the alveolar crests | mm | 33.17 | 2.58 | 36.69 | 3.03 | 3.51 | 1.64 | 0.000*** |
| Maxillary basal bone width | mm | 60.14 | 3.47 | 63.35 | 3.56 | 3.21 | 1.40 | 0.000*** |
| 1st inter-premolar width | mm | 26.2 | 2.94 | 30.8 | 3.64 | 4.65 | 2.30 | 0.000*** |
| 2nd inter-premolar width | mm | 30.8 | 2.94 | 35.50 | 3.62 | 4.66 | 2.21 | 0.000*** |
| Intermolar width | mm | 40.2 | 3.17 | 45.1 | 3.6 | 4.91 | 2.16 | 0.000*** |
| Average 1st premolar torque | ° | 90.07 | 5.13 | 93.24 | 5.20 | 3.16 | 2.56 | 0.000*** |
| Average 2nd premolar torque | ° | 90.92 | 5.51 | 94.10 | 5.56 | 3.18 | 2.75 | 0.000*** |
| Average molar torque | ° | 93.27 | 5.64 | 96.35 | 5.90 | 3.07 | 2.13 | 0.000*** |
| Axial measurements | ||||||||
| Anterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.43 | 1.57 | 3.43 | 1.57 | 0.000*** |
| Middle mid-palatal suture opening | mm | 0.00 | 0.00 | 3.27 | 1.47 | 3.27 | 1.47 | 0.000*** |
| Posterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.09 | 1.46 | 3.09 | 1.46 | 0.000*** |
| Sagittal measurements | ||||||||
| SNA | ° | 80.90 | 3.98 | 81.36 | 4.14 | 0.46 | 1.39 | 0.004** |
| SNB | ° | 79.42 | 6.19 | 78.52 | 6.31 | –0.90 | 1.26 | 0.000*** |
| ANB | ° | 1.48 | 5.09 | 2.84 | 4.94 | 1.36 | 1.58 | 0.000*** |
| A-Nperp | mm | 2.72 | 1.76 | 2.87 | 1.96 | 0.14 | 1.24 | 0.294 |
| B-Nperp | mm | 6.49 | 6.32 | 7.05 | 6.88 | 0.56 | 2.70 | 0.059 |
| AB diff/Nperp | mm | –3.76 | 6.31 | –4.18 | 6.55 | –0.41 | 2.88 | 0.207 |
| Vertical measurements | ||||||||
| PP/SN | ° | 9.94 | 4.02 | 10.14 | 4.19 | 0.20 | 1.84 | 0.32 |
| MMP | ° | 28.24 | 8.15 | 29.75 | 8.18 | 1.51 | 2.14 | 0.000*** |
| MP/SN | ° | 38.17 | 8.11 | 39.81 | 8.42 | 1.63 | 1.49 | 0.000*** |
| N-ME | mm | 116.8 | 7.10 | 118.9 | 6.98 | 2.16 | 1.81 | 0.000*** |
| S-Go | mm | 75.5 | 7.24 | 75.5 | 6.92 | 0.02 | 2.47 | 0.79 |
| J ratio | mm | 0.64 | 0.05 | 0.63 | 0.05 | –0.01 | 0.02 | 0.000*** |
| Measurements | Class I | Class II | Class III | ANOVA | Multiple comparisons post hoc tests | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | M | SD | M | SD | Cl I- Cl II | Cl I- Cl III | Cl II- Cl III | ||
| Transverse measurements | ||||||||||
| Coronal measurements | ||||||||||
| Right frontozygomatic angle | 1.86 | 1.16 | 2.00 | 1.07 | 1.78 | 1.03 | 0.772 | 0.902 | 0.961 | 0.742 |
| Left frontozygomatic angle | 1.70 | 0.91 | 2.50 | 1.00 | 1.93 | 1.11 | 0.017* | 0.011 | 0.693 | 0.137 |
| Right maxillary inclination angle | 1.81 | 1.20 | 1.83 | 0.86 | 2.17 | 1.19 | 0.421 | 0.998 | 0.536 | 0.472 |
| Left maxillary inclination angle | 2.36 | 1.28 | 1.40 | 1.19 | 2.09 | 1.05 | 0.014* | 0.020 | 0.690 | 0.080 |
| Lower interzygomatic distance | 2.98 | 1.44 | 2.96 | 1.57 | 2.91 | 1.41 | 0.983 | 0.997 | 0.980 | 0.993 |
| Nasal cavity width | 2.06 | 1.13 | 2.40 | 1.19 | 2.33 | 1.14 | 0.533 | 0.547 | 0.657 | 0.980 |
| Maxillary width between the alveolar crests | 3.69 | 1.73 | 3.43 | 1.64 | 3.43 | 1.59 | 0.808 | 0.844 | 0.839 | 1.000 |
| Maxillary basal bone width | 3.15 | 1.41 | 3.12 | 1.36 | 3.36 | 1.47 | 0.795 | 0.998 | 0.850 | 0.812 |
| Inter 1st premolar width | 4.50 | 1.89 | 4.75 | 2.66 | 4.71 | 2.37 | 0.919 | 0.919 | 0.939 | 0.997 |
| Inter 2nd premolar width | 4.73 | 1.92 | 4.78 | 2.80 | 4.46 | 1.84 | 0.859 | 0.997 | 0.867 | 0.879 |
| Intermolar width | 5.21 | 2.37 | 4.95 | 2.04 | 4.57 | 2.10 | 0.577 | 0.908 | 0.571 | 0.793 |
| Average 1st premolar torque | 3.46 | 1.73 | 3.92 | 3.73 | 2.11 | 1.18 | 0.028* | 0.835 | 0.006 | 0.064 |
| Average 2nd premolar torque | 4.17 | 2.14 | 3.63 | 3.59 | 1.75 | 1.55 | 0.003** | 0.789 | 0.000 | 0.051 |
| Average molar torque | 3.09 | 2.83 | 2.99 | 1.64 | 3.13 | 1.80 | 0.974 | 0.987 | 0.998 | 0.958 |
| Axial measurements | ||||||||||
| Anterior mid-palatal suture opening | 3.35 | 1.70 | 3.49 | 1.50 | 3.44 | 1.57 | 0.952 | 0.949 | 0.980 | 0.993 |
| Middle mid-palatal suture opening | 3.28 | 1.65 | 3.29 | 1.39 | 3.25 | 1.41 | 0.994 | 1.000 | 0.997 | 0.993 |
| Posterior mid-palatal suture opening | 3.18 | 1.51 | 2.98 | 1.41 | 3.11 | 1.52 | 0.884 | 0.875 | 0.987 | 0.942 |
| Sagittal measurements | ||||||||||
| SNA | 0.06 | 1.16 | 0.42 | 1.34 | 0.888 | 1.56 | 0.103 | - | - | - |
| SNB | –1.16 | 0.90 | –0.82 | 1.22 | –0.71 | 1.59 | 0.410 | - | - | - |
| ANB | 1.36 | 1.58 | 1.24 | 1.64 | 1.60 | 1.71 | 0.644 | - | - | - |
| A-Nperp | –0.18 | 0.98 | 0.60 | 1.47 | 0.03 | 1.13 | 0.059 | - | - | - |
| B-Nperp | 0.80 | 3.02 | 0.88 | 2.81 | 0.00 | 2.23 | 0.442 | - | - | - |
| AB diff /Nperp | –0.99 | 2.91 | –0.27 | 3.30 | 0.02 | 2.38 | 0.433 | - | - | - |
| Vertical measurements | ||||||||||
| PP/SN | 0.18 | 1.41 | 0.30 | 1.46 | 0.10 | 2.50 | 0.924 | - | - | - |
| MMP | 1.51 | 2.39 | 1.65 | 2.41 | 1.38 | 1.61 | 0.906 | - | - | - |
| MP/SN | 1.54 | 1.54 | 1.76 | 1.59 | 1.59 | 1.39 | 0.860 | - | - | - |
| N-ME | 2.43 | 1.78 | 2.28 | 1.79 | 1.78 | 1.88 | 0.413 | - | - | - |
| S-Go | –0.11 | 1.96 | 0.39 | 3.36 | –0.19 | 1.84 | 0.653 | - | - | - |
| J ratio | –0.01 | 0.01 | –0.005 | 0.03 | –0.01 | 0.01 | 0.400 | - | - | - |
| Measurements | Unit | Before expansion | After expansion | Treatment change | P-value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Transverse measurements | ||||||||
| Coronal measurements | ||||||||
| Right frontozygomatic angle | ° | 79.4 | 3.60 | 81.2 | 4.04 | 1.86 | 1.16 | 0.000*** |
| Left frontozygomatic angle | ° | 78.5 | 3.90 | 80.2 | 3.92 | 1.70 | 0.91 | 0.000*** |
| Right maxillary inclination angle | ° | 94.5 | 4.49 | 96.4 | 4.49 | 1.81 | 1.20 | 0.000*** |
| Left maxillary inclination angle | ° | 93.5 | 5.02 | 95.9 | 4.91 | 2.36 | 1.28 | 0.000*** |
| Lower interzygomatic distance | mm | 92.2 | 5.05 | 95.24 | 5.40 | 2.98 | 1.44 | 0.000*** |
| Nasal cavity width | mm | 30.1 | 2.34 | 32.2 | 2.40 | 2.06 | 1.13 | 0.000*** |
| Maxillary width between the alveolar crests | mm | 32.7 | 2.65 | 36.4 | 3.30 | 3.69 | 1.73 | 0.000*** |
| Maxillary basal bone width | mm | 60.3 | 3.00 | 63.4 | 3.31 | 3.15 | 1.41 | 0.000*** |
| Inter 1st premolar width | mm | 25.8 | 2.87 | 30.3 | 3.94 | 4.50 | 1.89 | 0.000*** |
| Inter 2nd premolar width | mm | 30.3 | 2.89 | 35.0 | 3.98 | 4.73 | 1.92 | 0.000*** |
| Intermolar width | mm | 39.9 | 2.91 | 45.1 | 3.50 | 5.21 | 2.37 | 0.000*** |
| Average 1st premolar torque | ° | 90.3 | 4.44 | 93.8 | 4.78 | 3.46 | 1.73 | 0.000*** |
| Average 2nd premolar torque | ° | 91.3 | 4.38 | 95.4 | 4.91 | 4.17 | 2.14 | 0.000*** |
| Average molar torque | ° | 94.1 | 3.93 | 97.2 | 5.44 | 3.09 | 2.83 | 0.000*** |
| Axial measurements | ||||||||
| Anterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.35 | 1.70 | 3.35 | 1.70 | 0.000*** |
| Middle mid-palatal suture opening | mm | 0.00 | 0.00 | 3.28 | 1.65 | 3.28 | 1.65 | 0.000*** |
| Posterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.18 | 1.51 | 3.18 | 1.51 | 0.000*** |
| Sagittal measurements | ||||||||
| SNA | ° | 80.9 | 4.85 | 81.0 | 4.63 | 0.06 | 1.16 | 0.857 |
| SNB | ° | 79.5 | 4.73 | 78.3 | 4.53 | –1.16 | 0.90 | 0.000*** |
| ANB | ° | 1.40 | 1.12 | 2.64 | 1.64 | 1.23 | 1.41 | 0.000*** |
| A-Nperp | mm | 2.69 | 1.82 | 2.50 | 2.12 | –0.18 | 0.98 | 0.525 |
| B-Nperp | mm | 4.78 | 3.56 | 5.59 | 4.30 | 0.80 | 3.02 | 0.159 |
| AB diff/Nperp | mm | –1.73 | 3.30 | –2.22 | 4.74 | –0.99 | 2.91 | 0.417 |
| Vertical measurements | ||||||||
| PP/SN | ° | 10.13 | 3.61 | 10.32 | 3.60 | 0.18 | 1.41 | 0.507 |
| MMP | ° | 27.9 | 6.07 | 29.4 | 5.31 | 1.51 | 2.39 | 0.003** |
| MP/SN | ° | 37.9 | 5.95 | 39.5 | 6.08 | 1.54 | 1.54 | 0.000*** |
| N-ME | mm | 117.7 | 5.90 | 120.1 | 5.99 | 2.43 | 1.78 | 0.000*** |
| S-Go | mm | 76.67 | 6.05 | 76.5 | 6.12 | –0.11 | 1.96 | 0.97 |
| J ratio | mm | 0.65 | 0.04 | 0.63 | 0.04 | –0.01 | 0.01 | 0.001** |
| Measurements | Unit | Before expansion | After expansion | Treatment change | P-value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Transverse measurements | ||||||||
| Coronal measurements | ||||||||
| Right frontozygomatic angle | ° | 79.73 | 4.15 | 81.7 | 4.35 | 2.00 | 1.07 | 0.000*** |
| Left frontozygomatic angle | ° | 78.4 | 4.92 | 80.9 | 5.10 | 2.50 | 1.00 | 0.000*** |
| Right maxillary inclination angle | ° | 93.5 | 3.19 | 95.3 | 3.16 | 1.83 | 0.86 | 0.000*** |
| Left maxillary inclination angle | ° | 92.9 | 3.49 | 94.4 | 3.69 | 1.40 | 1.19 | 0.000*** |
| Lower interzygomatic distance | mm | 93.5 | 3.91 | 96.52 | 3.72 | 2.96 | 1.57 | 0.000*** |
| Nasal cavity width | mm | 30.4 | 2.91 | 32.8 | 2.89 | 2.40 | 1.19 | 0.000*** |
| Maxillary width between the alveolar crests | mm | 32.5 | 2.57 | 35.9 | 2.80 | 3.43 | 1.64 | 0.000*** |
| Maxillary basal bone width | mm | 60.06 | 3.72 | 63.2 | 3.82 | 3.12 | 1.36 | 0.000*** |
| Inter 1st premolar width | mm | 25.4 | 2.33 | 30.2 | 3.07 | 4.75 | 2.66 | 0.000*** |
| Inter 2nd premolar width | mm | 30.3 | 2.45 | 35.1 | 3.29 | 4.78 | 2.80 | 0.000*** |
| Intermolar width | mm | 38.56 | 2.80 | 43.5 | 3.05 | 4.95 | 2.04 | 0.000*** |
| Average 1st premolar torque | ° | 87.4 | 5.14 | 91.3 | 5.93 | 3.92 | 3.73 | 0.000*** |
| Average 2nd premolar torque | ° | 87.9 | 5.68 | 91.6 | 6.12 | 3.63 | 3.59 | 0.000*** |
| Average molar torque | ° | 91.3 | 4.63 | 94.3 | 4.69 | 2.99 | 1.64 | 0.000*** |
| Axial measurements | ||||||||
| Anterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.49 | 1.50 | 3.49 | 1.50 | 0.000*** |
| Middle mid-palatal suture opening | mm | 0.00 | 0.00 | 3.29 | 1.39 | 3.29 | 1.39 | 0.000*** |
| Posterior mid-palatal suture opening | mm | 0.00 | 0.00 | 2.98 | 1.41 | 2.98 | 1.41 | 0.000*** |
| Sagittal measurements | ||||||||
| SNA | ° | 81.2 | 3.68 | 81.6 | 3.85 | 0.42 | 1.34 | 0.118 |
| SNB | ° | 74.2 | 4.00 | 73.3 | 4.37 | –0.82 | 1.22 | 0.002** |
| ANB | ° | 6.97 | 2.58 | 8.22 | 2.44 | 1.24 | 1.64 | 0.001** |
| A-Nperp | mm | 2.82 | 1.86 | 2.85 | 1.93 | 0.60 | 1.47 | 0.047* |
| B-Nperp | mm | 7.77 | 8.65 | 8.65 | 9.52 | 0.88 | 2.81 | 0.078 |
| AB/Nperp | mm | –8.09 | 5.41 | –8.02 | 6.86 | –0.27 | 3.30 | 0.912 |
| Vertical measurements | ||||||||
| PP/SN | ° | 10.7 | 2.94 | 11.0 | 3.37 | 0.30 | 1.46 | 0.290 |
| MMP | ° | 32.4 | 9.27 | 34.12 | 9.63 | 1.65 | 2.41 | 0.002** |
| MP/SN | ° | 43.4 | 7.84 | 45.21 | 8.62 | 1.76 | 1.59 | 0.000*** |
| N-ME | mm | 116.4 | 6.90 | 118.7 | 7.02 | 2.28 | 1.79 | 0.000*** |
| S-Go | mm | 71.5 | 6.00 | 71.9 | 6.11 | 0.39 | 3.36 | 0.839 |
| J ratio | mm | 0.61 | 0.053 | 0.60 | 0.05 | –0.005 | 0.03 | 0.281 |
| Measurements | Unit | Before expansion | After expansion | Treatment change | P-value | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |||
| Transverse measurements | ||||||||
| Coronal measurements | ||||||||
| Right frontozygomatic angle | ° | 77.7 | 3.65 | 79.5 | 3.52 | 1.78 | 1.03 | 0.000*** |
| Left frontozygomatic angle | ° | 77.25 | 3.51 | 79.19 | 3.49 | 1.93 | 1.11 | 0.000*** |
| Right maxillary inclination angle | ° | 94.07 | 2.63 | 96.2 | 2.74 | 2.17 | 1.19 | 0.000*** |
| Left maxillary inclination angle | ° | 95.03 | 4.62 | 97.1 | 4.68 | 2.09 | 1.05 | 0.000*** |
| Lower interzygomatic distance | mm | 92.2 | 4.21 | 95.2 | 4.25 | 2.91 | 1.41 | 0.000*** |
| Nasal cavity width | mm | 30.15 | 3.03 | 32.5 | 3.33 | 2.33 | 1.14 | 0.000*** |
| Maxillary width between the alveolar crests | mm | 34.3 | 2.26 | 37.7 | 2.82 | 3.43 | 1.59 | 0.000*** |
| Maxillary basal bone width | mm | 60.0 | 3.78 | 63.41 | 3.68 | 3.36 | 1.47 | 0.000*** |
| Inter 1st premolar width | mm | 27.4 | 3.27 | 32.1 | 3.65 | 4.71 | 2.37 | 0.000*** |
| Inter 2nd premolar width | mm | 31.9 | 3.26 | 36.3 | 3.55 | 4.46 | 1.84 | 0.000*** |
| Intermolar width | mm | 42.07 | 2.88 | 46.6 | 3.81 | 4.57 | 2.10 | 0.000*** |
| Average 1st premolar torque | ° | 92.5 | 4.60 | 94.6 | 4.38 | 2.11 | 1.18 | 0.000*** |
| Average 2nd premolar torque | ° | 93.5 | 5.07 | 95.2 | 4.85 | 1.75 | 1.55 | 0.000*** |
| Average molar torque | ° | 94.3 | 7.45 | 97.5 | 7.04 | 3.13 | 1.80 | 0.000*** |
| Axial measurements | ||||||||
| Anterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.44 | 1.57 | 3.44 | 1.57 | 0.000*** |
| Middle mid-palatal suture opening | mm | 0.00 | 0.00 | 3.25 | 1.41 | 3.25 | 1.41 | 0.000*** |
| Posterior mid-palatal suture opening | mm | 0.00 | 0.00 | 3.11 | 1.52 | 3.11 | 1.52 | 0.000*** |
| Sagittal measurements | ||||||||
| SNA | ° | 80.6 | 3.40 | 81.5 | 4.03 | 0.888 | 1.56 | 0.008** |
| SNB | ° | 84.5 | 4.93 | 83.8 | 5.13 | –0.71 | 1.59 | 0.031* |
| ANB | ° | –3.92 | 3.21 | –2.32 | 2.97 | 1.60 | 1.71 | 0.000*** |
| A-Nperp | mm | 2.89 | 1.96 | 2.77 | 1.91 | 0.03 | 1.13 | 0.89 |
| B-Nperp | mm | 6.91 | 5.52 | 6.92 | 5.65 | 0.00 | 2.23 | 0.970 |
| AB diff/Nperp | mm | –4.09 | 5.09 | –4.06 | 4.84 | 0.02 | 2.38 | 0.96 |
| Vertical measurements | ||||||||
| PP/SN | ° | 8.90 | 5.13 | 9.01 | 5.23 | 0.10 | 2.50 | 0.909 |
| MMP | ° | 24.3 | 6.87 | 25.70 | 6.96 | 1.38 | 1.61 | 0.000*** |
| MP/SN | ° | 33.1 | 7.10 | 34.71 | 7.05 | 1.59 | 1.39 | 0.000*** |
| N-ME | mm | 116.1 | 8.45 | 117.9 | 7.90 | 1.78 | 1.88 | 0.000*** |
| S-Go | mm | 78.3 | 7.93 | 78.1 | 7.15 | –0.19 | 1.84 | 0.595 |
| J ratio | mm | 0.67 | 0.06 | 0.66 | 0.058 | –0.01 | 0.01 | 0.001** |
Sagittal effects
In Class I sample, significant changes were found for the measurements SNB (–1.16°) and ANB (+1.23°, P < 0.05). No significant changes were found with SNA, A-NV, B-NV, and AB-NV [Table 5]. In Class II sample, significant changes were found for the measurements SNB (–0.82°), ANB (+1.24°), and A-NV distance (+0.6 mm) as a result of the downward and forward rotation of the maxilla and mandible [Table 6]. In Class III sample, significant changes were found with measurements SNA (+0.88°), SNB (–0.71°), and ANB (+1.6°) [Table 7]. The intergroups comparison showed insignificant changes in the sagittal plane measurements as presented in [Table 4].
Vertical effects
In Class I sample, significant changes were found with measurements MMP (+1.51°), MP/SN (+1.54°), N-Me (+2.43 mm), and the Jarabak ratio (–0.01 mm) [Table 5].
In Class II sample, significant changes were found with measurements MMP (+1.65°), MP/SN (+1.76°), and N-Me (+2.28 mm) [Table 6]. In Class III sample, significant changes were found with the measurements MMP (+1.38°), MP/SN (+1.59°), N-Me (+1.78 mm), and the Jarabak ratio (–0.01 mm) [Table 7]. The intergroups comparison showed insignificant changes in the sagittal plane measurements as presented in [Table 4].
DISCUSSION
The use of MARPE appliance has recently been offered to young adult patients as a treatment option for correcting maxillary transverse discrepancy. However, there is limited information on the craniofacial changes of this new technique specifically in skeletally matured patients. The bone-borne anchorage device can result in skeletal and dentoalveolar expansion in young adults despite the increased resistance of the mid-palatal and circumaxillary sutures.[6,39]
The total expansion was 6.7 mm ± 4.5–8.8 mm. This variation of expansion was expected as not all cases required the same amount of expansion based on the baseline transverse dimension measurement as well as the stage of mid-palatal suture maturation. This is normally expected[17,18,40] but the clinical stopper of such an expansion in that all cases should end up with over-correction as recommended to counteract for natural relapse.
Expansion with the MARPE appliance effectively achieved dentoalveolar as well as skeletal expansion by separation of the mid-palatal suture in 92.85% of the subjects in the current study. The skeletal index used in this study was the extended distance of mid-palatal suture. The increase in IMW width (4.91 mm) accounted for 66.4% of the skeletal expansion at the mid-palatal suture (3.26 mm), 65.4% of the skeletal expansion at J point (3.21 mm), 60.0% of the skeletal expansion at the lower interzygomatic distance (2.95 mm), and 46.0% of the skeletal expansion at the nasal cavity (2.26 mm). This pattern of expansion in the coronal plane indicates that the maxillary expansion followed almost parallel pattern in all kinds of malocclusion without any significant differences between them, in contrast to the expansion pattern reported with other studies.[8,17]
In the current study, 66.4% of transverse expansion in the molar region was attributed to skeletal expansion, 5% to alveolar expansion at alveolar process of maxilla (0.25 mm), and 28.5% to dental expansion at the cusp tip (1.4 mm). The result is in agreement with the study of Zong et al.[18] and in contrast with other studies.[16,17] Choi et al.[16] reported orthopedic expansion in a young adult sample with 43% of transverse expansion attributed to skeletal expansion, while Park et al.[17] found that the amount of skeletal expansion was 37% of total expansion in intermolar region. The possible cause for this variation could be due to the varying in appliance design, mini-implant length, and insertion depths, the two of the previous studies used mini-implant with 7 mm length for all of their samples, whereas in this study, the mini-implant length was either 11 mm or 14 mm. A recent study reported that the length of miniscrews used in MARPE affected maxillary transverse expansion and that bicortical miniscrews have greater stability and allowed more horizontal expansion than monocortical miniscrews.[35]
On the axial plane, the mid-palatal suture was successfully split by expansion with the MARPE appliance in 92.85% of the patients. In the previous studies, the use of maxillary skeletal expanders (MSE), a kind of MARPE appliance, produced almost parallel expansion in the axial view.[19,41] Cantarella et al.[19] utilized MSE maxillary expander activated by 6.8 ± 1.9 mm on all patients and found that the split at anterior nasal spine (ANS) and at posterior nasal spine (PNS) was 4.8 and 4.3 mm, respectively. The amount of sutural separation at PNS was 90% compared to that at ANS, showing at the opening of the mid-palatal suture was almost perfectly parallel anteroposteriorly. The results in the current study agree with Cantarella et al.[19] that the borders of the mid-palatal suture moved almost perfectly parallel to each other since the amount of split at PNS (3.09 mm) was 90% of that at ANS (3.43 mm).
The use of four mini-implants in the MARPE appliance, with a considerable anteroposterior distance between them and adequate length of microimplants allowed bicortical engagement of the palatal and nasal floor, reducing the force transmitted to the anchored teeth during expansion, consequently, the magnitude of separation force will be larger and distributed along the entire suture length allow more parallel split of the mid-palatal suture in an anteroposterior direction.[35,42]
As for dental expansion, 68 of the 78 patients presented dental tipping of maxillary premolars and molar after treatment with the MARPE appliance. The previous studies using MARPE appliances reported a buccal tipping of 2.6°–5.8° for the maxillary first molar.[17,18] These values are similar to those found in the present study. The possible reasons could be that part of mechanical force generated from MARPE was transmitted to the anchored teeth since MARPE was a hybrid appliance. Even though the relative position of anchored teeth did not change in alveolar bone, dental tipping would still be observed because of alveolar bending. For adult patients, the bone resistance was significantly greater, considerable part of orthopedic force would be exerted on anchored teeth, leading to both of dental tipping and alveolar bending.
In addition, the mechanical force of MARPE led not only to the transverse expansion but also to the maxillary rotation. Our study demonstrates that the relationship between the maxillary basal bone and the zygomatic bone was maintained during the expansion and that they rotate together around a common center of rotation. The larger augmentation in lower interzygomatic distance (+2.95 mm) and the increases in the frontozygomatic angle of average 1.96° indicates outward rotation of the zygomatic bone. As the zygomatic bone is pushed laterally by the underlying maxilla, it tends to rotate around the weaker frontozygomatic suture, generating an increase in the frontozygomatic angle. This significant displacement of the zygomatic bone indicates that a larger midfacial orthopedic response can be achieved with the MARPE appliances. This result was in accordance with the result of Cantarella et al.[19] who reported significant increase in lower interzygomatic distance by 4.6 mm. The pattern of lateral displacement of the zygomaticomaxillary complex within the craniofacial complex was also calculated as the ratio between the increase in frontozygomatic angle (average of the right and left sides) and the increase in the lower interzygomatic distance this ratio was 0.66° per millimeter (1.96°/2.95 mm).
The intergroup comparison revealed significant increase in the left frontozygomatic angle and decrease in the left maxillary inclination angle in Class II compare to Class I and Class III and also significant decrease in the first and second premolars torque in Class III compare to Classes I and II. The previous study[19] reporting negligible changes in these dimensions after maxillary expansion might have been based on the results from averaging mixed samples with different kinds of malocclusion. Significant change in the left frontozygomatic angle and left maxillary inclination angle could be due to asymmetrical expansion in transverse direction after MARPE treatment as demonstrated recently[30,43] with nearly half of the patients experiencing significant asymmetry. On average, one half of maxilla moved 2.1 mm more than the opposite half.
For the sagittal and vertical measurements, our data clearly showed that in all classes of malocclusion, there was a slightly forward displacement of the maxilla and backward rotation of mandible in the sagittal plane, this forward displacement was more prominence and significant in Class III than Class II and Class I patients. This result is in accordance with the study conducted by Hourfar et al.[44] which reported advancement of the maxilla based on SNA in the Class III patients treated with a combined tooth- and bone-borne appliance. It should be noted that in our study, even the ANB difference in Class III patients improved by +1.6° as the result of an anterior movement of the maxilla and downward and backward rotation of the mandible, the amount of maxillary forward movement was small (+0.88°), which might not be clinically significant. Thus, one should not anticipate that the use of MARPE appliance can correct a skeletal Class III malocclusion by spontaneous forward maxillary displacement, as suggested by Haas.[45] This finding was in agreement with the previous report by Chung and Font[26] who found that the maxilla was displaced downward and forward after RPE; however, the amount of forward movement was small and might not be clinically significant. Chung et al. also found that the maxilla displaced forward to a statistically significant amount immediately after SARPE in adults; however, the movement was minimal (+.6°).
Our results also showed that the maxilla always moves downward and moves varying degrees, from slightly backward (31 of 78 patients) to sometimes significantly forward (47 of 78 patients) in all kinds of malocclusion (Class I, 10 patients backwards vs. 16 forwards, Class II, 13 patients backwards vs. 13 forwards, and Class III, 8 patients backwards vs. 18 forwards) during suture opening. This finding is in agreement with the previous reports by Wertz[24] and Wertz and Dreskin[25] who reported that the maxilla moved downward and backward in some patients and downward and forward in others after RPE treatment. However, our data disagreed with those of de Silva Fo et al.[46] who found that the maxilla did not change sagittally but moved downward after RPE, displaying downward and backward rotation in the palatal plan. Gardner and Kronman[47] underlined that opening the spheno-occipital synchondrosis could be responsible for the forward displacement of the maxilla, this change happens in the active phase of treatment. Through this finding, we can concluded that the maxillary expansion might help in correcting the sagittal discrepancy in forward direction in some patients and in backward direction in another but it is unpredictable in determining which patients would benefit from maxillary expansion.
McNamara et al.[48] found that the use of a bonded RPE results in significant sagittal Class II correction in the early mixed dentition from mandibular forward displacement. However, Volk et al.[49] concluded that maxillary expansion might help Class II correction in some patients but is unpredictable in determining which patients would benefit from maxillary expansion. They found improvement in Class II malocclusions about 50% of the time, but in some cases, the Class II malocclusion became worse. In our study in Class II patients even the change in SNA was non-significant (+0.4°), however, the A-Nperp measurement was increased in significant manner (+0.6 mm) and without mandibular forward displacement (SNB –0.82°) which could be led to slight advancement in maxilla.
Regarding the vertical measurements, we found that after treatment with the MARPE appliance, there was a significant increase in vertical dimension for the variables MMP, MP/SN, and N-Me in all classes of malocclusions. This result is in agreement with the previous study by Chung and Font[26] who found that after RPE treatment, the mandible rotated downward and backward, which resulted in a smaller SNB, higher mandibular plane angle, and longer anterior facial height. The variable MMP increased because of a downward and backward displacement of the maxilla. Wertz et al.[24] noted that the increase in the mandibular plane angle could be accompanied by a decrease in the SNB angle. The increase in the mandibular plane is responsible for the increase in anterior facial height, N-Me, in these groups of patients. This could be due to the downward displacement of the maxilla as a consequent of anterior position of expander. Yoon et al.[50] reported that when the jet screw was positioned in the anterior direction, it showed greater changes in overall transverse displacement and showed increased clockwise rotation of the maxilla, in contrast, when the expander was positioned in the posterior direction and showed smaller changes in overall displacement with overall total intrusion of the maxilla. The previous studies by Davis and Kronman[23] Wertz[24] and de Silva Fo et al.[46] also showed an increase in the mandibular plane angle; Farronato et al.[20] and Maspero et al.[51] found a decrease in SNB in Class III after the RPE treatment. Basciftci and Karaman[52] found that the mandible rotated downward and backward and that the lower facial height increased even though a bonded RPE was used.
In addition to its strengths, the limitations of our current study were the absence of a control group, super short-term observation, and retrospective nature with possible selection bias. Further prospective studies involving larger numbers of patients and long-term evaluation of stability after expansion with the MARPE appliance is warranted.
CONCLUSION
Skeletal transverse expansion was obtained in 92.85% of the young adult patients diagnosed with transverse maxillary deficiency in all three types of sagittal malocclusions
There is no difference in the skeletal and dental response to maxillary expansion with MARPE appliances in between the three skeletal classes with exception of the left frontozygomatic angle, left maxillary inclination angle, and torque in the first and second premolars
In Class III patients, the maxilla moved forward significantly and the mandible moved downward and backward improving the anteroposterior skeletal relationship. Maxillary expansion also induced a downward and backward rotation of the mandible for all of classes of malocclusions resulting in an increase in anterior total face height.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000;117:567-70.
- [CrossRef] [Google Scholar]
- The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200-17.
- [Google Scholar]
- Global distribution of malocclusion traits: A systematic review In: Dental Press J Orthod. Vol 23. 2018. p. :40.e1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal expansion: Just the beginning of dentofacial orthopedics. Am J Orthod Dentofac Orthop. 1970;57:219-55.
- [CrossRef] [Google Scholar]
- Rapid palatal expansion (RPE): Meta-analysis of long-term effects. Orthod Craniofac Res. 2018;21:225-35.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal growth studied on human autopsy material: A histologic microradiographic study. Am J Orthod. 1975;68:42-54.
- [CrossRef] [Google Scholar]
- Long-term effects of rapid maxillary expansion followed by fixed appliances. Angle Orthod. 2010;80:5-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253-62.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically assisted rapid palatal expansion: A literature review. Am J Orthod Dentofacial Orthop. 2008;133:290-302.
- [CrossRef] [PubMed] [Google Scholar]
- Complications following surgically assisted rapid palatal expansion: A retrospective cohort study. J Oral Maxillofac Surg. 2012;70:2394-402.
- [CrossRef] [PubMed] [Google Scholar]
- Age changes in the human frontozygomatic suture from 20 to 95 years. Am J Orthod. 1976;69:411-30.
- [CrossRef] [Google Scholar]
- Direct bone placement of the hyrax fixation screw for surgically assisted rapid palatal expansion (SARPE) J Oral Maxillofac Surg. 2006;64:1313-7.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional evaluation of surgically assisted implant bone-borne rapid maxillary expansion: A pilot study. Am J Orthod Dentofacial Orthop. 2007;131:S92-9.
- [CrossRef] [PubMed] [Google Scholar]
- Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofac Orthop. 2010;137:830-9.
- [CrossRef] [PubMed] [Google Scholar]
- Application and effectiveness of a mini-implant-and tooth-borne rapid palatal expansion device: The hybrid hyrax. World J Orthod. 2010;11:323-30.
- [Google Scholar]
- Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016;86:713-20.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J Orthod. 2017;47:77-86.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal and dentoalveolar changes in the transverse dimension using microimplant-assisted rapid palatal expansion (MARPE) appliances. Semin Orthod. 2019;25:46-59.
- [CrossRef] [Google Scholar]
- Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. Prog Orthod. 2017;18:34.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal and vertical effects of rapid maxillary expansion in Class I, II, and III occlusions. Angle Orthod. 2011;81:298-303.
- [CrossRef] [PubMed] [Google Scholar]
- Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152-64.
- [Google Scholar]
- Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73-90.
- [Google Scholar]
- Anatomical changes induced by splitting of the midpalatal suture. Angle Orthod. 1969;39:126-32.
- [Google Scholar]
- Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41-66.
- [CrossRef] [Google Scholar]
- Midpalatal suture opening: A normative study. Am J Orthod. 1977;71:367-81.
- [CrossRef] [Google Scholar]
- Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569-75.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of rapid palatal expansion on the sagittal and vertical dimensions of the maxilla: A study on cephalograms derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:398-403.
- [CrossRef] [PubMed] [Google Scholar]
- Three dimensional reliability analyses of currently used methods for assessment of sagittal jaw discrepancy. J Clin Exp Dent. 2018;10:e352-60.
- [CrossRef] [PubMed] [Google Scholar]
- Temporomandibular joint measurements in normal occlusion: A three-dimensional cone beam computed tomography analysis. J World Fed Orthod. 2014;3:155-62.
- [CrossRef] [Google Scholar]
- Three-dimensional assessment of asymmetric mid-palatal suture expansion assisted by a customized microimplant-supported rapid palatal expander in non-growing patients: Uncontrolled clinical trial. Orthod Craniofac Res 2021:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofac Orthop. 2013;144:759-69.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Three Methods to Analyze the Skeletal Transverse Dimension in Orthodontic Diagnosis [Thesis] United States: University of Pennsylvania; 2010.
- [Google Scholar]
- Periodontal rationale for transverse skeletal normalization. Orthod Pract. 2014;5:50-3.
- [Google Scholar]
- Three-dimensional morphological and positional analysis of the temporomandibular joint in adults with posterior crossbite: A cross-sectional comparative study. J Oral Rehabil. 2021;48:666-77.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of monocortical and bicortical mini-implant anchorage on bone-borne palatal expansion using finite element analysis. Am J Orthod Dentofacial Orthop. 2017;151:887-97.
- [CrossRef] [PubMed] [Google Scholar]
- Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005;34:369-75.
- [CrossRef] [PubMed] [Google Scholar]
- Fast three-dimensional superimposition of cone beam computed tomography for orthopaedics and orthognathic surgery evaluation. Int J Oral Maxillofac Surg. 2015;44:1188-96.
- [CrossRef] [PubMed] [Google Scholar]
- An assessment of the maxilla after rapid maxillary expansion using cone beam computed tomography in growing children In: Dent Press J Orthod. Vol 19. 2014. p. :26-35.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977;72:42-52.
- [CrossRef] [Google Scholar]
- Midfacial changes in the coronal plane induced by microimplant-supported skeletal expander, studied with cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2018;154:337-45.
- [CrossRef] [PubMed] [Google Scholar]
- Tomographic assessment of palatal suture opening pattern and pterygopalatine suture disarticulation in the axial plane after midfacial skeletal expansion. Prog Orthod. 2020;21:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanics of rapid maxillary sutural expansion. Am J Orthod Dentofacial Orthop. 2000;118:257-61.
- [CrossRef] [PubMed] [Google Scholar]
- An assessment of the magnitude, parallelism, and asymmetry of micro-implant-assisted rapid maxillary expansion in non-growing patients. Prog Orthod. 2020;21:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Differential treatment effects of two anchorage systems for rapid maxillary expansion: A retrospective cephalometric study. J Orofac Orthop. 2016;77:314-24.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal expansion: Just the beginning of dentofacial orthopedics. Am J Orthod. 1970;57:219-55.
- [CrossRef] [Google Scholar]
- Rapid maxillary expansion in the primary and mixed dentitions: A cephalometric evaluation. Am J Orthod Dentofacial Orthop. 1991;100:171-9.
- [CrossRef] [Google Scholar]
- Cranioskeletal displacements caused by rapid palatal expansion in the rhesus monkey. Am J Orthod. 1971;59:146-55.
- [CrossRef] [Google Scholar]
- Changes in occlusal relationships in mixed dentition patients treated with rapid maxillary expansion. A prospective clinical study. Angle orthod. 2010;80:230-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid palatal expansion for spontaneous Class II correction. Am J Orthod Dentofacial Orthop. 2010;137:310-5.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of changing various parameters in miniscrew-assisted rapid palatal expansion: A three-dimensional finite element analysis. Korean J Orthod. 2019;49:150-60.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal and vertical effects of transverse sagittal maxillary expander (TSME) in three different malocclusion groups. Prog Orthod. 2015;16:6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of a modified acrylic bonded rapid maxillary expansion appliance and vertical chin cap on dentofacial structures. Angle Orthod. 2002;72:61-71.
- [Google Scholar]






