Translate this page into:
Orthodontic management of a periodontally compromised dentition
Address for Correspondence: Dr. Prashant K. Zaveri, Zaveri Orthodontic and Periodontic Centre, Ascot Office Park, Unit GC, 95 Ascot Avenue, Remuera, Auckland, New Zealand. E-mail: prashant@zaveriortho.co.nz
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Zaveri PK. Orthodontic management of a periodontally compromised dentition. APOS Trends Orthod 2016;6:31-8.
Abstract
Malocclusion superimposed with severe periodontitis may present a great challenge to clinicians while providing orthodontic treatment due the episodic and site-specific nature of the disease with risk of rapid tissue breakdown. However, orthodontic treatment in such situation may contribute significantly to the overall rehabilitation both functionally and esthetically. In this article, a case report outlines a combined periodontic-orthodontic management of compromised dentition. A 37-year-old female patient with significant medical history was treated for Class II Division 1 type of malocclusion associated with spaced upper and lower anterior teeth, deep overbite, and increased overjet, superimposed with chronic generalized periodontitis and bone loss. Treatment was completed using temporary anchorage devices assisted strategically applied force and modified tandem retraction biomechanics amidst management of acute inflammatory episodes during and mucogingival complication after treatment. Affected areas healed very well after post-orthodontic periodontal treatment with minimal pocket depth, and bleeding on probing, and a healthy zone of attached gingiva at the follow up visits. The orthodontic results lead to improvement in patient’s facial profile, lip posture, and correction of protrusion which addressed her main concern. One year follow-up shows good orthodontic and periodontic stability. The report highlights the importance of identifying “at risk” individuals and continuous monitoring of disease status during treatment. Despite all precautionary measures, a flare-up during the treatment can be anticipated.
Keywords
Alveolar bone levels
frenectomy
intrusion mechanics
light forces
periodontally compromised dentition
stability
supportive periodontal therapy
temporary anchorage devices
INTRODUCTION
Periodontitis is an inflammatory disease associated with a bacterial infection.[1] The rate of development and the degree of clinical inflammatory response is variable between individuals, even under similar plaque accumulation conditions.[2] Multiple risk factors may play a role in enhancing the destructive effects such as genetic, environmental, and host immune factors, especially in the “at risk” group.[3]
Ngom et al.[4] found significant correlations and suggested that malocclusions are risk markers for periodontal diseases. Tooth malalignment predisposes to plaque accumulation and leads to persistent gingival inflammation.[5]
Many studies have shown that teeth with a reduced but healthy periodontium can be moved without further attachment loss. On the other hand, inflammatory periodontal destruction is accelerated by a combination of plaque-infected teeth and orthodontic force.[6]
CASE REPORT
A 37-year-old female patient presented at our surgery concerned about protrusion of upper teeth. She was a nonsmoker and had significant medical history. Diagnostic records revealed Class II Division 1 type of malocclusion superimposed with chronic generalized periodontitis with bone loss, deep (4–7 mm) pockets, Grade I–II mobility in anterior teeth, bleeding on probing (BOP), and recession on certain teeth [Tables 1 and 2, Figure 1C, D, E and F].

- The patient’s initial condition. Extraoral photos. (a) Right profile nonsmiling. (b) Frontal. (c) Frontal smiling

- Intraoral photos buccal view. (a) Right lateral. (b) Frontal. (c) Left lateral. (d) Upper occlusal. (e) Lower occlusal

- Intraoral photos lingual view; note the advanced signs of periodontitis. (a) Right palatal. (b) Upper anterior lingual. (c) Upper left palatal. (d) Lower right lingual. (e) Lower anterior lingual. (f) Lower left lingual

- Pretreatment - periodontal charting

- Pretreatment lateral cephalogram

- Pretreatment orthopantomogram; note the bone loss
| Class II division pattern of malocclusion; deep anterior overbite; collapse of arches; protrusion of teeth; relapse of incomplete orthodontic treatment Superimposed chronic generalized periodontitis with significant bone loss Significant medical history: Hashimoto’s disease; high blood pressure; heart murmur; anemia; allergic to Maxalon and Stemetil Nonsmoker Stressful routine of life (work, home) |
| Generalized chronic periodontitis with deep pockets in many areas (deepest 7-8 mm in molar region) BOP most areas, especially lingual and palatal sides Furcation involvement in all first molars Grade I-II Mobility: Grade I on teeth 17, 16, 15, 11, 21, 25, 27, 32, 35, 37, and 42; Grade II - 31 and 41 |
Extraoral findings included mild facial asymmetry, protruding incisors, and convex profile [Figure 1A]. Intraoral findings showed relapsed or incomplete previous orthodontic treatment, anterior spacing, and proclined upper and lower incisors; increased overjet and deep overbite [Figure 1B].
Treatment objectives
Periodontal: To eradicate inflammation, reduce pocket depths, improve underlying bone condition, and establish stability
Orthodontic: To retract upper and lower anterior teeth, distalize upper arch, align, and establish occlusion.
Treatment alternatives
One option proposed to the patient was exclusive restorative or prosthodontic treatment. This would entail heavy reduction of tooth tissue or extraction of teeth. In addition, it could possibly incur higher costs. Alternatively, only periodontal treatment and maintenance were suggested. This was not suitable for the patient as it did not address her main concern. Patient agreed to the orthodontic treatment plan with full awareness that long-term maintenance was important to achieve stable results.
Treatment progress
Pre-orthodontic phase
Periodontal treatment involved deep scaling, root planning, and subgingival curettage. A protocol for supportive periodontal treatment was established (3 × 12 monthly S and C with oral hygiene instructions) [Figure 2].

- Postperiodontal treatment. Intraoral buccal view. (a) Frontal. (b) Right lateral. (c) Left Lateral

- Intraoral lingual view. (a) Lower left lingual. (b) Upper left palatal. (c) Lower right lingual. (d) Upper right palatal. (e) Upper anterior occlusal. (f) Lower occlusal. (g) Upper occlusal

- Charting after periodontal treatment
Orthodontic phase
Following 3 months of periodontal therapy, orthodontic treatment was initiated with a 022 MBT appliance and 0.16 heat activated (HA) nickel-titanium (NiTi) archwires. After 20 weeks, rectangular 19 × 25 HA NiTi archwires were placed for further alignment and leveling. Initial space closure with carried out with rectangular stainless steel (SS) wires with loops [Figure 3].

- Progress of orthodontic treatment. Intraoral buccal views. (a) Right lateral. (b) Frontal. (c) Left lateral. (d) Upper occlusal. (e) Lower occlusal

- Intraoral lingual views - note the plaque disclosing solution used for patient motivation and education. (a) Upper anterior lingual . (b) Upper right palatal. (c) Upper left palatal. (d) Lower anterior lingual. (e) Lower right lingual. (f) Lower left lingual

- Progress periodontal charting - note the acute condition on tooth 32 lingual

- Intraoral periapical X-rays lower anterior and 32 region. (a) Intraoral periapical - bone levels in 32 regions. (b) Lower anterior bone levels

- Progress treatment orthopantomogram - note levelling of occlusal plane and alveolar bone level

- Progress orthopantomogram showing temporary anchorage device assisted retraction and anterior torquing

- Intraoral buccal views; note modified tandem mechanics with auxiliary archwire for retraction and root torque control
Temporary anchorage devices (TADs) (SH 1312-07; Dentos) were placed in the posterior region on each side for further spaces closure and distalization. Upper premolars were extracted for periodontal reason. Modified biomechanics was applied to control force levels and root control [Figure 3G and F]. Finishing and detailing were done with 19 × 25 SS wires and after debond upper and lower fixed lingual retainers were placed in tandem with Essix retainer at night [Figure 4]. The patient has been on supportive periodontal therapy (SPT) and orthodontic retention check since completion. Treatment was controlled by small units of activations to achieve desired changes. However, it was prolonged due to acute episodic flare up with inflammation at certain sites, with several occasions where treatment had to be stopped and periodontal control established [Figure 3C and D]. Lower anterior mucogingival complication had to be dealt with by a frenectomy [Figure 5]. One year posttreatment showed good stability [Figure 6].

- Posttreatment records. Posttreatment extraoral view. (a) Frontal nonsmiling. (b) Frontal smiling. (c) Right profile nonsmiling

- Intraoral buccal view. (a) Right lateral. (b) Frontal. (c) Left lateral. (d) Upper occlusal. (e) Lower occlusal

- Intraoral lingual view. (a) Upper left palatal. (b) Anterior upper occlusal. (c) Upper right palatal. (d) Lower right lingual. (e) Anterior lower occlusal. (f) Lower left lingual

- (a) Posttreatment lateral cephalogram. (b) Posttreatment orthopantomogram

- Cranial base and profile superimposition. Black pre treatment and Green post treatment
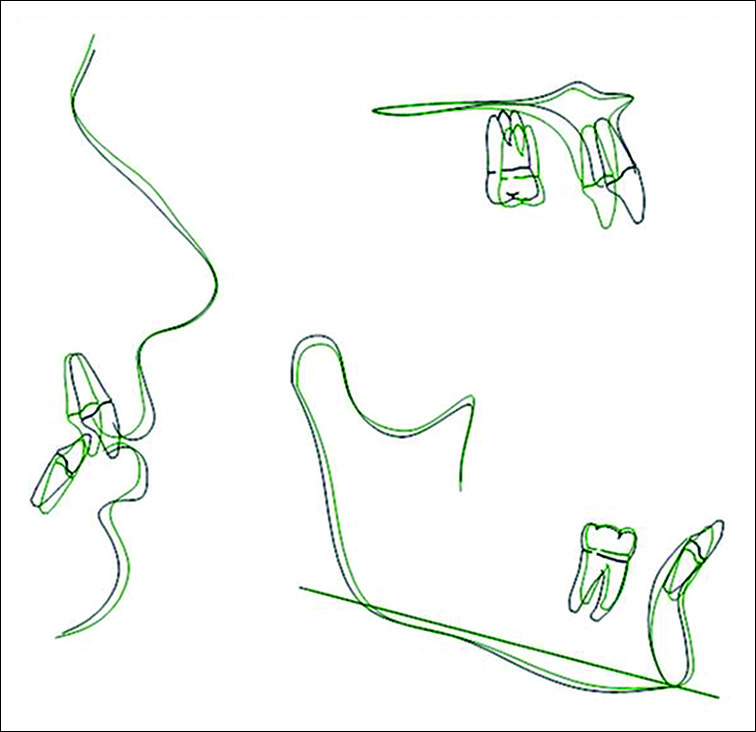
- Superimposition of post treatment changes profile, maxilla and mandible. Black pre treatment and Green post treatment

- (a) Laser-assisted correction of mucogingival complication. High frenal attachment with tension test positive inducing detachment and bone loss; (b) Laser-assisted surgical correction; (c) Laser- assisted surgical correction suturing of alveolar mucosa; (d) One-year posttreatment healing - note the stable zone of attached gingiva

- One-year posttreatment records. Extraoral photographs. (a) Frontal smiling. (b) Frontal nonsmiling. (c) Right lateral

- Intraoral buccal views. (a) Right buccal. (b) Frontal. (c) Left buccal. (d) Upper occlusal. (e) Lower occlusal

- Intraoral lingual views. (a) Right upper posterior sextant - palatal. (b) Upper occlusal - anterior sextant. (c) Left upper posterior sextant - palatal. (d) Right lower posterior sextant - lingual. (e) Lower occlusal - anterior sextant. (f) Left lower posterior sextant - lingual

- One-year posttreatment lateral cephalogram

- One-year posttreatment orthopantomogram
Acute episodes
Acute inflammatory episodes were experienced during treatment [Figure 3B-D]. An example displaying the high susceptibility can be seen in 32 region, a large swelling 3 mm × 7 mm × 2 mm appeared between adjustment visits. Following a 2% chlorhexidine solution flush, the patient has advised a course of antibiotics. Deep scaling and/or root planning (SRP) was carried out 3 days later.
Treatment results
The orthodontic results lead to improvement in patient’s facial profile, lip posture, and correction of protrusion which addressed her main concern. Overjet and overbite were within normal range. Cephalometric values showed good dentoalveolar changes [Table 3]. However, upper anterior could have been torqued further. Lower anterior were held relatively stable during treatment. TAD-assisted biomechanics helped control occlusal plane, intrusion of upper anterior and lip posture. Periodontal health control was very challenging with acute inflammatory episodes during treatment. Affected areas healed very well after periodontal treatment with minimal pocket depth, BOP, and healthy zone of attached gingiva at the follow-up visit. Several breaks during treatment did not affect the ultimate outcome and long-term stability. The patient was satisfied with results [Figure 7]. Mucogingival complication was treated 3 months after debond with a frenectomy. One year follow-up shows good orthodontic and periodontic stability.
| Pretreatment value | Posttreatment value | Norm | SD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SNA (°) | 89.2 | 89.2 | 82 | 3.5 | |||||||||
| SNB (°) | 79.6 | 80.1 | 80.9 | 3.4 | |||||||||
| ANB (°) | 9.6 | 9.1 | 1.6 | 1.5 | |||||||||
| SND (°) | 78.4 | 78.6 | 80 | 3 | |||||||||
| U1 -NA (mm) | 1.5 | −3.6 | 4.3 | 2.7 | |||||||||
| U1 -NA (°) | 12.3 | 2.6 | 22.8 | 5.7 | |||||||||
| L1 -NB (mm) | 8.4 | 5.7 | 4 | 1.8 | |||||||||
| L1 -NB (°) | 37.3 | 28.9 | 25. | 3 6 | |||||||||
| Pog -NB (mm) | 2.1 | 1.8 | 2.4 | 1.7 | |||||||||
| Po and L1 -NB difference (mm) | 6.3 | 3.9 | 2.6 | 1.7 | |||||||||
| Interincisal angle (U1-L1) (º) | 120.7 | 139.5 | 130 | 6 | |||||||||
| Occ plane to SN (°) | 12.4 | 16.9 | 14.4 | 2.5 | |||||||||
| SN -GoGn (°) | 21.4 | 23.2 | 32.9 | 5.2 | |||||||||
| S-L (mm) | 54.1 | 53.9 | 51 | 3 | |||||||||
| S-E (mm) | 15.7 | 13.9 | 22 | 3 | |||||||||
| FMA (MP-FH) (°) | 17 | 18.6 | 23.9 | 4.5 | |||||||||
| IMPA (L1-MP) (°) | 114.1 | 103.4 | 95 | 7 | |||||||||
| FMIA (L1-FH) (°) | 48.9 | 58 | 64.8 | 8.5 | |||||||||
| Y-axis (SGn-SN) (°) | 61.6 | 62.1 | 67 | 5.5 | |||||||||
| U1 -SN (°) | 101.5 | 91.7 | 102.8 | 5.5 | |||||||||
| L1 protrusion | 2 | −0.4 | 2.7 | 1.7 | |||||||||
| (L1-APo) (mm) | |||||||||||||
| Y-axis length (mm) | 111.5 | 113.1 | 131 | 6 | |||||||||
| Upper lip to E-plane (mm) | −3.5 | −7.5 | −6 | 2 | |||||||||
| Lower lip to E-plane (mm) | 0 | −3.5 | −2 | 2 | |||||||||
| Wits appraisal (mm) | 7.6 | 4.9 | −1 | 1 | |||||||||
| U1 -FH (°) | 108.2 | 98.5 | 111 | 6 | |||||||||
| LFH (ANS-Me || FH) (%) | 53.5 | 54.1 | 54 | 5 | |||||||||
| UFH (Na-ANS) (%) | 46.5 | 45.9 | 46 | 5 | |||||||||
SD – Standard deviation

- (a) Treatment comparison. Pretreatment three-quarter smiling; (b) Posttreatment three-quarter smiling; (c) One year posttreatment three-quarter smiling
DISCUSSION
Advanced disease progression at a young age of our patient could suggest acute episodes with aggressive form of the disease, a genetic predisposition (family history), ethnicity (Promsudthi et al. 2005), stress (Peruzzo et al. 2007), or poorly aligned teeth as possible contributory factors for her condition (Nunn 2003).[7]
By virtue of past history, screening, and evaluation of her condition, the sequence of treatment was initiated with thorough professional SRP .[8,9] The first objective was to stabilize the condition with emphasis on reducing marginal inflammation and improving hygiene conditions.[6] Orthodontic treatment objective was to level the alveolar bone with tooth movement – which was successfully achieved (Lindhe 2008).
Even though the patient showed good commitment by consistently maintaining excellent supragingival plaque control, she had a few acute flare-ups at certain sites. For example, BOP, at 18 months, only at 8 probing sites (mainly on 2 teeth) with 5 mm pocket in 32 lingual and 16 mesio-lingual region is a reflection of site specific and episodic nature of disease. This often obliterates the distinction between chronic and aggressive forms of the disease.[10,11]
It has been suggested that if the patient fails to maintain high level of oral hygiene, aggravation of the disease occurs or if the patient’s oral hygiene deteriorates; orthodontic therapy has to be stopped to ensure a reasonable risk/benefit ratio.[6] This became necessary at certain times during treatment. However, our protocol of continuous monitoring and assessment of periodontal condition, adequate SPT and periodic reinforcement of oral hygiene instructions, and motivation[12] helped us to manage the acute flare-ups during the treatment. The increased duration of treatment did not adversely affect the outcome.
Previous studies have clearly demonstrated that fixed orthodontic appliances and elastomeric rings increase plaque accumulation and gingival inflammation. Molar bands were avoided and steel ligature ties utilized most times to minimize and manage the ecology of plaque. Meticulous plaque removal in all hygiene-critical areas; bracket periphery, and interproximal and gingival tooth surfaces was carried out periodically.
Limiting factors in dealing with periodontally affected teeth include loss of anchorage and reduction of bone support/ attachment, induced by uncontrolled force systems. Due to reduced bone support and Grade II–III mobility on 15, upper premolars were extracted midtreatment. We endeavored to place the line of force closer to the center of resistance to reduce the tendency for teeth to tip.[13] Our results showed good intrusion and leveling along with distalization. However, the palatal root torque on upper anterior was less than desirable. This may be due to not allowing enough time for palatal root movement to take place even though the force vector was applied linear to TAD on both sides.
Controlled intrusion and retraction of teeth was achieved by focusing on indirect anchorage from TADs and smaller units of activation and movements. This allowed preservation of crestal alveolar bone levels.
It has been suggested the orthodontic correction of malocclusion would help periodontal stability and function.[7] It is evident that the treatment has improved bony architecture and occlusal relationship. The prognosis is good; however, the challenge would be to maintain these favorable tissue responses through years to come.
CONCLUSION
Diagnosis of active phases of periodontal disease represents challenges for clinical practitioners.[14] Hence, complex cases should be co-evaluated by the periodontist and the orthodontist. Orthodontic treatment in a high-risk patient with periodontally compromised dentition was carried out. Result showed significant improvement of functional status, esthetic balance, and periodontal health with long-term stability. The importance of a regimented oral hygiene program before and during orthodontic treatment has been emphasized. Despite all precautionary measures, a flare up during the treatment can be anticipated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Modulation of clinical expression of plaque-induced gingivitis. I. Background review and rationale. J Clin Periodontol. 2004;31:229-38.
- [Google Scholar]
- Environmental and other modifying factors of the periodontal diseases. Periodontol 2000. 2006;40:107-19.
- [Google Scholar]
- Influence of orthodontic anomalies on periodontal condition. Odontostomatol Trop. 2007;30:9-16.
- [Google Scholar]
- Effects of malalignment of teeth in the anterior segments on plaque accumulation. J Clin Periodontol. 1981;8:481-90.
- [Google Scholar]
- Interrelationship between periodontics and adult orthodontics. Periodontology 2000. 2004;1:143-9.
- [Google Scholar]
- Effects of malocclusions and orthodontics on periodontal health: Evidence from a systematic review. J Dent Educ. 2008;72:912-8.
- [Google Scholar]
- A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):55-71.
- [Google Scholar]
- Microbiological profile of early onset/aggressive periodontitis patients. Oral Microbiol Immunol. 2004;19:314-21.
- [Google Scholar]
- Genetic and environmental risk factors for chronic periodontitis and aggressive periodontitis. Periodontol 2000. 2010;53:138-53.
- [Google Scholar]
- Mechanical principles in orthodontic force control. In: Proffit WR, Fields HW Jr., Sarver DM, editors. Contemporary Orthodontics. St. Louis, Missouri: Elsevier Health Sciences; 2014.
- Etiology and pathogenesis of periodontal diseases. Dent Clin North Am. 2005;49:491-516.
- [Google Scholar]






