Translate this page into:
Multidisciplinary orthodontic-orthognathic management of severe skeletal Class III malocclusion and anterior open bite

*Corresponding author: Nguyen Viet Anh, Private Practice, Viet Anh Orthodontic Clinic, Nam Tu Liem, Hanoi, Vietnam. bsvietanhniengrang@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Son T, Anh N, Ninh D. Multidisciplinary orthodontic-orthognathic management of severe skeletal Class III malocclusion and anterior open bite. APOS Trends Orthod, doi: 10.25259/APOS_78_2023
Abstract
This case report presents the multidisciplinary management of a patient with severe skeletal Class III malocclusion, anterior open bite, dentigerous cyst, and multiple restorations. The patient underwent orthodonticorthognathic treatment, autotransplantation, cyst removal, and esthetic rehabilitation with porcelain veneers. The presurgical orthodontic decompensation of the proclined upper incisors involved mini-screw-assisted entire upper arch distalization. The bimaxillary osteotomy included advancing the maxilla, mandibular setback, rotating the maxillomandibular complex clockwise, and moving the chin posteriorly. The role of multidisciplinary treatment is very important in orthognathic patients with compromised dentition. Autotransplantation could help patients avoid the need for prosthetic implants. Entire arch distalization could be a possible alternative to premolar extraction for presurgical orthodontic decompensation in cases of proclined incisors.
Keywords
Anterior open bite
Skeletal Class III malocclusion
Multidisciplinary treatment
Bimaxillary osteotomy
Tooth autotransplantation
INTRODUCTION
Skeletal Class III malocclusion in hyperdivergent patients is usually associated with anterior open bite and may pose many difficulties for the orthodontist.[1,2] Cases of mild to moderate severity might be possible to be treated with camouflage orthodontics alone, but severe cases usually require orthognathic surgery with a mandibular setback or bimaxillary osteotomy.[3,4] Presurgical orthodontic decompensation is usually done with maxillary premolar extraction to upright proclined upper incisors in surgical cases.[5]
This case report presents the multidisciplinary management of a severe skeletal Class III patient with anterior open bite, dentigerous cyst, and multiple restorations with orthodonticorthognathic treatment, autotransplantation, cyst removal, and esthetic rehabilitation with porcelain veneers.
CASE REPORT
A 20-year-old female patient presented to our clinic with chief complaints of anterior open bite and prognathic mandible. On the extraoral examination, she had a concave profile, a long face, and a protruded and left deviated chin. The smile esthetics was compromised due to the open bite and a reduced incisal display. No sign of temporomandibular joint disorder was detected [Figure 1]. On the intraoral examination, the patient had a severe Class III canine and molar relationship with anterior open bite, missing mandibular left first molar, heavily restored mandibular right first molar, and multiple restorations on maxillary teeth. A large interdental space existed between the mandibular right first and second premolars, which might be caused by a low position of the tongue or a buccal frenum attachment. Her lower dental midline deviated 1.5 mm to the left side.

- Pre-treatment facial and intraoral photographs.
On the lateral cephalometric examination, the patient had a severe skeletal Class III relationship (A point, nasion, B point [ANB], −5.8°) with a prognathic mandible (sella nasion point B [SNB], 85.1°) and hyperdivergent facial pattern (Frankfort mandibular plane angle, 29.3°) [Table 1]. The upper incisors were proclined (U1-SN, 111.5°) and the lower incisors were retroclined (incisor mandibular plane angle (IMPA), 74.3°). The decreased upper incisal display of −0.9 mm was confirmed and both lips were behind the E line. The panoramic radiograph showed a dentigerous cyst of the maxillary left third molar, and a severe endodonticperiodontal lesion of the mandibular right first molar [Figure 2].
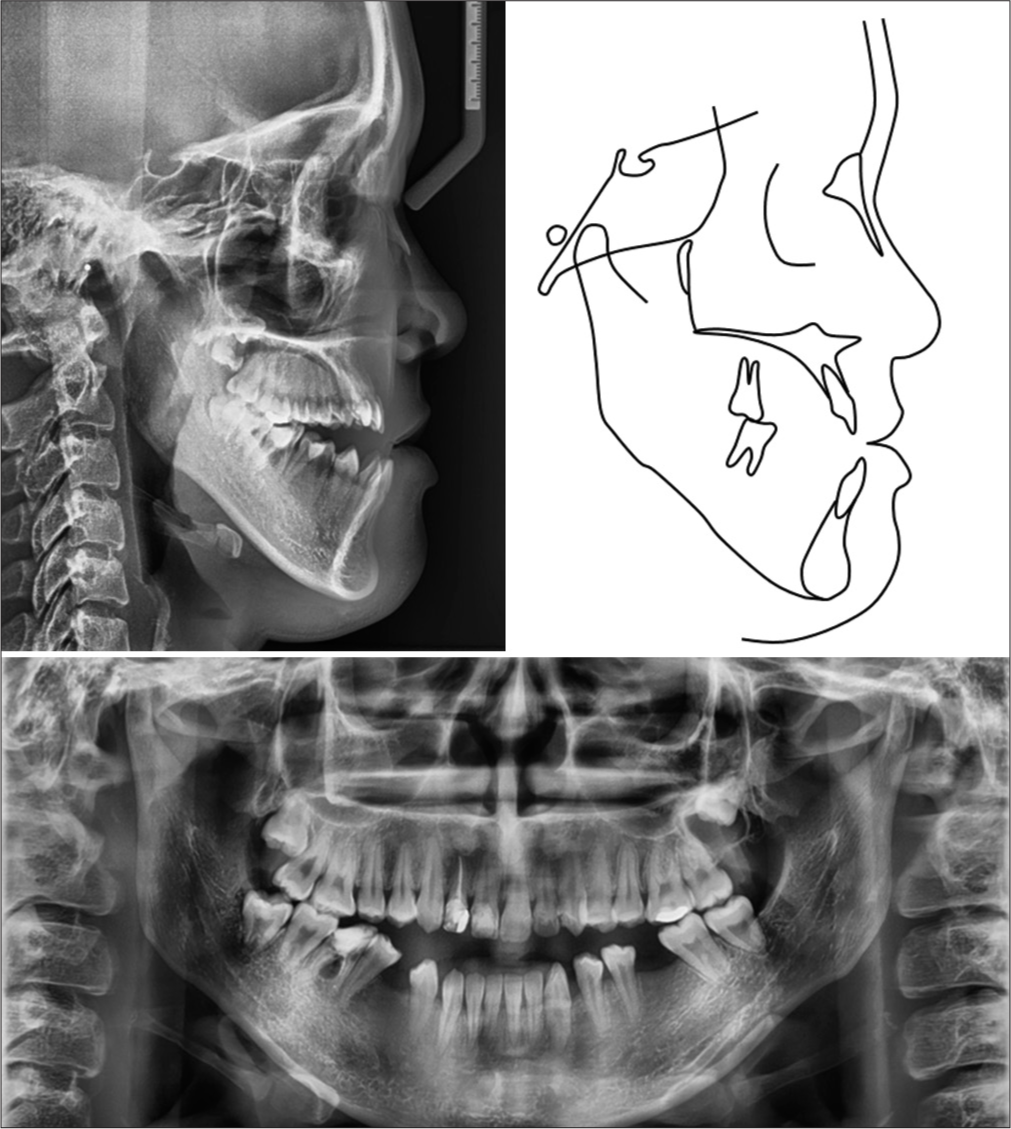
- Pre-treatment radiographs and tracing.
| Pre-treatment | Pre-surgery | Post-treatment | Norm | |
|---|---|---|---|---|
| Skeletal | ||||
| SNA (°) | 79.3 | 79.4 | 82.3 | 81.1±3.7 |
| SNB (°) | 85.1 | 83.5 | 82.3 | 79.2±3.8 |
| ANB (°) | −5.8 | −4.1 | 0.0 | 2.5±1.8 |
| FMA (°) | 29.3 | 29.1 | 30.6 | 25.0±4.0 |
| Dental | ||||
| U1-SN (°) | 111.5 | 99.8 | 101.9 | 105.3±6.6 |
| U1-NA (°) | 32.1 | 20.5 | 19.8 | 22.0±5.0 |
| U1-NA (mm) | 8.8 | 4.9 | 4.5 | 4.0±3.0 |
| IMPA (°) | 74.3 | 70.5 | 72.6 | 90.0±3.5 |
| L1-NB (°) | 19.2 | 14.3 | 15.9 | 25.0±5.0 |
| L1-NB (mm) | 4.3 | 1.7 | 1.6 | 4.0±2.0 |
| U1-L1 (°) | 134.4 | 144.0 | 144.6 | 128.0±5.3 |
| U1 display | −0.9 | 0.9 | 1.1 | 2.5±1.5 |
| Soft tissue | ||||
| E-line/UL (mm) | −6.4 | −6.2 | −2.8 | 0.0±2.0 |
| E-line/LL (mm) | −1.3 | −2.2 | −2.6 | 0.0±2.0 |
ANB: A point, nasion, B point, FMA: Frankfort mandibular plane angle, IMPA: Incisor mandibular plane angle, L1: Lower central incisor, LL: Lower lip, MP: Mandibular plane, NA: Nasion point A NB: Nasion point B, SNA: Sella nasion point A, SNB: Sella nasion point B, U1: Upper central incisor, UL: Upper lip, E-line: Riketts
Treatment objectives
The orthodontic treatment objectives included improving the Class III skeletal and dental relationship, closure of the anterior open bite, correction of chin deviation, improving the concave profile, and increasing the upper incisal display. The multidisciplinary treatment objectives included removing the dentigerous cyst, replacement of the missing and hopeless mandibular first molars, and improving the esthetics of the poorly restored upper anterior teeth in the patient.
Treatment alternatives
Considering the severity of skeletal Class III malocclusion and anterior open bite, an orthodontic-orthognathic treatment plan was selected. The presurgical orthodontic phase included space management in the lower arch and decompensation of the proclined upper incisors. The orthognathic surgery consisted of LeFort I osteotomy and a bilateral sagittal split osteotomy to advance the maxilla, setback the mandible, rotate the maxillomandibular complex clockwise, and move the chin posteriorly.
Treatment progress
The orthodontic treatment was started by bonding all teeth with 0.022 × 0.028-inch pre-adjusted brackets (OK Bracket, Jaintek, South Korea). The archwire sequence was 0.014-inch, 0.016-inch, 0.016 × 0.022-inch, 0.019 × 0.025-inch nickel-titanium, and 0.019 × 0.025-inch stainless steel. After 1 month of treatment, the patient was referred to a maxillofacial surgeon for dentigerous cyst removal, and autotransplantation of the mandibular right third molar to the mandibular right first molar position. After the leveling and alignment stage, the decompensation of the proclined upper incisors was done by en masse distalization of the entire maxillary arch using palatal mini-screw anchorage [Figure 3]. The mandibular left first molar extraction space was opened using open coil springs and all other spaces in the lower arch were closed on a pre-torqued 0.019 × 0.025-inch stainless steel archwire. Throughout the orthodontic treatment, the patient was educated to position the tongue properly to facilitate space closure in the lower arch. The presurgical orthodontic phase was completed in 10 months with an improvement in the anterior open bite and normal inclination of the upper incisors (U1-SN, 99.8°) [Figure 4].

- Entire upper arch distalization with mini-screw anchorage to decompensate proclined incisors.
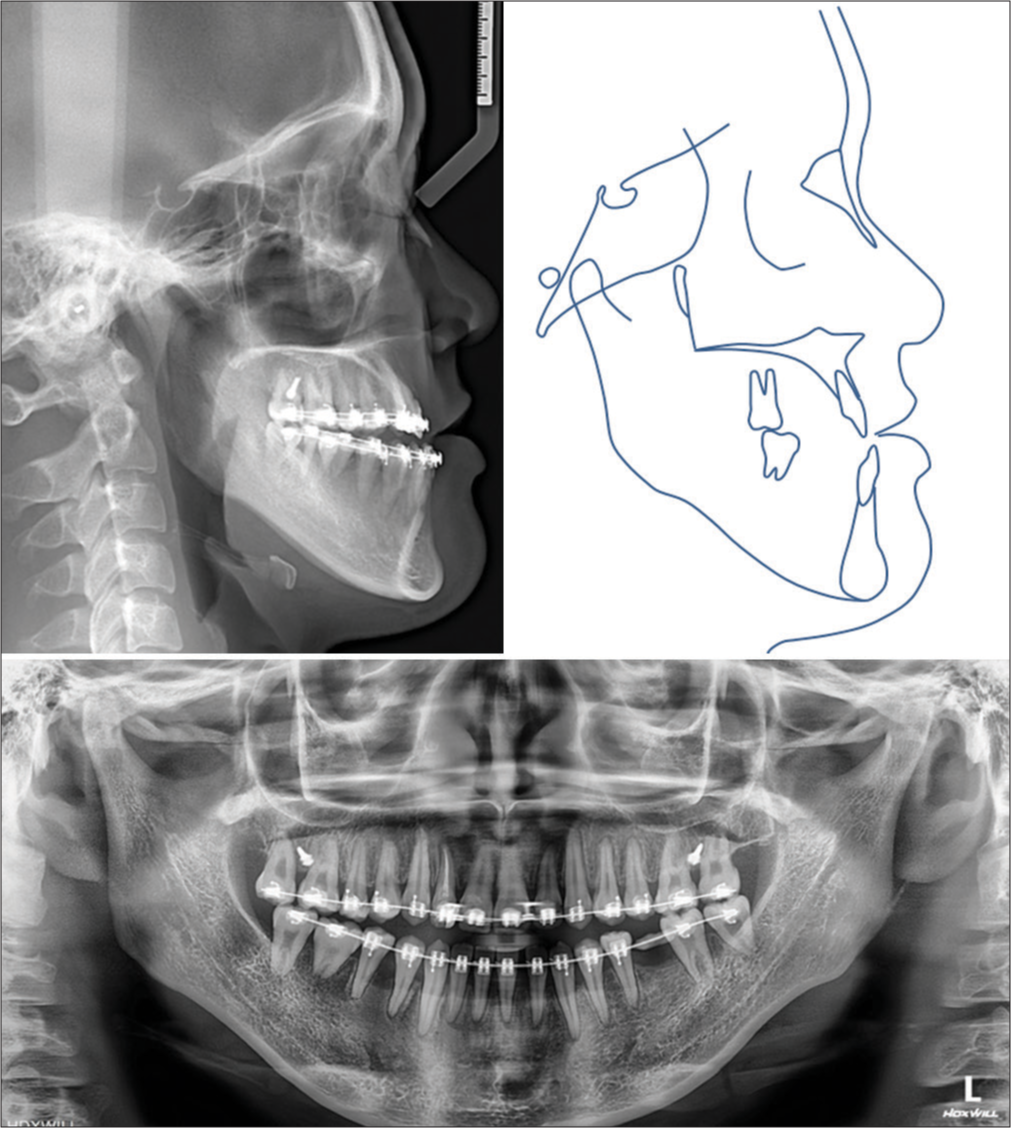
- Presurgical radiographs and tracing.
After 11 months of treatment, a digital impression and a cone-beam computed technology (CBCT) were taken to plan for the orthognathic surgery. All the data were imported into a virtual planning software (Proplan CMF, Materialise, Leuven, Belgium) and a bimaxillary osteotomy was planned. The maxilla was advanced by 2 mm and rotated clockwise by 1° with slight anterior intrusion and posterior impaction. The mandible was set back by 6.3 mm, and a genioplasty was performed to move the chin backward by 1.3 mm and upward by 2.2 mm [Figure 5]. Surgical splints were designed and printed with a high-resolution 3-dimensional printer (Sonic Mini 4K, Phrozen, Hsinchu, Taiwan), and a surgical guide resin (Surgical Guide 3, SprintRay, CA, USA) for high accuracy.[6] The orthognathic surgery was performed under general anesthesia, and the intermaxillary fixation was removed immediately post-surgery.

- Virtual orthognathic surgery plan.
The postsurgical orthodontic phase was initiated 2 weeks after the surgery including closing the remaining spaces and finalizing the occlusion. A slight Class II malocclusion developed postsurgically, so the entire upper arch distalization was continued and Class II elastics were applied on the left side. The postsurgical orthodontic phase lasted 6 months, and the total active treatment time was 17 months.
Treatment results
The post-treatment photographs confirmed that all treatment objectives were achieved [Figure 6]. The Class I canine and molar relationship was obtained with coincided midlines and the anterior open bite was corrected. The mandibular left first molar space was adequately opened for implant restoration and all other spaces were completely closed. The prognathic mandible and concave profile were improved.
The lateral cephalometric analysis confirmed the improvement of the skeletal Class III relationship (ANB, 0.0°; sella nasion point A, 82.3°; SNB, 82.3°). The upper incisal proclination and display were improved (U1-SN, 101.9; U1 display, 1.1 mm), but the lower incisors were more retroclined (IMPA, 72.6°). The retruded upper lip was improved (E-line/UL, −2.8 mm). The panoramic radiograph showed adequate root parallelism and good condition of the autotransplanted tooth [Figure 7]. The general and maxillary cephalometric superimposition showed the slight extrusion of upper incisors, intrusion of upper molars, clockwise rotation of the occlusal plane, and posterior movement of the mandibular symphysis and incisors. Because the regional mandibular superimposition was based on the mandibular symphysis, the skeletal changes could be seen at the condyle and chin [Figure 8]. After bracket removal, the patient was referred to a prosthodontist for esthetic rehabilitation of the upper anterior teeth with porcelain laminate veneers. The slightly reduced overjet and overbite were favorable for minimizing the amount of enamel removal during tooth preparation.

- Post-treatment facial and intraoral photographs.
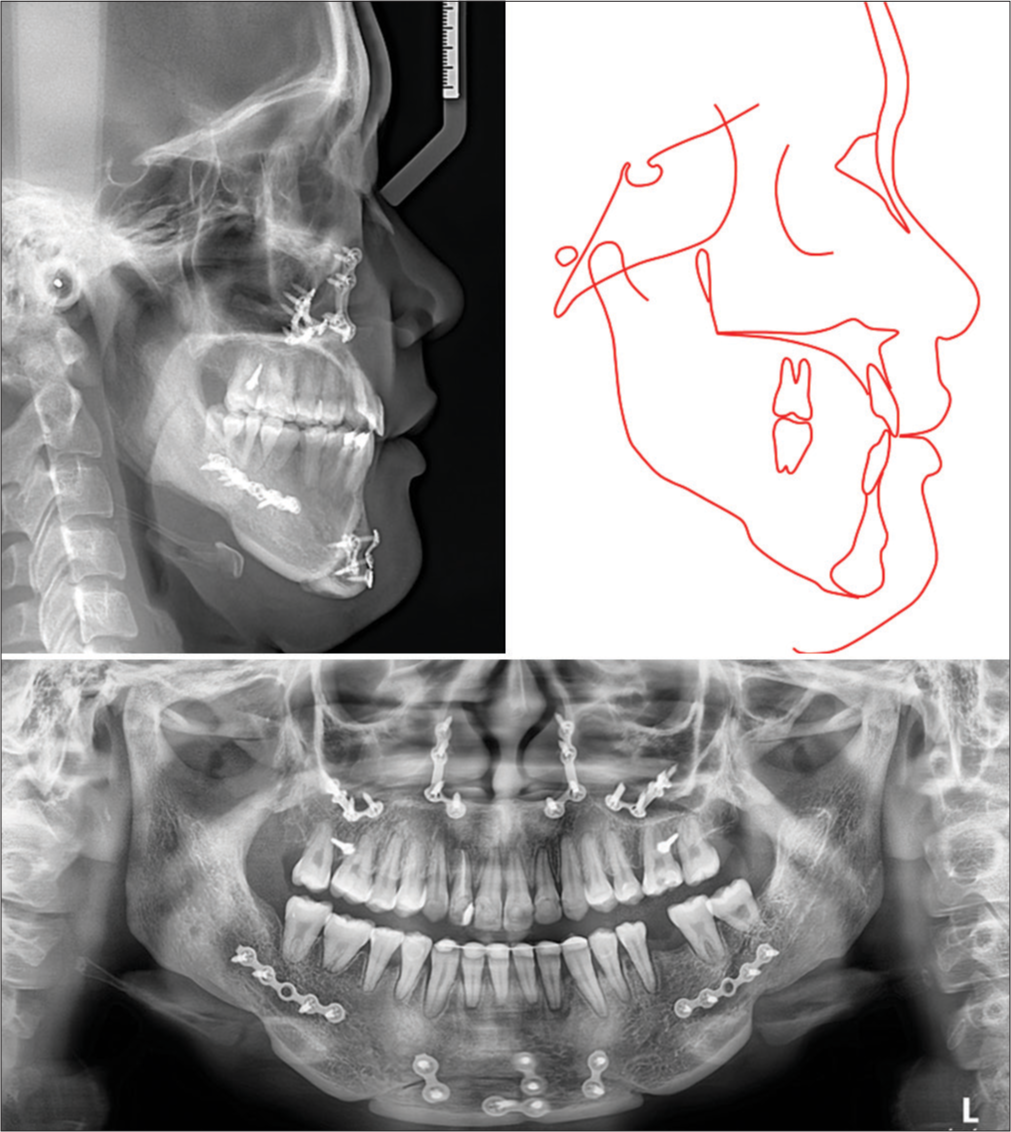
- Post-treatment radiographs and tracing.

- Overall and regional cephalometric superimpositions: Black: pre-treatment, blue: pre-surgery, red: post-treatment.
The 6-month post-retention photographs showed the treatment results to be stable [Figure 9]. The proper tongue position and the removal of buccal frenum attachment during the orthognathic surgery might have contributed to the maintenance of space closure in the lower arch.

- Six-month follow-up photographs. Upper anterior teeth were restored with porcelain laminate veneer.
DISCUSSION
In this orthodontic-orthognathic case report, the presurgical orthodontic decompensation was done with en masse retraction of the entire upper arch using skeletal anchorage without premolar extraction. Short crimpable hooks were used to apply retraction force to create a clockwise rotation of the upper arch, as the force vector passed inferiorly to the center of resistance of the entire upper arch.[7] As a result, the anterior open bite and the upper incisal display were improved after this presurgical orthodontic phase. The upper incisor inclination was reduced by 11.8° despite no premolar extraction being performed.
The palatal alveolar bone was selected for mini-screw placement in this patient, because the labial posterior alveolar bone was insufficient. The palatal inter-radicular space in the upper molar region is larger than the labial one, as the upper molars only have one palatal root so that more molar distalizing amount could be achieved without being interfered with by the mini-screws.[8]
The mandibular first molar extraction spaces were not orthodontically closed in this patient as the lower incisors were already retroclined before treatment. Instead, implant restoration and autotransplantation of the third molar were planned. Root canal treatment was not performed on the autotransplanted tooth as the apex closure had not been completed.[9] This non-closure of the apex would have facilitated the revascularization process to maintain the vitality of the transplanted tooth. Orthodontic forces were applied 4 weeks after the transplantation to allow the tooth to heal and prevent ankylosis.[10-12] The post-treatment radiograph showed good integration and root formation of the transplanted third molar without signs of replacement resorption or periodontal attachment loss.
There was a decrease in pharyngeal airway space after orthognathic surgery on cephalometric analysis due to the mandibular setback, but no sign of obstructive sleep apnea was detected during the postsurgical period. Other studies have also shown that mandibular setback osteotomy resulted in a reduction in the size of the pharyngeal airway dimensions, but it did not lead to obstructive sleep apnea.[13,14] However, it is important to consider the risk factors associated with sleep breathing disorders during orthognathic treatment planning to prevent the development of obstructive sleep apnea.
CONCLUSION
The role of multidisciplinary treatment is very important in orthognathic patients with compromised dentition. Autotransplantation could help patients avoid the need for prosthetic implants. Entire arch distalization could be a possible alternative to premolar extraction for presurgical orthodontic decompensation in cases of proclined incisors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Skeletal Class III malocclusion with lateral open bite and facial asymmetry treated with asymmetric lower molar extraction and lingual appliance: A case report. Int J Environ Res Public Health. 2021;18:5381.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontally compromised severe skeletal Class III with open bite corrected by orthodontic camouflage using temporary anchorage devices. APOS Trends Orthod. 2020;10:253-8.
- [CrossRef] [Google Scholar]
- A severe skeletal Class III malocclusion treated with Le Fort I combined with sagittal split ramus osteotomy, mandibular body ostectomy and tongue reduction surgery. A case report. APOS Trends Orthod. 2022;12:221-9.
- [CrossRef] [Google Scholar]
- Skeletal Class III malocclusion in an adult patient-orthodontics versus orthognathic surgery: Is there another alternative? APOS Trends Orthod. 2018;8:161-7.
- [CrossRef] [Google Scholar]
- Converting a bi-jaw surgery to a single-jaw surgery: Posterior maxillary dentoalveolar intrusion with microimplants to avoid the need of a maxillary surgery in the surgical management of skeletal Class III vertical malocclusion. APOS Trends Orthod. 2016;6:218-27.
- [CrossRef] [Google Scholar]
- Effect of horizontal resolution of printer on trueness of 3D-printed provisional crown: An in vitro study. Eur J Gen Dent. 2023;12:34-41.
- [CrossRef] [Google Scholar]
- Severe overjet and deep overbite correction by en masse distalization using lingual appliances and mini-implant anchorage: Two case reports. Clin Investig Orthod. 2022;81:217-28.
- [CrossRef] [Google Scholar]
- Lingual orthodontic treatment of a skeletal Class II patient with miniscrew-assisted absolute anchorage in maxillary arch and total distalization in mandibular arch: A case report. Orthod Waves. 2021;80:97-106.
- [CrossRef] [Google Scholar]
- Autotransplantation of immature third molars using a computer-aided rapid prototyping model: A report of 4 cases. J Endod. 2013;39:1461-6.
- [CrossRef] [PubMed] [Google Scholar]
- Autotransplantation of premolars to premolar sites. A long-term follow-up study of 40 consecutive patients. Am J Orthod Dentofacial Orthop. 2004;125:668-75.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term observation of autotransplanted teeth with complete root formation in orthodontic patients. Am J Orthod Dentofacial Orthop. 2010;138:720-6.
- [CrossRef] [PubMed] [Google Scholar]
- A long-term study of 370 autotransplanted premolars. Part IV. Root development subsequent to transplantation. Eur J Orthod. 1990;12:38-50.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea-a systematic review. J Craniomaxillofac Surg. 2015;43:248-53.
- [CrossRef] [PubMed] [Google Scholar]
- Multislice computed tomography assessment of airway patency changes in the supine position following mandibular setback surgery for mandibular prognathism: A prospective 1-year follow-up study. APOS Trends Orthod. 2020;11:106-15.
- [CrossRef] [Google Scholar]







