Translate this page into:
Buccal corridor and gummy smile treatment with MARPE and gingivoplasty: A 2-year follow-up case report

*Corresponding author: Viet Hoang, Department of Orthodontics and Pedodontics, Faculty of Dentistry, Van Lang University, Ho Chi Minh City, Vietnam. viet.h@vlu.edu.vn
-
Received: ,
Accepted: ,
How to cite this article: Hoang V, Tran PH, Dang TT. Buccal corridor and gummy smile treatment with MARPE and gingivoplasty: A 2-year follow-up case report. APOS Trends Orthod. doi: 10.25259/APOS_216_2023
Abstract
The advent of Mini-screws assisted rapid palatal expansion (MARPE) has introduced a simpler in-office procedure that enables the translation of the alveolar process in adults. This case report showed the combination of MARPE, orthodontic treatment, and gingivoplasty to correct malocclusion and enhance smile aesthetics. A 20-year-old woman expressed concerns about excessive buccal corridors and a gummy smile. She exhibited skeletal class I malocclusion, with buccal corridors exceeding 4 mm, a gummy smile, and lingual tipping of the lower posterior segments. The treatment plan involved utilizing the MARPE appliance, a Nitinol wire, gingivoplasty to address the gummy smile. Retention evaluations demonstrated the stability of MARPE in transversal skeletal discrepancies. There was notable improvement in incisor inclination and soft tissue profile, particularly evident in the E-line and nasolabial angle. Cephalometric analysis confirmed these changes, showing a decrease of 5.9 degrees in the inclination of the maxillary incisors. After a 2-year follow-up, the results remain stable, and the patient expresses satisfaction with the outcome. MARPE can be considered as an effective tool for managing buccal corridors, complemented by fixed orthodontic treatment employing labial appliances and gingivoplasty to correct malocclusion and enhance smile aesthetics. The treatment showed positive long-term outcomes.
Keywords
MARPE
gummy smile
gingivoplasty
expansion
mini-screws
miniscrew-assisted rapid palatal expansion
INTRODUCTION
Smiling has a significant impact on the satisfaction of individuals, it is related to skeletal, dental, and soft-tissue problems.[1] Common factors have negative impacts on the beauty of a smile, such as buccal corridor, maxillary central incisor crown width to height ratio, maxillary lateral to central incisor ratio, maxillary midline to face, maxillary to mandibular midlines, the teeth alignment, canine and posterior crown torque, incisal edge discrepancy, and maxillary gingival display.[2]
Buccal corridors as the spaces between the anterior surfaces of the posterior teeth and the corners of the lips when the patient is smiling. Having small buccal corridors is considered an attractive characteristic for both males and females. Significant buccal corridors should be identified as an issue during the diagnosis and planning stages of orthodontic treatment.[3,4] Significant buccal corridors in adult patients were commonly addressed through orthognathic surgery or surgically assisted rapid palatal expansion.[5-7] However, the inherent surgery risks, high costs, long-term hospitalization, and attendant morbidity are huge concerns for patients to undergo these procedures.[8]
To overcome those drawbacks, miniscrew-assisted rapid palatal expansion (MARPE) was developed.[9,10] MARPE has two variants, a tooth-bone borne or a solely bone-borne device with a rigid component linking to mini-screws implanted into the palate, enabling the direct expansion force to the basal bone of the maxilla. It was designed to maximize skeletal effects because the incomplete ossification of the mid-palatal suture in humans, even among older individuals, is demonstrated through recent histological research.[10] Therefore, MARPE is considered a non-surgical treatment for maxillary transverse deficiency.
Expression, symmetry, and appearance of the teeth and gingival display also have significant impacts on smile attractiveness. Many patients who require orthodontic treatment are motivated by dental esthetics.[11] The gummy smile is related to the visibility of an excessive amount of gingiva during smiling. The major etiological factors consist of a short upper lip, hyperactive upper lip, skeletal conditions, or altered passive eruption.[12] This study aimed to describe a successful case report regarding the treatment of buccal corridor and gummy smile by MARPE appliance, Niti wire bending, and gingivoplasty.
CASE REPORT
The 20-year-old female patient presented with a chief complaint of protruding lips, maxillary and mandibular incisors that were proclined, a gummy smile, and an excessive buccal corridor [Figure 1].
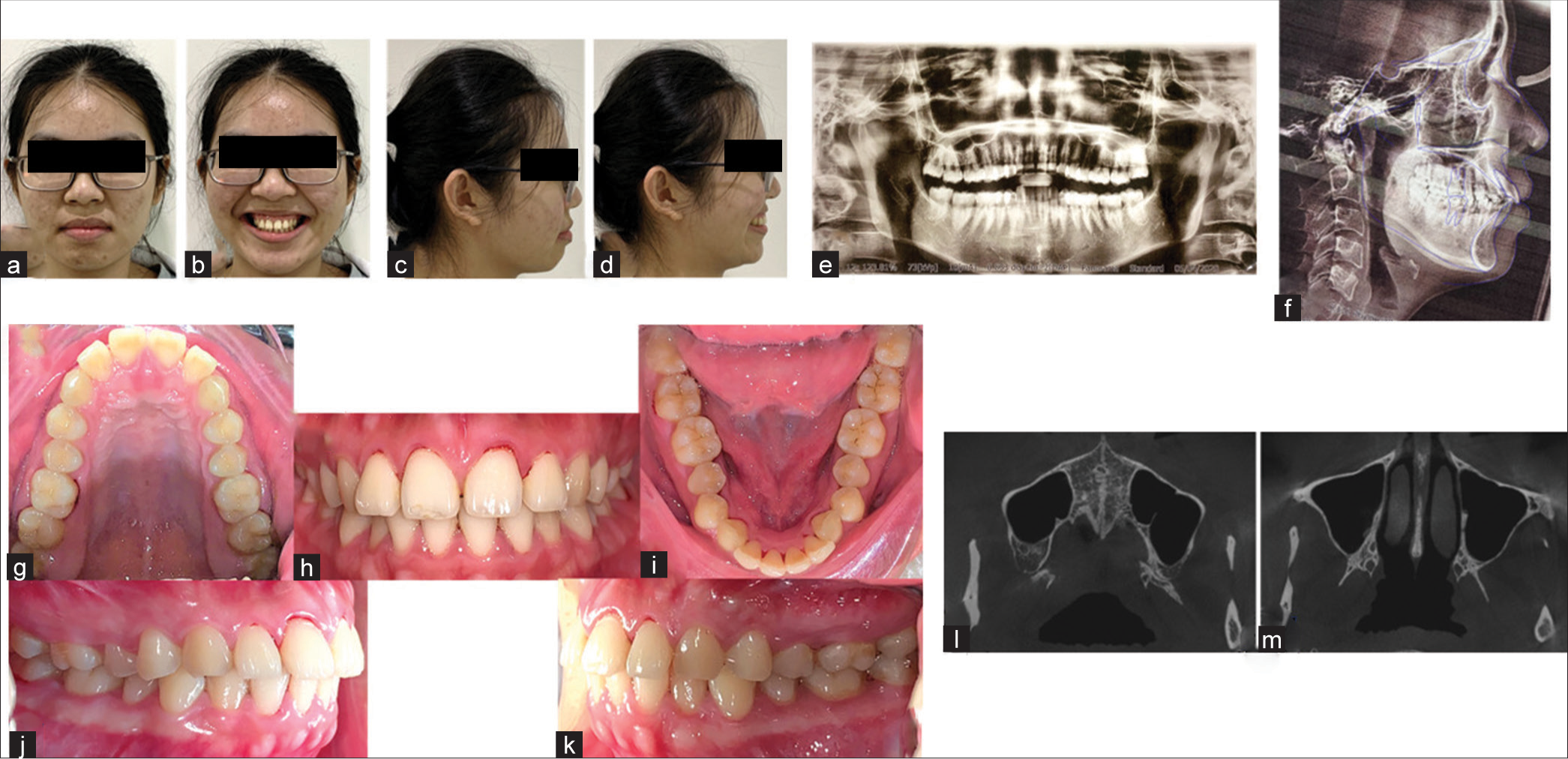
- (a-d) initial extraoral, (g-k) intraoral photographs, (e and f) panoramic and lateral cephalometric X-rays, (l and m) cone beam computed tomography (CBCT) scans.
Clinical findings
Soft tissue
Convex profile
Acute nasolabial angle
Strain on circumoral muscle when closing the mouth (no temporomandibular joint symptoms).
Dental
Molar relationship: Class I
Canine relationship: Class II (both sides)
-
Archform:
Upper: Severely narrow
Lower: Severely narrow, especially due to lingually inclined molars
-
Lower arch:
6 mm crowding
Flat curve of Spee
-
Bolton discrepancy:
Anterior: 3-3:82.7% (reduced)
Posterior: 91.8% (normal)
Midline: Upper and lower coincident with facial midline.
Skeletal
Skeletal jaw relationship: Class I
Maxilla and mandible: Relatively normal position (SNA 82.4°, SNB 79°, and ANB 3.4°)
Lower facial height: Reduced (FMA 21.4°).
-
Incisor angulation
Upper: Proclined (U1-SN 121.7°)
Lower: Proclined (L1-MP 100.8°).
Diagnostic assessment
Lip position assessment
Upper and lower lips protrusive
Both lips anterior to E-line
Smile: Gummy smile
Buccal corridors: Present.
Dental assessment
Molar relation: Class I
Canine relation: Class II (both sides)
-
Arch form:
Upper: Transverse deficiency with severe narrowing
Lower: Severe narrowing with mild crowding
Dental discrepancy: Bolton tooth size discrepancies
-
Incisor angulation:
Upper and mandibular incisors proclined.
Skeletal
Class I jaw relationship
Reduced lower facial height.
Treatment objectives
The objectives were to fix skeletal Class I malocclusion, with buccal corridors exceeding 4 mm, a gummy smile, and lingual tipping of the lower posterior segments.
Potential alternative treatments
In discussions with the patient regarding this case, we presented several treatment options, including the choice between the current treatment plan and extraction/distalization combined with the intrusion of the entire upper arch. However, the patient expressed concerns about the buccal corridor and preferred not to pursue the option involving the intrusion of the whole upper arch. Consequently, she opted for the treatment involving MARPE and gingivoplasty following the treatment process.
In the case of vertical maxillary excess, intrusion using temporary anchorage devices can be employed. Severe instances may require orthognathic surgery as part of the treatment.
Treatment timeline
First stage: MARPE appliance (three weeks)
Second stage: Fixed appliance with metal brackets (18 months)
Third stage: Gingivoplasty after one month of debonding
Treatment progress
The initial step involved the installation of the MARPE appliance, using a tooth-bone-born design. Teeth separators were placed mesiodistally of the U6s. One week later, the bands were fitted, and an impression was made to create the MARPE with an 8 mm body. The appliance was cemented in place a week later, and 4 mini-screws (1.8 × 12 mm) were inserted through the body of the MARPE. These screws were guided by four holes in the MARPE body, positioned between the second premolar and first molar, with two mini-screws installed at the back with bicortical support.
The braces were bonded on the same day, and a 0.014 Nitinol wire was inserted in both the upper and lower arches. During treatment, upper archwires were utilized for both upper and lower arches. The lower archwire was expanded in the posterior sector to aid the uprighting process, along with lingual buttons and a ¼ 3.5 oz cross elastic for facilitation.
The MARPE was expanded at a rate of 0.25 mm/turn, with an activation pattern of six turns on the first day, followed by two turns in the morning and evening until spacing occurred between 11 and 21 (on the fifth day). Subsequently, one turn was applied in the morning and evening until 4 mm of palatal expansion was achieved. Post-expansion, the MARPE was retained in place for eight months to allow for retention and palatal suture bone remodeling. Moreover, on the first day of bracket bonding, the upper wire was cut between 11 and 21.
In the second stage, after three weeks of MARPE, a continuous archwire and thread elastic were introduced to initiate the closure of the space. The upper cutting remained separated into two segments during the entire MARPE phase, and continuous wires were employed thereafter. When reaching the Nitinol 0.016 × 0.022 stage, a V bend was added between 11 and 21 to facilitate a translation movement while closing the space. For the finishing stage and addressing Bolton discrepancies, interproximal reduction (IPR) was performed on the lower anterior from distal 33 to distal 43 using IPR blades of 0.1 mm, 0.2 mm, and 0.3 mm, followed by fluor polishing. Post this, a 0.017 × 0.025 SS wire on the upper and 0.020 SS wire on the lower, along with Class II elastics (1/8 3.5), were utilized from L6s to U3s to correct the dental Class II relationship [Figures 2 and 3].
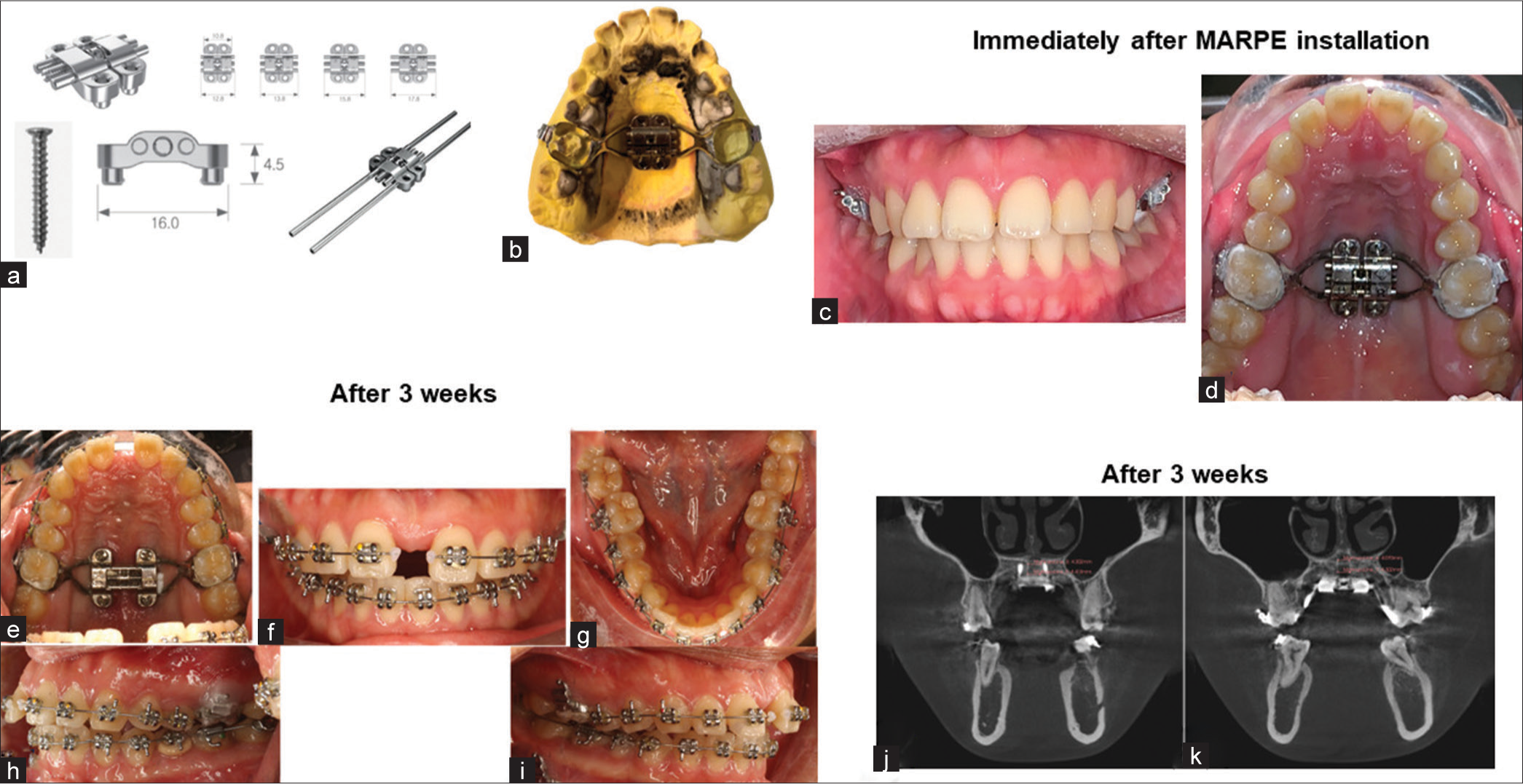
- (a) MARPE appliance, and (b) MARPE design, (c and d) immediately after MARPE installation, (e-i) three weeks after MARPE installation, and (j and k) cone beam computed tomography (CBCT) scans three weeks after MARPE installation; MARPE: miniscrew-assisted rapid palatal expansion.
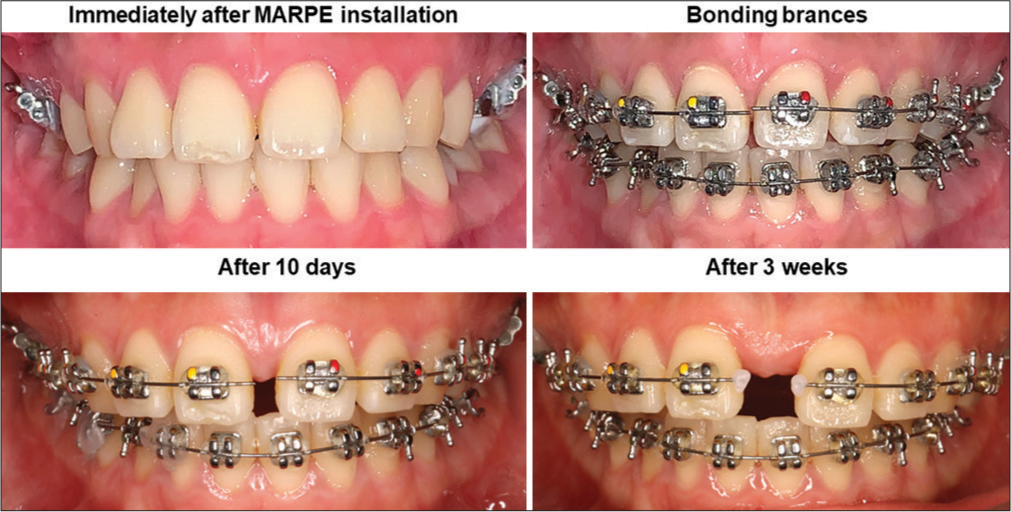
- MARPE: miniscrew-assisted rapid palatal expansion.
In the last stage, gingivoplasty was conducted, involving smile design before treatment presentation to the patient and guidelines for the gingivoplasty procedure. The process involved 2 mm gum cutting, flap opening for gum recontouring, alveolar bone trimming, and closure using medical sutures [Figure 4]. Finally, the Essix appliance was used for the retention protocol, with full-time wear in the first year and in the evenings from the second year onward.
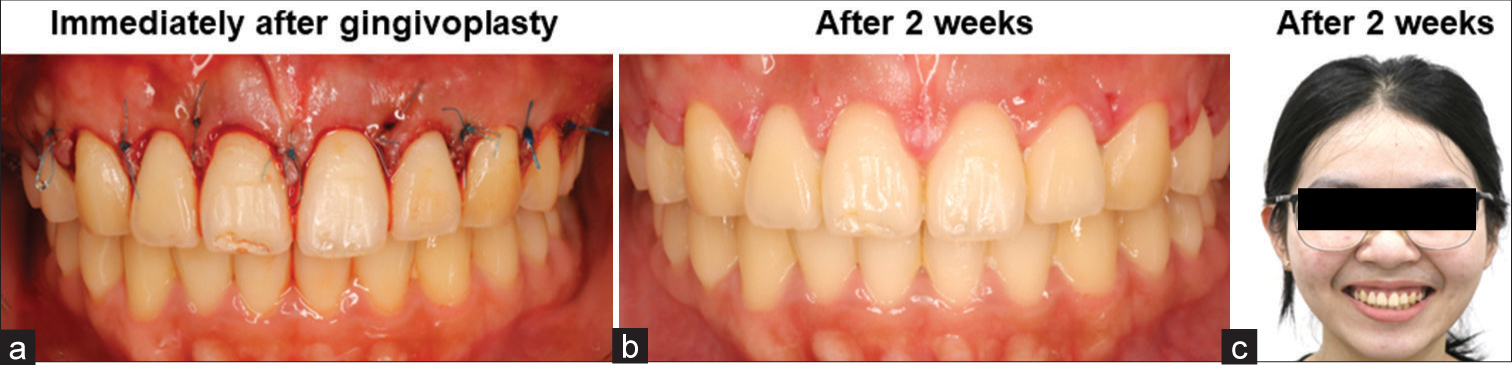
- (a) Immediately after gingivoplasty, and (b,c) two weeks after gingivoplasty.
Treatment results
All treatment objectives were successfully met, resulting in a well-aligned dentition and improved facial esthetics. The expansion of the mid-palatal suture reached 4 mm with minimal buccal crown tipping of the upper posterior teeth. Retraction of both upper and lower incisors effectively corrected severe overjet, utilizing the space created from the MARPE expansion.
The achieved outcomes include the maintenance of a Class I molar relationship and a slight Class II relationship on the canines, attributed to tooth size discrepancies; however, the occlusion is considered acceptable. The maxilla was expanded through MARPE, whereas the mandibular intra-arch width experienced slight expansion due to molar uprighting, as evidenced in cone-beam computed tomography (CBCT) scans [Figure 2].
Throughout the treatment, the retraction of both upper and lower lips facilitated a passive lip seal, contributing to a notably straight profile post-treatment. Minimal root resorption was observed, with good root parallelism achieved across most teeth, aside from tooth 44. There was a notable improvement in incisor inclination and soft-tissue profile, particularly evident in the E-line and nasolabial angle. Cephalometric analysis confirmed these changes, showing a decrease of 5.9° in the inclination of the maxillary incisors [Figures 4-7 and Table 1].

- Niti bending (V bend on 16 22 Niti between 11 21 and elastic thread for closing diastema), Niti: Nickel-titanium.
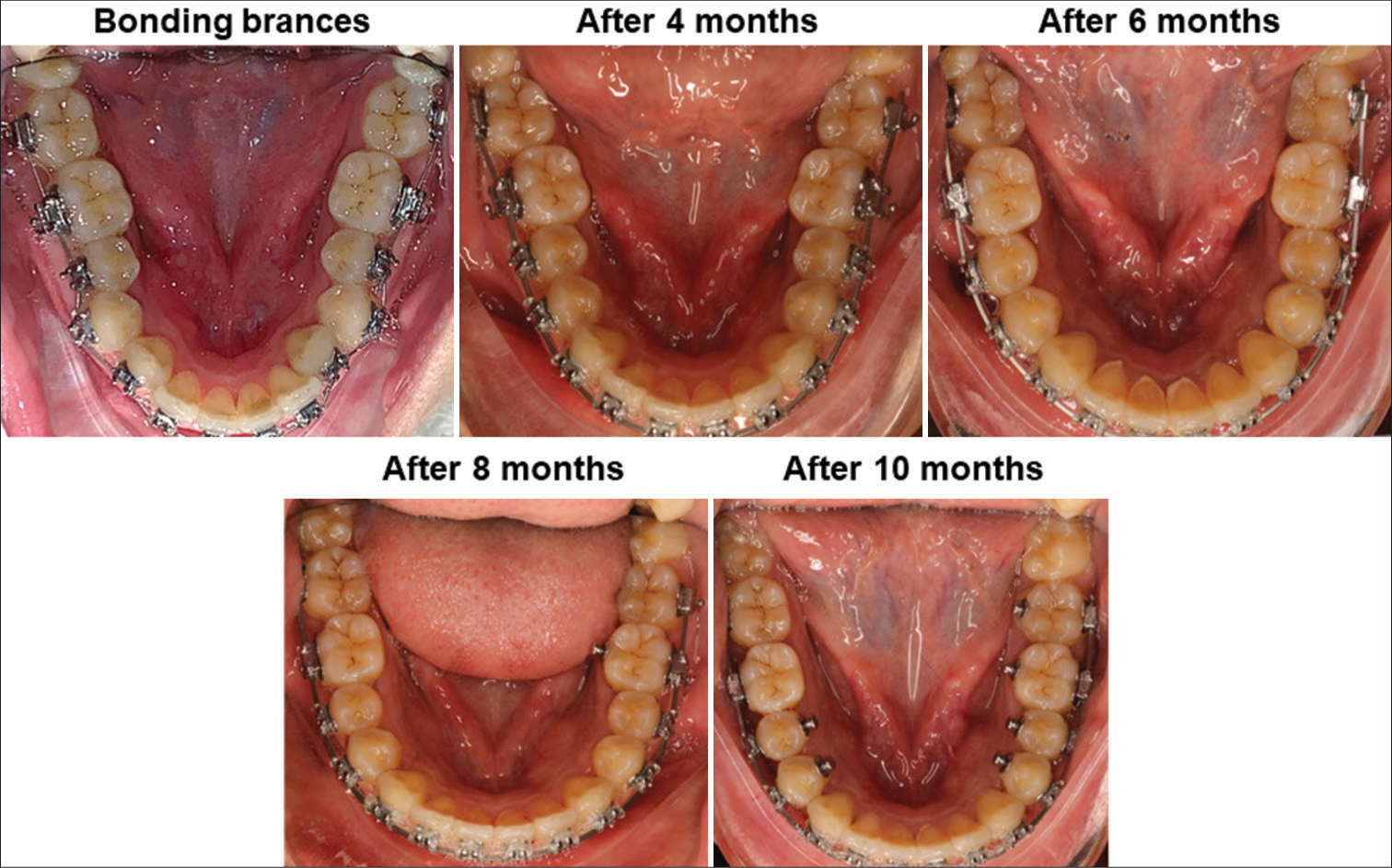
- Nickel-titanium (Niti) bending for buccal tipping posterior lower teeth.
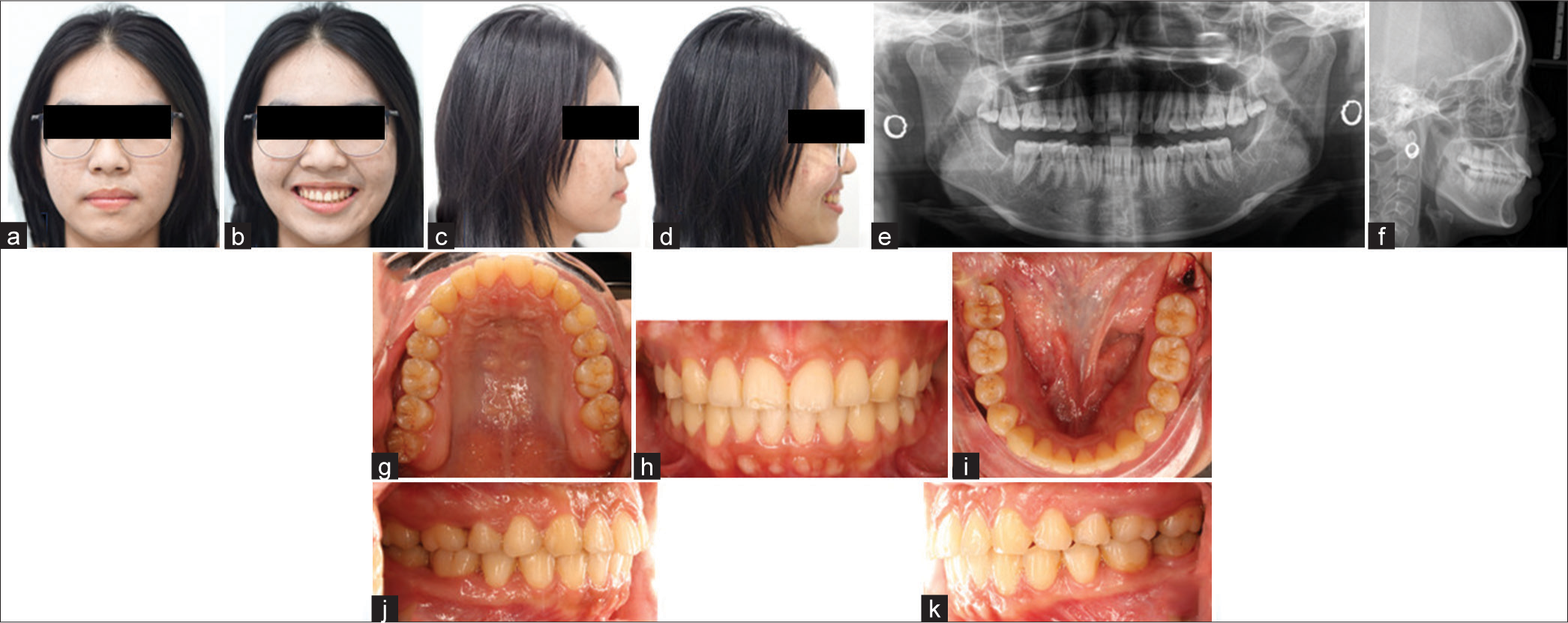
- (a-d) post-treatment extraoral, (e, f) panoramic and lateral cephalometric X-rays, (g-k) intraoral photographs.
| Measurement | Normal | Pre-treatment | Post-treatment | |
|---|---|---|---|---|
| SNA (°) | 78–82 | 82.4 | 82.4 | Skeletal |
| SNB (°) | 76–82 | 79 | 78.2 | |
| ANB (°) | 0–4 | 3.4 | 4.1 | |
| A-N Perp FH (mm) | −1.9–2.7 | 2.8 | 3.1 | |
| B-N Perp FH (mm) | −5.5–−1.5 | −0.6 | −1.7 | |
| FMA (°) | 25 | 24.4 | 23.7 | |
| Y-Axis (°) | 59 (53–63) | 60.4 | 60.2 | |
| U1-SN (°) | 104 | 121.7 | 114.8 | Dental |
| U1-NA (mm/°) | 4/22 | 8/39 | 4.5/32.4 | |
| U1-MaxP (°) | 110–116 | 127.9 | 122 | |
| U1-L1 (°) | 131 | 102.6 | 112.5 | |
| L1-NB (mm/°) | 4/25 | 8.7/34.8 | 6.4/31 | |
| L1-MP: IMPA (°) | 90 | 100.8 | 98.2 | |
| UL-E line (mm) | −4–−1 | −1.3 | −2 | Soft tissue |
| LL-E line (mm) | −2–0 | 0.7 | 0.4 |
ANB: A point, nasion, B point, FMA: Frankfort mandibular plane angle, IMPA: Incisor mandibular plane angle, L1: Lower central incisor, LL: Lower lip, MP: Mandibular plane, MaxP: Maxillary plane, NA: Nasion point A, NB: Nasion point B, SN: Sella nasion, SNA: Sella nasion point A, SNB: Sella nasion point B, U1: Upper central incisor, UL: Upper lip, E-line: A line connects the nose tip to the chin, A to N Perp FH: Distance between point A to Nasion perpendicular Frankfort plane (FH), B to N Perp FH: Distance between point B to Nasion perpendicular Frankfort plane.
After a 2-year follow-up, the results remain stable, and the patient expresses satisfaction with the outcome [Figure 8].
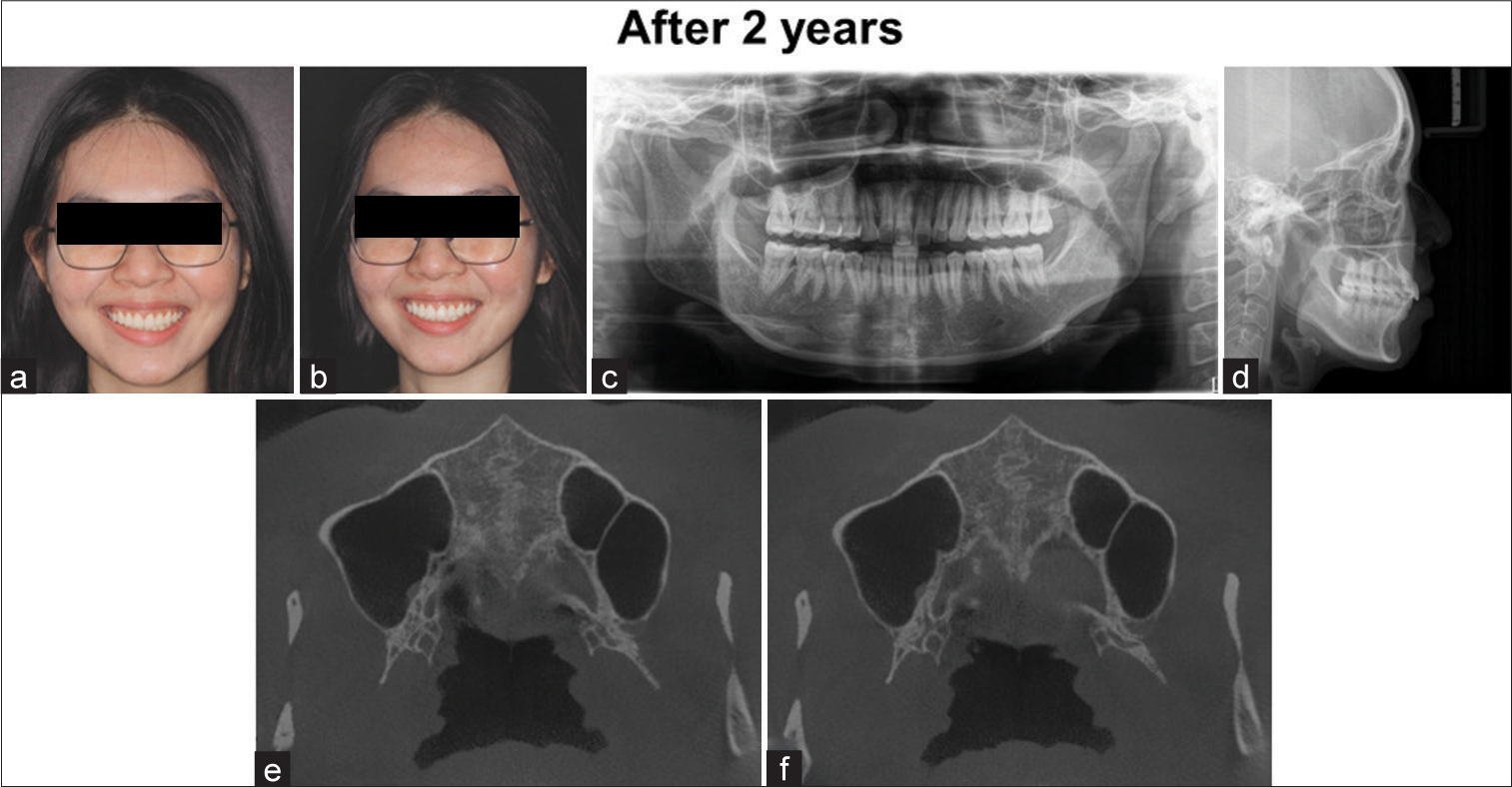
- (a-b) two years after treatment: extraoral, (c-d) panoramic and lateral cephalometric X-rays, and (e-f) cone-beam computed tomography (CBCT) scans.
DISCUSSION
This case report demonstrates a successful compensatory treatment of the buccal corridor and gummy smile with MARPE, Nickel-titanium (Niti) wire bending, and gingivoplasty.
The purpose was to expand the mid-palatal suture and address the buccal crown tipping of the lower posterior, aiming to reduce the issue of excessive buccal corridor and enhance the esthetic appearance of the smile. MARPE was considered a suitable choice for this case due to the normal crown torque of the upper posterior teeth, the need for an interproximal reduction on the lower anterior teeth, and the implementation of Class II elastics to reduce the proclination of the upper incisors, ultimately aiming to achieve a favorable occlusion. As the gummy smile originated from a gingival-based cause, surgery was selected as the treatment method. The CBCT revealed that the intermaxillary suture was at a stage B maturation level (the scalloped appearance of the high-density sutural line),[13] which has been linked to a high success rate with MARPE. However, some molar tipping occurred due to the appliance being tooth-bone-borne rather than bone-borne. Utilizing a MARPE appliance, a degree of buccal tipping is anticipated, despite significantly less compared to rapid palatal expansion (RPE), as teeth continue to serve as anchor units alongside mini-screws. The tendency for buccal tipping is directly linked to the resistance exerted by the mid-palatal suture.
Finally, to optimize the cosmetic outcome, an adjunctive procedure involving gingivoplasty was recommended post-treatment. Gingivoplasty was selected as the treatment choice due to the presence of altered passive eruption as the etiology, coupled with a favorable positioning of the incisal edge concerning the lower lip.
Research conducted by Gurgel et al.[14] and Christie et al.[15] has similarly highlighted a certain level of buccal tipping. Previous studies have suggested more pronounced alterations in molar inclination compared to premolars.[16] This greater buccal inclination observed in the first molar, as opposed to the first premolar, could potentially be attributed to the increased density of the buccal cortical bone in the maxillary canine and premolar areas.[17-19]
CONCLUSION
Utilizing bicortical mini-screws in MARPE has been shown to be an effective method in addressing buccal corridors. In addition, combining fixed orthodontic treatment with labial appliances and gingivoplasty has proven to be successful in correcting malocclusion and improving smile esthetics, demonstrating lasting and stable outcomes.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Therapeutic effects of botulinum toxin type A in subjects with gummy smile: A longitudinal sEMG approach. Int Orthod. 2021;19:652-8.
- [CrossRef] [PubMed] [Google Scholar]
- Influence on smile attractiveness of the smile arc in conjunction with gingival display. Am J Orthod Dentofacial Orthop. 2013;144:541-7.
- [CrossRef] [PubMed] [Google Scholar]
- Buccal corridors and smile esthetics. Am J Orthod Dentofacial Orthop. 2005;127:208-13.
- [CrossRef] [PubMed] [Google Scholar]
- The smile buccal corridors: Aesthetic value for dentists and laypersons. Prog Orthod. 2006;7:56-65.
- [Google Scholar]
- Surgically assisted rapid palatal expansion (SARPE): A literature review. Sch J Dent Sci. 2021;8:25-40.
- [CrossRef] [Google Scholar]
- Periodontal effects of surgically assisted rapid palatal expansion evaluated clinically and with cone-beam computerized tomography: 6-month preliminary results. Am J Orthod Dentofacial Orthop. 2011;139:S117-28.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically assisted rapid palatal expansion: A literature review. Am J Orthod Dentofacial Orthop. 2008;133:290-302.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically assisted rapid maxillary expansion: A systematic review of complications. Int J Oral Maxillofac Surg. 2020;49:325-32.
- [CrossRef] [PubMed] [Google Scholar]
- An interview with Won Moon. Dental Press J Orthod. 2013;18:12-28.
- [CrossRef] [PubMed] [Google Scholar]
- Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137:830-9.
- [CrossRef] [PubMed] [Google Scholar]
- Do dental esthetics have any influence on finding a job? Am J Orthod Dentofacial Orthop. 2014;146:423-9.
- [CrossRef] [PubMed] [Google Scholar]
- Esthetic lip repositioning: A cosmetic approach for correction of gummy smile-a case series. J Indian Soc Periodontol. 2019;23:290-4.
- [CrossRef] [PubMed] [Google Scholar]
- Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013;144:759-69.
- [CrossRef] [PubMed] [Google Scholar]
- Transverse changes after surgically assisted rapid palatal expansion. Int J Oral Maxillofac Surg. 2014;43:316-22.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: A cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2010;137:S79-85.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal bone density in adult subjects: Implications for mini-implant placement. Angle Orthod. 2010;80:137-44.
- [CrossRef] [PubMed] [Google Scholar]
- Transverse dentoalveolar changes after slow maxillary expansion. Am J Orthod Dentofacial Orthop. 2011;140:317-25.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749-58.
- [CrossRef] [PubMed] [Google Scholar]







