Translate this page into:
Three-dimensional evaluation of dentoalveolar and skeletal transverse changes between rapid maxillary expansion and slow maxillary expansion in growing subjects – A systematic review and meta-analysis

*Corresponding author: Abirami Selvaraj, Department of Orthodontics, Chettinad Dental College and Research Institute, Kelambakkam, Tamil Nadu, India. varshaabi77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Selvaraj A, George AM, Arvind P. Three-dimensional evaluation of dentoalveolar and skeletal transverse changes between rapid maxillary expansion and slow maxillary expansion in growing subjects – A systematic review and meta-analysis. APOS Trends Orthod. 2024;14:203-13. doi: 10.25259/APOS_180_2022
Abstract
To systematically compare dentoalveolar and skeletal changes of RME and SME using same expanders with different activation protocols via 3D radiographs. Pubmed, Scopus, LILACS, Cochrane Library and Google Scholar were searched till April 2022. Randomized control trials (RCTs) were included. Statistical analysis performed with Tau2 test to evaluate heterogeneity in the included studies. Risk of bias (RoB) was evaluated using Cochrane RoB 2.0 tool. 5 RCTs were included. RoB revealed one study have low risk of bias and others have some concerns. Meta-analysis showed that both RME and SME displayed significant intermolar expansion (p>0.05) with RME showing significantly greater molar tipping. Random effects meta-analysis performed for maxillary intermolar distance at cuspal [SMD=0.23(95% CI=-0.50 to 0.95)] and alveolar level [SMD=0.76(95% CI=-0.57 to 2.09)] revealed no significant difference between groups with low reliability. RME showed significantly increased posterior skeletal nasal width [P value=0.007, SMD= 0.95(95% CI= 0.25 to 1.64)] with low heterogeneity (I2=24%) and good reliability. Greater molar tipping, determined using buccolingual inclination can be noted in RME. Increase in effective arch width and greater bodily translation was observed in SME. Utilizing the correct expansion protocol in the relevant clinical scenarios can prevent adverse periodontal complications during expansion and provide greater post-expansion stability.
Keywords
Slow maxillary expansion
Rapid maxillary expansion
Cone-beam computed tomography
Expander
INTRODUCTION
Transverse dimension discrepancies are clinically distinguished as cross-bites when the lower posteriors are positioned either buccally or lingually to the upper posteriors.[1,2] Unilateral or bilateral posterior cross-bites typically associated with transverse maxillary deficiencies are observed in 8–22% of growing patients.[3-5]
Maxillary expansion in the form of slow maxillary expansion (SME) or rapid maxillary expansion (RME) is recommended to improve occlusal relationships[6] and prevent the development of anatomical alterations that may cause functional disturbances.[7] It increases the transverse width with a combination of orthodontic and orthopedic effects through the opening of the midpalatal suture.[8,9] Interceptive correction combined with adequate rehabilitation may restore normal growth and jaw function.[10,11] In general, greater the age of the patient, higher the dental effects and smaller the skeletal changes.[12] It has been reported that RME, associated with tooth/tissue-borne appliances (Hyrax/Haas), has immediate effects and acts by applying heavy forces over a short period of time.[6] A coil spring or quad helix appliance is more commonly associated with SME because it uses continuous low-force systems over a longer period of time, which has been claimed to be a more physiological approach with greater sutural stability.[13,14] Previous studies have claimed that RME minimizes lateral tooth movements and maximizes skeletal displacements while SME promotes bone growth in intermaxillary sutures, leading to greater treatment stability.[15,16] The advantages and disadvantages of each protocol have been assessed with multiple study designs, and yet, the issue remains unclear and controversial because the different devices and methodologies may interfere with comparisons between the two expansion procedures.
Several studies have assessed skeletal, dentoalveolar, and periodontal changes from both expansion modalities through two-dimensional (2D) imaging (lateral/frontal cephalometry, panoramic radiographs, photographs, and plaster models).[17] However, limitations of 2D imaging such as projection errors, distortions, and difficulty in landmark identification due to structure superimposition can influence the generated findings.[18,19] To overcome these limitations, 3D imaging in the form of computed tomography (CT) was first utilized by Timms et al. in 1982 for assessing transverse maxillary dimensions.[20] This was followed by the advent of cone-beam CT (CBCT) which has ushered in a new age of dental diagnostics.[21] CBCT can be used to measure linear dimensions between skeletal and dental landmarks in a real-world setting with the availability of reconstruction software accounting for high precision and accuracy.[22,23] Despite the extensive research and literature available, practitioners’ clinical experience and attitude still have a major role in their choice of RME or SME expansion techniques. As a result, strong evidence is necessitated to defend this preference. Randomized control trials (RCTs) that have evaluated data using 3D techniques were included in the review to increase the reliability of evidence and eliminate bias in the comparison of methods between these two expansion procedures.
This review aimed to evaluate the skeletal and dentoalveolar effects produced by two different maxillary expansion protocols using similar jackscrew expanders through 3D radiographs.
MATERIAL AND METHODS
Protocol registration
The present review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The review protocol was submitted under the PROSPERO database (CRD42020219075).
Search strategy
Electronic databases including PUBMED, Cochrane Library, Google Scholar, Scopus, and LILACS along with a complimentary manual search of key orthodontic journals till April 2022 were performed. Keywords were customized for each database and are mentioned in [Table 1].
| S. No | Database | Search terms | No. of hits |
|---|---|---|---|
| 1 | PUBMED | (orthodontics) OR (orthodontic patients) OR (fixed orthodontic appliances) AND (slow maxillary expansion) OR (SME) OR (slow mechanical expansion) OR (slow palatal expansion) AND (rapid maxillary expansion) OR (RME) OR (rapid palatal expansion) OR (rapid mechanical expansion) AND (three dimensional evaluation) AND (3 D evaluation) AND (skeletal transverse width) OR (skeletal transverse changes) AND (dental transverse changes) OR (dentoalveolar changes) OR (dental transverse width) | 19 |
| 2 | Google Scholar | Three Dimensional AND Rapid AND Slow “Maxillary expansion” AND skeletal and dental changes | 77 |
| 3 | Cochrane | Slow maxillary expansion OR SME AND rapid maxillary expansion OR SME AND orthodontic patients and transverse dental and skeletal width AND three dimensional |
7 |
| 4 | Lilacs | Rapid palatal expansion or rapid maxillary expansion (title words) and slow palatal expansion or slow maxillary expansion (title words) and three-dimensional evaluation or 3 d evaluation (title words) |
1 |
| 5 | Scopus | Orthodontic patients OR orthodontic appliances AND slow maxillary or palatal expansion AND Rapid palatal or maxillary expansion AND three-dimensional evaluation AND skeletal and dental transverse changes. | 45 |
Bibliographies of the included full-text articles were scanned for relevant studies. No restrictions were done on the language or date of publication. Duplicate studies from different databases were eliminated manually. Initially, the titles of all studies identified through search strategies were screened by two independent authors, and irrelevant studies were excluded. The screened studies were then subjected to the eligibility criteria. Full texts were then procured for the articles which fulfilled the inclusion criteria. Additional studies were hand-searched from reference lists of all eligible studies to detect any missed publications from databases.
Population, Intervention, Comparison, Outcome (PICO) analysis
Population: Growing patients in either mixed or permanent dentition, maxillary transverse discrepancy, unilateral or bilateral cross-bite.
Intervention: Treatment with a fixed expansion device such as a jack screw expander (e.g., Hyrax and Haas) used to achieve RME. Typically activated once a day.
Comparison: Treatment with similar fixed jack screw expander as the intervention group (e.g., Hyrax and Haas) used to achieve SME. Typically activated once/twice a week.
Outcome
Primary outcomes
3D radiographic assessment of transverse dentoalveolar (intermolar width [IMW], molar inclination) changes.
Secondary outcomes
3D radiographic assessment of transverse skeletal changes. Adverse effects such as root resorption, periodontal problems, and patient-reported outcomes such as pain/discomfort.
Eligibility criteria
Inclusion criteria
RCT, growing subjects, subjects treated with fixed jack screw expander (e.g., Hyrax and Haas) were included in the study.
Exclusion criteria
Controlled clinical trials, retrospective studies, case reports, abstracts, adolescents >13 years, patients undergoing pre-surgical orthodontics, expansion with facemask therapy, cleft lip and palate, and craniofacial syndromes were excluded from the study.
Data collection process
Study selection was done according to the guidelines mentioned in the PRISMA flow chart [Figure 1]. Data required for analysis were extracted by both reviewers (AS and AMG) independently. Disagreements with respect to the data collected were resolved by a third author (PA). Baseline study characteristics of included articles were tabulated and are presented in [Table 2].
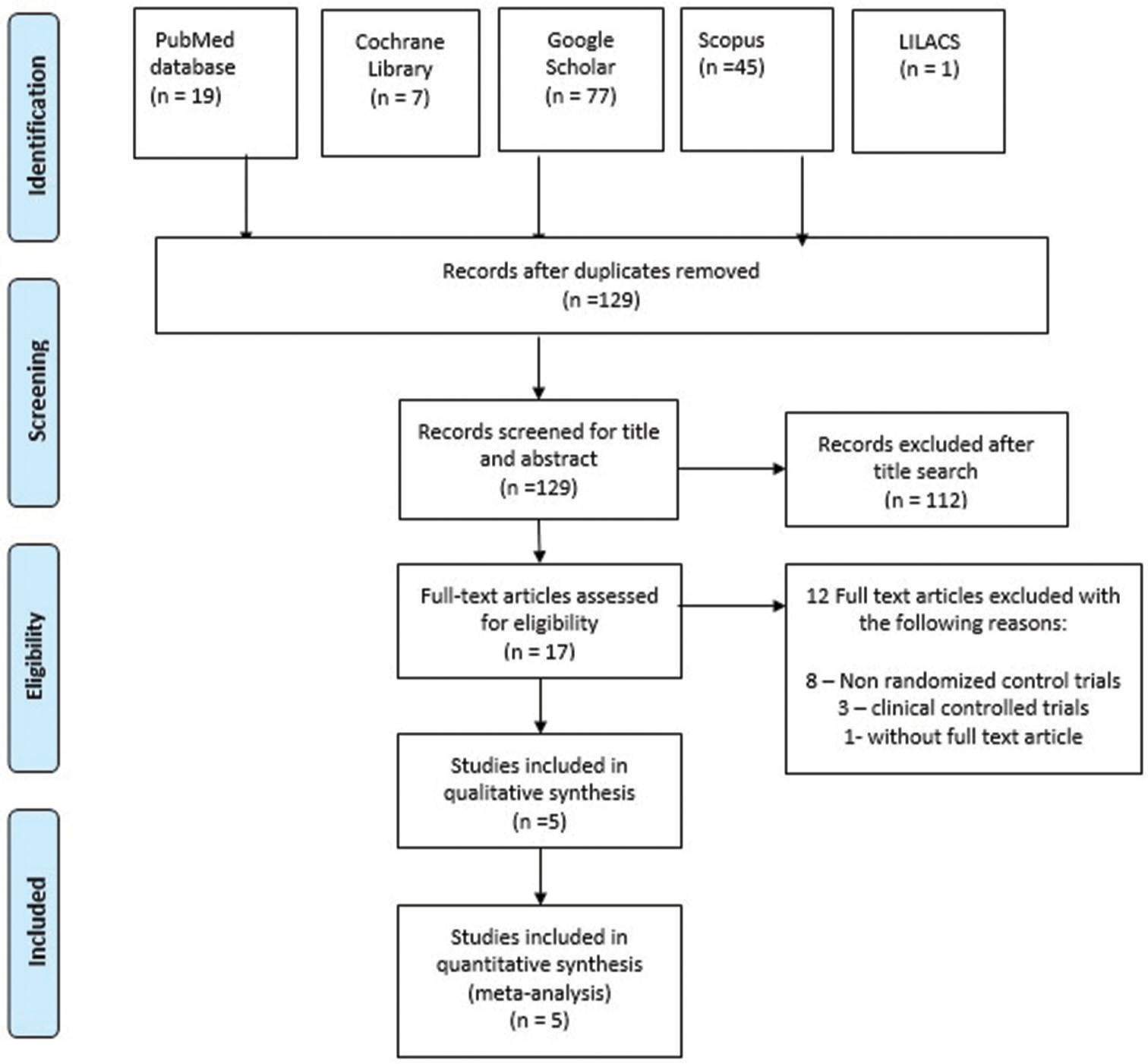
- Preferred reporting items for systematic reviews and meta-analyses flow chart.
| S. No |
Author and year of study | Design | Study groups, appliance, and mean age | Sample size | Activation frequency and activation period | Anchorage teeth, monitoring period, and retention period | Evaluation intervals and follow-up | Parameters assessed |
|---|---|---|---|---|---|---|---|---|
| 1 | Martina et al. (2012)[9] | RCT | Group 1: RME Group 2: SME Two band palatal expander RME: 9.7 ± 1.5 years SME: 10.3 ± 2.5 years. |
Total: 26 RME: 14 SME: 12 |
RME: 3 times (0.75 mm)/day. Initial activation: 2 mm/8 times SME: Twice/week (0.50 mm). Until 2 mm molar transverse overcorrection was achieved |
Maxillary first permanent molars RME: Once a week SME: Every 2 weeks Appliance as retainer |
MSCT T1-pre treatment T2-After 7 months of the appliance removed. RME: 7 months SME: 7 months |
Skeletal measurements: • AME • PME • PE Dentoalveolar measurements: IMW IMA |
| 2 | Brunetto et al. (2013) [27] | RCT | Group 1: RME Group 2: SME Haas-type palatal expander RME: 8.9 years SME: 9 years |
Total: 59 RME: 28, SME: 31 Final: 33 RME: 17 SME: 16 |
RME: 1/2 turn (0.4 mm)/day, 21–28 days. 1st day activation: full turn. SME: 1/2 turn (0.4mm)/week, 141–148 days. 1st day activation: half turn. Until the screw has opened 8 mm in both groups achieved with 40 activations |
Maxillary first deciduous molars and first permanent molars Every 15 days Appliance as retainer RME: 5 months SME: 1 month |
CBCT T1-pre treatment T2-between 1 and 7 days after stabilization of the screw. RME: 3 weeks SME: 20 weeks |
Skeletal measurements: Alveolar bone height and Alveolar bone thickness Dentoalveolar measurements: IMA IMW |
| 3 | Pereira et al. (2017)[25] | RCT | Group 1: RME Group 2: SME Haas-type palatal expander For initial sample size: RME: 8.18 years SME: 8.43 years. Final sample size:RME: 8.43 years, SME: 8.70 years |
Total: 57 RME: 28, SME: 29 Final: 37 RME: 21 SME: 16 |
RME: 1/2 turn (0.4 mm)/day, 3 weeks 1st day activation: full turn. SME: 1/2 turn (0.4mm)/week, 20 weeks. 1st day activation: half turn. Until screw has opened 8mm in both groups achieved with 40 activations |
Maxillary first deciduous molars and first permanent molars Every week Appliance as retainer RME: 5 months SME: 1 month |
CBCT T1-pre- treatment T2-between 1 and 7 days after stabilization of the screw RME: 3 weeks SME: 20 weeks |
Skeletal measurements: Sagittal SNA, SNB, ANB, SN perp-A Vertical- SNperp.PP, SN-ENA, SN. GoGnTransverse– PABW PAP Dentoalveolar measurements: IMA. |
| 4 | Lo Giudice et al. (2017)[28] | RCT | Group 1: RME Group 2: SME Hyrax expander RME: 10.4 years SME: 10.5 years |
Total: 20 RME: 10 SME: 10 |
RME: 4 times (0.8 mm)/day, 8.5 days. SME: twice (0.4 mm)/week, 126.2 days. Until 2 mm of overexpansion was achieved |
Maxillary first permanent molars Appliance as retainer | CBCT T1-pre- treatment T2-After 7 months of appliance removed RME: 7 months SME: 7 months |
Skeletal measurements: PNW PW TNV. Dentoalveolar measurements: IMW |
| 5 | Luiz Ulema Ribeiro et al. (2020)[26] |
RCT | Group 1: RME Group 2: SME Haas-type palatal expander RME: 8.6 years SME: 9.3 years |
Total: 59 RME: 31 SME: 28 Final: 29 RME: 16 SME: 13 |
RME: 1/2 turn (0.4 mm)/day, (18 days). 1st day activation: full turn. SME: 1/2 turn (0.4mm)/week, 5 months 1st day activation: half turn Until screw has opened 8 mm in both groups achieved with 40 activations |
Maxillary first deciduous molars and first permanent molars Every 15 days Appliance as retainer RME: 5 months SME: 1 month |
CBCT T1-pre treatment T2-Between 1 and 7 days after stabilization of the screw. RME: 6 months SME: 6 months |
Dentoalveolar measurements: IMW ICW Skeletal measurements: PNW, PABW, PAPW ANW, APBSW, AABW, AABIW, AAPW, and IOW |
AME: Anterior maxillary expansion, PME: Posterior maxillary expansion, PE: Pterygoid expansion, IMW: Intermolar width, IMA: Intermolar angle, PW: Palate width, TNV: Total nasal volume, IOW: Interorbital width, PNW: Posterior nasal width, PABW: Posterior apical base width, PAPW: Posterior alveolar process width, ANW: Anterior nasal width, AABWS: Anterior apical base superior, AABW: Anterior apical base width, AABWI: Anterior apical base width inferior, AAPW: Anterior alveolar process width, MSCT: Multi-slice computed tomography, CBCT: Cone beam computed tomography, RCT: Randomized Control Trial, RME: Rapid Maxillary Expansion, SME: Slow Maxillary Expansion, SNA: Angle between S-N line and N-A line, SNB: Angle between S-N line and N-B line, ANB: Angle between SNA and SNB, SN-ENA: Orthogonal distance to S-N line from ANS
Study risk of bias (RoB) assessment
Cochrane RoB 2.0 tool utilizing five domains was used for assessing RoB [24] [Figure 2]. Each RCT was then assigned under high, unclear, or low risk. Out of the five domains, even if one domain was unclear or high, then overall RoB becomes unclear or high, respectively. Two authors (AS and AMG) performed the RoB independently and a consensus-based discussion involving a third author (PA) was done to resolve disparities. The Cohen κ test was used to assess agreement level between reviewers and a coefficient value of 0.923 suggested a high degree of agreement.
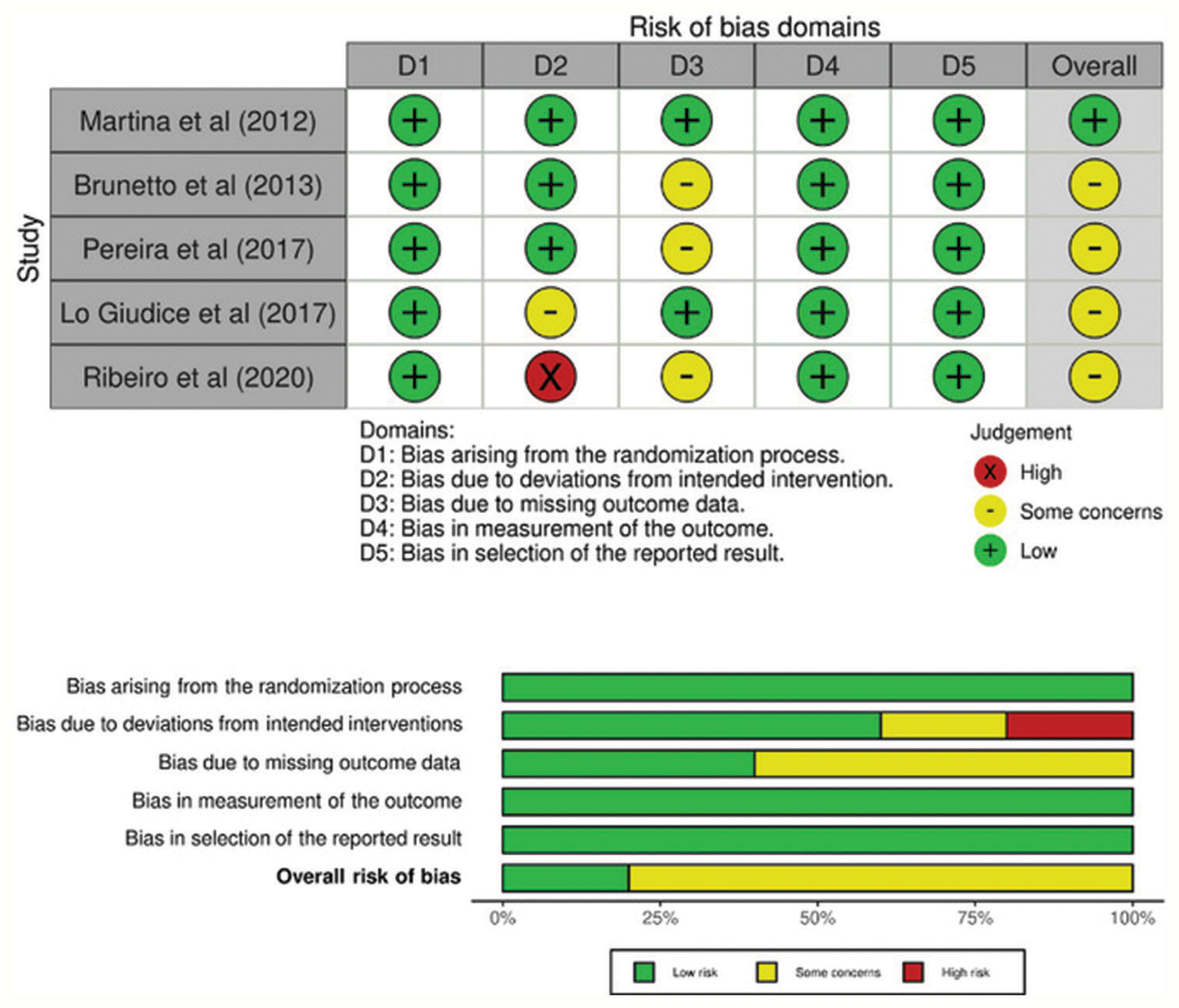
- Risk of bias summary.
Meta-analysis
Statistical heterogeneity was evaluated from obtained forest plots of IMW changes, intermolar angle (IMA), and posterior skeletal transverse width changes. A Chi-square test was used to determine heterogeneity where P < 0.1 meant significant heterogeneity. I2 tests were done to quantify the extent of heterogeneity with values of 25, 50, and 75%, corresponding to low, moderate, and high heterogeneity, respectively. A random effects model was chosen to determine the pooled estimates. The Tau2 test was used to assess heterogeneity in the random-effects model. Meta-analyses were undertaken using the Review Manager program (RevMan Version 5.3; Copenhagen: The Nordic Cochrane Centre, Cochrane Collaboration, 2014).
Evidence level of selected articles
All five[9,25-28] included studies had a Level 2 Evidence design.
RESULTS
An electronic search identified a total of 149 studies. After the removal of duplicates, there were a total of 129 articles, which were subjected to further screening of titles and abstracts. One hundred and twelve articles were excluded and a total of 17 articles were assessed for eligibility. After excluding 12 articles not meeting the eligibility criteria, five studies were identified and included for qualitative and quantitative analysis. The results of the search were illustrated in the PRISMA flow chart [Figure 1]. All the included studies were RCTs. A total of 145 participants were involved, all of whom were treated with either slow or rapid expansion protocols.
RoB of the included studies
Results of RoB for included RCTs are presented in [Figure 2]. Out of five RCTs, one[9] had low RoB whereas the other four[25-28] had some concerns.
3D analysis of transverse dentoalveolar changes between RME and SME
IMW at cuspal level
Four RCTs[9,26-28] have assessed IMW at cuspal level following expansion with two different protocols of which only Luiz Ulema Ribeiro et al.[26] reported a significantly greater change in RME when compared to SME (P < 0.001) [Table 3].
| S. No |
Authors | Dental parameters | Landmarks | RME (mean±SD) |
SME (mean±SD) |
RME-SME Difference and Statistically Significant Differences |
|---|---|---|---|---|---|---|
| 1 | Martina et al. (2012)[9] | IMW at cuspal level (mm) | Distance between mesiopalatal cusp tip of upper first permanent molars. | 5.7±1.6 *P<0.001 |
6.3±2.1 *P<0.001 |
−0.6 |
| IMW at apex level (mm) |
Distance between palatal root apices of upper first permanent molars |
4.7±1.2 *P<0.001 |
6.0±1.7 *P<0.001 |
−1.3 *P=0.02 |
||
| IMA (mm) | Measured as the difference between the apex of palatine roots and mesiopalatal cusp tip of upper first permanent molars. |
1.0±1.2 *P<0.05 |
0.3±0.9 P>0.05 NS |
0.7 | ||
| 2 | Brunetto et al. (2013)[27] |
IMW at cuspal level (mm) |
Distance between mesiobuccal cusps of upper first permanent molars. |
9.26±2.05 *P<0.001 |
9.02±1.7 *P<0.001 |
0.24 P=0.7194 NS |
| IMW at apex level (mm) | Distance between most buccal points of mesiobuccal roots of upper first permanent molars |
4.85±1.31 *P<0.001 |
6.39±1.12 *P<0.001 |
1.12 *P=0.0011 |
||
| IMA (degrees) | Angle formed by tangents to both mesial cusps of upper first permanent molars. |
−12.88±9.35 *P<0.001 |
−7.87±6.8 *P<0.001 |
−5.01 P=0.9050 NS |
||
| 3 | Pereira et al. (2017)[25] |
IMW at alveolar level(mm) | Linear distance of the lowest point of the alveolar process of the right side to the left side |
5.03±1.66 *P<0.001 |
4.86±1.44 *P<0.001 |
0.17 P=0.736 NS |
| IMA (degrees) | Angle formed by the apex of palatal root and the distobuccal cusp of upper first permanent molars. |
20.73±5.06 *P<0.001 |
9.22±6.18 *P<0.001 |
11.51 *P<0.001 |
||
| 4 | Lo Giudice et al. (2017)[28] |
IMW at cuspal level (mm) | Distance between the apex of mesiopalatal cusp of upper first permanent molars. |
6.11±1.89 | 6.67±2.36 | −0.56 |
| 5 | Luiz Ulema Ribeiro et al. (2020)[26] | IMW at cuspal level (mm) |
Distance between mesiopalatal cusp tips of upper first permanent molars. |
6.64±1.95 *P<0.05 |
4.10±1.66 *P<0.05 |
2.54 *P<0.001 |
| IMW at alveolar level (mm) | Measured as the distance between the right and left alveolar process at their most inferior limit | 5.97±1.19 *P<0.05 |
4.11±1.29 *P<0.05 |
1.86 *P=0.001 |
IMW at apical level
Brunetto et al. and Martina et al.[9,27] assessed IMW at apical level and reported significantly lesser expansion in RME compared to SME (P < 0.05) [Table 3].
IMW at alveolar level
Pereira et al. and Luiz Ulema Ribeiro et al.[25,26] have assessed IMW at alveolar levels of which Luiz Ulema Ribeiro et al.[26] reported IMW to be significantly greater in RME compared to SME (P < 0.05) [Table 3].
IMA
Three studies[9,25,27] have assessed IMA and reported molar inclination to be significantly greater in RME when compared to SME (P < 0.05) [Table 3].
3D analysis of transverse skeletal changes between RME and SME
Posterior maxillary expansion
Three RCTs[9,25,26] have assessed posterior maxillary expansion of which Pereira et al. and Luiz Ulema Ribeiro et al.[25,26] have assessed posterior apical base width (PABW) and reported a significantly greater increase in RME (P < 0.05). Martina et al.[9] assessed two posterior skeletal parameters (level of pterygoid process and level of greater palatine foramen) and reported expansion at pterygoid process to be significantly greater in RME (P < 0.05) [Table 4].
| S. No | Authors | Skeletal parameters | Landmarks | RME (mean±SD) | SME (mean±SD) | RME-SME Differences and statistically significant differences |
|---|---|---|---|---|---|---|
| 1 | Martina et al. (2012)[9] | Anterior maxillary expansion (mm) | Measured at piriform aperture level | 2.5±1.5 *P<0.001 |
1.9±1.3 *P<0.001 |
0.6 |
| Posterior maxillary expansion (mm) | Measured at greater palatine foramen level | 2.4±0.9 *P<0.001 |
1.9±1.0 *P<0.001 |
0.5 | ||
| Pterygoid expansion (mm) | Measured at apices of pterygoid process level | 1.2±0.9 *p<0.001 |
0.6±0.6 *p<0.05 |
0.6 *p=0.04 |
||
| 2 | Pereira et al. (2017)[27] | Posterior apical base width (mm). | Distance between right and left buccal contours of maxilla using tangent to lower border of the nasal cavity. | 1.76±2.08 *P=0.001 |
1.09±2.82 P=0.142 NS |
6.67 *P=0.412 |
| 3 | Lo Giudice et al. (2017) [28] | Posterior nasal width (mm) | Maximum distance between the right and left nasal wall | 3.13±0.82 | 2.67±0.74 | 0.46 |
| 4 | Luiz Ulema Ribeiro et al. (2020)[26] | Posterior nasal width (mm) | Maximum distance between the right and left nasal wall | 2.38±0.63 *P<0.05 |
1.45±0.80 *P<0.05 |
0.93 *P=0.02 |
| Posterior apical base width (mm). | Distance between right and left buccal contours of maxilla using tangent to lower border of the nasal cavity. | 2.72±0.90 *P<0.05 |
1.79±0.82 *P<0.05 |
0.93 *P=0.007 |
||
| Anterior nasal width (mm) | Maximum distance between right and left nasal wall at 10 mm anterior to crista galli | 2.65±0.90 *P<0.05 |
1.32±0.83 *P<0.05 |
1.34 *P<0.01 |
||
| Anterior apical base width (mm) | Distance between right and left buccal contours of maxilla using tangent to lower border of nasal cavity at 10 mm anterior to crista galli | 3.47±1.52 *P<0.05 |
1.38±1.22 *P<0.05 |
2.08 *P=0.001 |
||
| Anterior alveolar process width (mm) | Measured as distance between right and left alveolar process at their most inferior limit at 10 mm anterior to crista galli | 5.57±2.22 *P<0.05 |
4.36±1.89 *P<0.05 |
1.21 P=0.130 NS |
Anterior maxillary expansion
Martina et al. and Brunetto et al.[9,27] have assessed anterior maxillary expansion with varying reference landmarks. Martina et al.[9] assessed at the piriform aperture level with no significant differences between groups. Luiz Ulema Ribeiro et al.[26] assessed anterior apical base width and reported significantly greater changes in RME (P < 0.05) [Table 4].
Skeletal nasal width
Luiz Ulema Ribeiro et al. and Lo Giudice et al.[26,28] assessed skeletal nasal width. Luiz Ulema Ribeiro et al.[26] analyzed anterior and posterior nasal width (PNW) and reported a significant increase in RME (P < 0.05). Contrastingly, Lo Giudice et al.[28] reported PNW to be increased in RME, though not statistically significant (P > 0.05) [Table 4].
Meta-analysis
[Figure 3] is a graphical representation of random-effects meta-analyses done to compare IMW at cuspal level for four studies[9,26-28] and alveolar level for two studies.[25,26] With respect to the cuspal level, overall effect P = 0.54 (SMD = 0.23 [95% Confidence Intervals [CI] = −0.50– 0.95]) indicates no statistically significant changes between groups. Heterogeneity (I2 = 71%) is high and indicates low reliability. With respect to the alveolar level, overall effect P = 0.26 (SMD = 0.76 [95% CI = −0.57–2.09]) indicates no statistically significant changes between groups. Heterogeneity (I2 = 84%) is high and indicates low reliability.
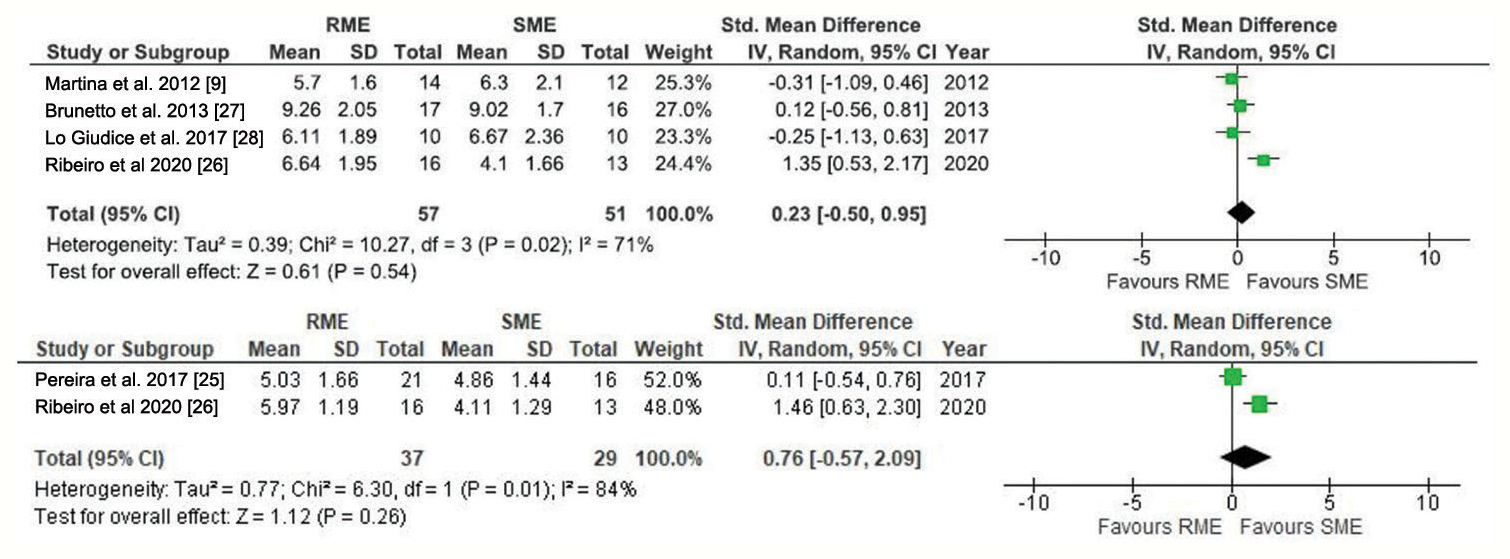
- Random effects meta-analysis of intermolar width at cuspal and alveolar level. RME: Rapid maxillary expansion, SME: Slow maxillary expansion, CI: Confidence interval, SD: Standard deviation.
[Figure 4] is a graphical representation of random-effects meta-analyses done to compare PABW and PNW for two studies.[26,28] With respect to PABW, overall effect P = 0.11 (SMD = 0.63 [95% CI = −0.13–1.38]) indicates no statistically significant differences between groups. Heterogeneity (I2 = 55%) is moderate and indicates fair reliability. With respect to PNW, the overall effect P = 0.007 (SMD = 0.95 [95% CI = 0.25–1.64]) indicates a significant increase with RME. Heterogeneity (I2 = 24%) is low and indicates good reliability.
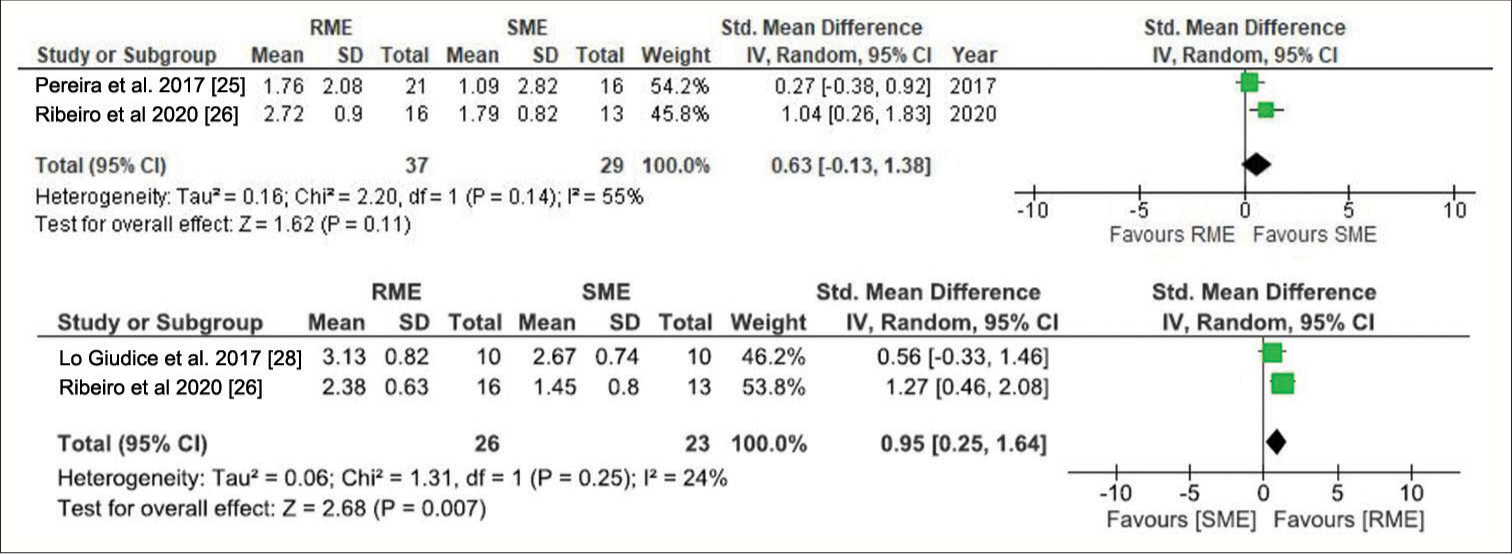
- Random effects meta-analysis of posterior apical base width and posterior nasal width. RME: Rapid maxillary expansion, SME: Slow maxillary expansion, CI: Confidence interval, SD: Standard deviaton.
DISCUSSION
Both RME and SME are equally effective in correcting developing cross-bites in growing patients.[29] Although multiple studies have compared their effectiveness, they have only been evaluated and quantified using dental casts or two-dimensional (2D) radiographs.[30-32] 3D scans, which utilize precise radiographic slices of CBCTs hold great promise in the diagnosis of transverse discrepancies. In addition, it can be used to generate 3D models when combined with appropriate reconstruction software’s and allows for slice-by-slice assessment to detect the extent of the boundaries with expansion.[19,33] The aim of the review was to evaluate treatment effects produced by RME and SME using 3D dental and skeletal landmarks that can provide clinically relevant information regarding the choice of appliance in treating cross-bites.
Primary outcomes – dentoalveolar changes
Both RME and SME showed similar amount of expansion at cuspal (4.1–9.2 mm) and alveolar level (4.1–5.9 mm) and this degree of dental expansion was identical to findings reported by previous studies.[30,34] RME showed significantly greater molar tipping and decreased IMW at apical level compared to SME. These findings seem to suggest the greater bodily translation of molars in slow expansion after accounting for various factors accumulated from clinical experience. First, a rapid increase in force levels directed at the crown of the molars during RME may have generated a fulcrum effect leading to increased tipping. Second, both SME and RME have different assessment time intervals, with the former being longer. A slower rate of expansion coupled with force dissipation across the entire skeletal unit may have permitted the molars to move through the alveolar housing in a bodily manner. These findings reinforce the need for pre-operative assessment of alveolar bone width before any expansion procedure. Suture position and margins of dentoalveolar structures can be analyzed by 3D imaging before expansion. With regard to the reliability of the findings from the review, meta-analysis between parameters could not be performed owing to the varying landmarks utilized for reference.
Uncontrolled tipping movements may increase root proximity to the buccal alveolar bone, promoting root resorption and adverse periodontal effects.[35] Only one paper[27] reported periodontal bone loss in SME and the author speculated that this may be related to the greater bodily displacement of molars and reduced alveolar bending of anchor teeth. Recent studies have however explained the phenomenon of alveolar bone bending to a greater degree and concluded bodily movement to be more effective in increasing effective arch width.[36,37] Moreover, periodontal findings should be assessed with caution when CBCT scans with lower spatial resolution are used due to the reduced image clarity at the assessment site. Using bonded expanders/occlusal splints, which have superior stiffness, may be effective in reducing adverse periodontal outcomes when deciduous molars are involved.
Secondary outcomes-skeletal changes
Martina et al.[9,28] reported that although similar skeletal expansion (about 2.2 mm) occurred at anterior and posterior levels, a minor amount of triangle-shaped expansion was noted at the level of the pterygoid process with RME (detected using 3D radiographs). This may be attributed to a more posterior line of action of the two band expanders employed in RME. However, the inclusion of different activation protocols may have influenced results, as three studies were done until the screw opened 8 mm in both groups, and two studies were done until 2 mm of molar transverse overcorrection was achieved in both groups. Hence, direct comparison of data from included studies is impossible. To make a comparison of different expansion protocols, a simple mathematical model has been proposed to assess the nasal or palatal width as a percentage of IMW.[26] Out of five RCTs, two[28] have assessed skeletal nasal width (as a proportion of IMW) and reported RME to have a significant skeletal nasal width increase. The results of the meta-analysis have shown low heterogeneity and good reliability. Since external walls of the nasal cavity are close to maxillary sutures, they may expand laterally as a result of this expansion. Consequently, RME may be beneficial in improving intranasal capacity, treat nasal deformity, mouth breathing, and obstructive sleep apnea (OSA). Lo Giudice et al.[28] reported an approximate increase of 46% with RME and 33% with SME, whereas Luiz Ulema Ribeiro et al.[26] reported 36% with RME and 35% with SME. Percentage differences between the studies may be due to different expansion protocols and expander designs. Only one study[9] reported RME patients to have higher levels of pain and discomfort, especially during initial activation. This may be due to the difference in the nature of forces–heavy and intermittent in RME, light and continuous in SME. However, these results should be viewed with caution as they have moderate evidence.
Limitations of the review
The main limitation of the review was heterogeneity of the included studies with respect to sample size, expanders utilized, defined anatomical references, outcome measures, and age groups. Moreover, trials with untreated controls and long-term follow-ups were lacking. There is still uncertainty in the evidence regarding the rate of skeletal expansion between the two types as well as the type of tooth movement. To establish evidence-based conclusions, further research should concentrate more on adverse effects such as root resorption, fenestrations, dehiscence, and bone loss.
CONCLUSION
A moderate level of evidence exists to support the 3D assessment of dentoskeletal changes between RME and SME. Similar amounts of dental (IMW) and skeletal (anterior and posterior maxillary width) were observed with both expansion modalities.
RME showed greater molar tipping and posterior skeletal nasal width increase suggesting greater bodily expansion in SME. RME is recommended when molar tipping is necessary to correct developing cross-bites whereas SME is advised when greater arch width development is needed in young children.
RME can be the method of choice in treating patients with OSA.
Acknowledgments
All authors have equal contribution in bringing out this research.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- An RCT on clinical effectiveness and cost analysis of correction of unilateral posterior crossbite with functional shift in specialist and general dentistry. Eur J Orthod. 2020;42:44-51.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior crossbite In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2020.
- [Google Scholar]
- Prevalence and associated factors for the development of anterior open bite and posterior crossbite in the primary dentition. Braz Dent J. 2014;25:336-42.
- [CrossRef] [PubMed] [Google Scholar]
- Occlusal status and prevalence of occlusal malocclusion traits among 9-year-old schoolchildren. Eur J Orthod. 2009;31:294-9.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors and predictors of crossbite at children. Rev Med Chir Soc Med Nat Iasi. 2015;119:564-71.
- [Google Scholar]
- Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8-9.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal and dental contributions to posterior crossbites. Angle Orthod. 2003;73:515-24.
- [Google Scholar]
- Dentofacial orthopedics with functional appliances St. Louis: Mosby Incorporated; 1997.
- [Google Scholar]
- Transverse changes determined by rapid and slow maxillary expansion--a low-dose CT-based randomized controlled trial. Orthod Craniofac Res. 2012;15:159-68.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior crossbite and functional changes. A systematic review. Angle Orthod. 2009;79:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in condylar postition and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111:410-8.
- [CrossRef] [PubMed] [Google Scholar]
- Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 1975;68:42-54.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment response and stability of slow maxillary expansion using Haas, hyrax, and quad-helix appliances: A retrospective study. Am J Orthod Dentofacial Orthop. 2009;136:331-9.
- [CrossRef] [PubMed] [Google Scholar]
- Slow maxillary expansion. A clinical study of the skeletal versus dental response to low-magnitude force. Am J Orthod. 1978;73:121-41.
- [CrossRef] [PubMed] [Google Scholar]
- Relapse following maxillary expansion. A study of twenty-five consecutive cases. Am J Orthod. 1983;83:56-61.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41-66.
- [CrossRef] [PubMed] [Google Scholar]
- Frontal cephalometric comparative study of dentoskeletal effects produced by three types of maxillary expansions. Rev Dent Press Ortod Ortop Facial. 2002;7:27-47.
- [Google Scholar]
- Radiographic cephalometry: From basics to 3-D imaging London: Quintessence Publishing Company; 2006.
- [CrossRef] [Google Scholar]
- Recent advances in imaging technologies in dentistry. World J Radiol. 2014;6:794-807.
- [CrossRef] [PubMed] [Google Scholar]
- A computed tomographic assessment of maxillary movement induced by rapid expansion-a pilot study. Eur J Orthod. 1982;4:123-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75-80.
- [Google Scholar]
- Three-dimensional imaging and software advances in orthodontics London: IntechOpen; 2012.
- [CrossRef] [Google Scholar]
- Cone beam computed tomography in orthodontics: Indications, insights, and innovations United States: John Wiley & Sons; 2014.
- [CrossRef] [Google Scholar]
- RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the rapid and slow maxillary expansion using cone-beam computed tomography: A randomized clinical trial. Dental Press J Orthod. 2017;22:61-8.
- [CrossRef] [PubMed] [Google Scholar]
- A preliminary 3-D comparison of rapid and slow maxillary expansion in children: A randomized clinical trial. Int J Paediatr Dent. 2020;30:349-59.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: A clinical trial study. Am J Orthod Dentofacial Orthop. 2013;143:633-44.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of rapid vs slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur J Paediatr Dent. 2017;18:299-304.
- [Google Scholar]
- Expansion of maxillary arches with crossbite: A systematic review of RCTs in the last 12 years. Eur J Orthod. 2013;35:29-37.
- [CrossRef] [PubMed] [Google Scholar]
- Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2016;43:543-64.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between RME, SME and Leaf Expander in growing patients: A retrospective postero-anterior cephalometric study. Eur J Paediatr Dent. 2018;19:199-204.
- [Google Scholar]
- Long-term skeletal changes with rapid maxillary expansion: A systematic review. Angle Orthod. 2005;75:1046-52.
- [Google Scholar]
- Quantitation of transverse maxillary dimensions using computed tomography: A methodological and reproducibility study. Eur J Orthod. 2004;26:209-15.
- [CrossRef] [PubMed] [Google Scholar]
- Dento-skeletal effects produced by rapid versus slow maxillary expansion using fixed jackscrew expanders: A systematic review and meta-analysis. Eur J Orthod. 2021;43:301-12.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2012;82:488-94.
- [CrossRef] [PubMed] [Google Scholar]
- Identifying cortical plate inclination as a parameter to re-assess transverse discrepancies in untreated adults with different vertical facial heights-A retrospective CBCT study. Orthod Craniofac Res. 2022;25:219-25.
- [CrossRef] [PubMed] [Google Scholar]
- Is the buccal alveolar bone less affected by mini-implant assisted rapid palatal expansion than by conventional rapid palatal expansion? - A systematic review and meta-analysis. Orthod Craniofac Res. 2020;23:237-49.
- [CrossRef] [PubMed] [Google Scholar]







