Translate this page into:
The influence of recommended mouthwashes against coronavirus disease 2019 on the shear bond strength of orthodontic brackets
*Corresponding author: Department of Orthodontics, Faculty of Dentistry, Mahidol University, Bangkok, Thailand. theerasak.nak@mahidol.ac.th
-
Received: ,
Accepted: ,
How to cite this article: Bunjerdjin P, Chintavalakorn R, Tancharoen S, Sipiyaruk K, Nakornnoi T. The influence of recommended mouthwashes against coronavirus disease 2019 on the shear bond strength of orthodontic brackets. APOS Trends Orthod. doi: 10.25259/APOS_97_2024
Abstract
Objective:
To assess the effect of recommended mouthwashes used for coronavirus disease 2019 (COVID-19) prevention on the shear bond strength (SBS) of orthodontic brackets.
Materials and Methods:
Sixty extracted human maxillary premolars were bonded with metal brackets (3M Unitek, California, USA) using an orthodontic bonding agent (Transbond XT, 3M Unitek, California, USA). The teeth were then randomly allocated into four groups (n = 15) to undergo rinsing with 1% hydrogen peroxide (H2O2), 0.5% povidone-iodine (PVP-I), and alcohol mouthwash for 30 s twice daily over 4 weeks, with immersion in artificial saliva during the remaining time. The control group was immersed in artificial saliva throughout the study for comparison. SBS was evaluated using a universal testing machine, and the adhesive remnant index (ARI) score was assessed. Data were analyzed using one-way analysis of variance followed by the Bonferroni test and the Chi-square test, respectively.
Results:
In comparison to the control groups (13.04 ± 3.55 Megapascal [MPa]), alcohol mouthwash showed a significantly lower SBS (10.14 ± 1.91 MPa). However, there were no statistically significant differences observed in the H2O2 (12.65 ± 2.73 MPa) and PVP-I (12.56 ± 2.70 MPa) groups. The ARI scores revealed no significant differences among the groups.
Conclusion:
The use of 1% H2O2 and 0.5% PVP-I mouthwashes did not affect SBS, suggesting their viability for pre-procedural use in COVID-19 prevention during fixed orthodontic treatment. However, caution is advised when using alcohol mouthwash due to its negative impact on SBS.
Keywords
Mouthwashes
Coronavirus disease 2019
Shear bond strength
INTRODUCTION
The emergence of the coronavirus disease 2019 (COVID-19) pandemic has evoked significant concern within global health systems, primarily due to the high transmissibility of the virus. It spreads easily through aerosols, droplets, or direct contact with respiratory secretions from infected individuals. Dental professionals face heightened vulnerability due to their proximity to patients’ respiratory tract openings during dental procedures[1] and prolonged exposure to saliva containing a significant load of oral microbes, including the virus.[2,3] Consequently, any dental intervention, particularly orthodontic procedures that may aerosolize contaminated saliva using handpieces and air-water syringes, has the potential to amplify airborne transmission of the virus greatly. Thus, dental professionals must implement comprehensive preventive protocols for infection control within dental settings.
Several oral antiseptic rinses have been recommended in recent studies for use before dental procedures to minimize the transmission of viruses. These include chlorhexidine gluconate, ethanol, essential oils, povidone-iodine (PVP-I), and hydrogen peroxide (H2O2) mouthwashes. While specific clinical studies on the efficacy of these mouthwashes in preventing cross-infection of COVID-19 are lacking, evidence suggests that rinses containing PVP-I and alcohol mouthwashes can reduce the viral load of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in saliva.[4] The use of alcohol antiseptics for 30 s has been shown to reduce the viral load of human coronavirus by over 99.9%.[5]
Similarly, rinsing with 0.2% PVP-I for 30 s has demonstrated the ability to decrease the infectivity of the SARS-CoV-2 virus to undetectable levels. In addition, PVP-I has been found to reduce the viral load in saliva and prevent the attachment of SARS-CoV-2 to oral and nasopharyngeal tissues.[6,7] However, it is crucial to highlight that PVP-I should not be used in patients with abnormal thyroid function or a history of iodine allergy, as well as those with kidney disease, pregnancy, and children under the age of 6 years.
Exploring alternatives to PVP-I to mitigate these contraindications is essential to enable a broader population to access the benefits of preprocedural oral rinsing. H2O2 is acknowledged as a potent oxidizer with bactericidal and virucidal properties.[8,9] Recommended by the American Dental Association as a preprocedural mouth rinse option, H2O2 holds promise against COVID-19 due to its susceptibility to oxidation. Its mechanism involves disrupting lipid membranes by generating oxygen free radicals. A recent systematic review highlighted the efficacy of 0.5% H2O2 in inactivating enveloped viruses, such as coronavirus 229E.[10] The use of mouthwash containing 1% H2O2 has also been suggested to diminish the viral load of SARS-CoV-2 in saliva.[11,12] In addition, H2O2 offers several advantages, including easy accessibility, low cost, and a well-established track record in dentistry.[8,9]
The efficacy of fixed orthodontic treatment is contingent upon achieving optimal bond strength between orthodontic brackets and enamel. Effective bonding not only reduces bond failure rates but also contributes to shorter treatment durations and improved orthodontic mechanics. While previously published research highlights the potential prophylactic role of oral rinses in preventing viral disease transmission; there is a concern regarding their potential adverse effects on bond strength. However, limited research exists on the effects of recently recommended preoperative mouthwashes on the shear bond strength (SBS) of orthodontic brackets. Therefore, the objective of this study was to compare the effects of different mouthwashes recommended during the COVID-19 pandemic on the SBS of orthodontic brackets.
MATERIALS AND METHODS
Sample size calculation
Sample size calculation was conducted utilizing data from the pilot study, with a significance level (α) of 0.05, power (β) of 0.2, variance of means of 0.39, and effect size of 0.20. Accordingly, the study necessitated a sample size of 15 individuals in each group. A total of sixty teeth underwent testing to assess their SBS properties and adhesive remnant index (ARI) scoring [Figure 1].
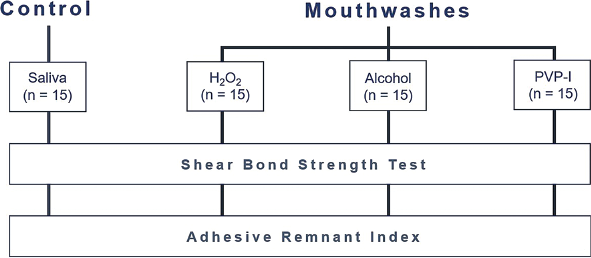
- Experimental flowchart. H2O2: Hydrogen peroxide, PVP-I: Povidone-Iodine.
Preparing the specimens
The extracted, caries-free human premolar teeth were chosen for the study. After removing residual debris, plaque, and calculus, the teeth underwent cleaning and were subsequently immersed in a solution containing 0.1% (weight/volume) thymol to prevent dehydration and inhibit bacterial growth. Each tooth was then sectioned below the cementoenamel junction, and the crowns were securely placed in polyvinyl chloride mounting rings using self-cured acrylic resin. To ensure alignment parallel to the bottom of the rings, the crowns were oriented in a manner that ensured the buccal enamel surfaces were parallel to the force during the SBS test.
Before testing, the buccal surface of each tooth underwent cleansing with fluoride-free pumice and a rubber cup for 10 s. Afterward, the teeth were rinsed for 15 s and dried with compressed air for an additional 15 s. Subsequently, each sample underwent a 30 s etching process on the buccal surface using 37% phosphoric acid. Following etching, the buccal surface was rinsed for 20 s with a water syringe and dried using oil-free compressed air. Metal brackets (3M Unitek, California, USA) were then bonded to the teeth using an orthodontic bonding agent (Transbond XT, 3M Unitek, California, USA) as per the manufacturer’s instructions. To ensure complete adhesion, a 500 g weight was applied to each bracket, and any excess bonding resin around the bracket was removed using a carver. Subsequently, all teeth were randomly assigned into four groups based on the type of mouthwash used:
Group I: Control group (artificial saliva).
Group II: 1% H2O2 mouthwash (K-Lab, Thailand). Hydrogen peroxide (INTEROX FCC 35) was obtained from Solvay Peroxythai Limited, Thailand.
Group III: Alcohol mouthwash – (Listerine®, Johnson and Johnson Consumer Inc., New Jersey, USA).
Group IV: 0.5% PVP-I mouthwash (Betadine® Gargle, Thai Meiji Pharmaceutical, Bangkok, Thailand).
In the control group, the teeth were immersed in artificial saliva for 4 weeks. In the experimental group, the specimens underwent mouthwash rinsing for 30 seconds twice daily, with an 8-hour interval between sessions, over a 4-week period. During the remaining time, the samples were stored in artificial saliva.
SBS test
After the bracket bonding procedure, all specimens were immersed in distilled water at 37°C for 24 h. An occlusogingival load was then applied to each bracket, generating a shear force at the bracket-tooth interface. This was achieved using the flattened end of a steel rod attached to a universal testing machine (Instron Ltd., Buckinghamshire, England) with a crosshead speed of 0.5 mm/min and a 1,000 N load. The force required to shear off the bracket, leading to failure of the bracket-adhesive-enamel complex, was recorded in Newtons and subsequently converted to strength (stress per unit area) in Megapascals (MPa).
ARI
After debonding, both the teeth and brackets were examined under a microscope at ×10 magnification (SZ 40; Olympus, Tokyo, Japan) and scored using the Image-Pro Plus 7.0 software program to assess the amount of resin remaining on the tooth. The ARI was employed to characterize the quantity of resin residue on the tooth surfaces, following the criteria proposed by Artun and Bergland.[13]
The scoring criteria for the ARI were as follows:
0 - Absence of adhesive residue on the tooth,
1 - Less than 50% of the adhesive remaining on the tooth,
2 - More than 50% of the adhesive remaining on the tooth,
3 - Complete presence of adhesive with an impression of the bracket mesh left on the tooth.
Statistical analysis
Statistical analysis was conducted using SPSS (Statistical Package for the Social Sciences) software. The normality of the data was assessed using the Kolmogorov-Smirnov test, which indicated a normal distribution. Descriptive analysis of the data was performed using the mean and standard deviation. The significance level was set at P < 0.05, with a power of analysis of 0.8. SBS data were analyzed for statistical significance using one-way analysis of variance (ANOVA) test followed by Bonferroni post hoc test, with a confidence level of 95%. The ARI scores were analyzed using the Chi-square test.
RESULTS
On comparing the three different mouth rinses with the control group, the artificial saliva group exhibited the highest mean SBS at 13.04 ± 3.55 MPa, followed by the H2O2 group with 12.65 ± 2.73 MPa, the PVP-I group with 12.56 ± 2.70 MPa, and the lowest SBS was observed in the alcohol group with 10.14 ± 1.91 MPa. Statistical analysis revealed significant differences in SBS among the various mouthwash groups (P < 0.05). The alcohol group demonstrated significantly lower SBS (P < 0.05) compared to the control group. However, no statistically significant difference was observed between the control, H2O2, and PVP-I groups [Figure 2].
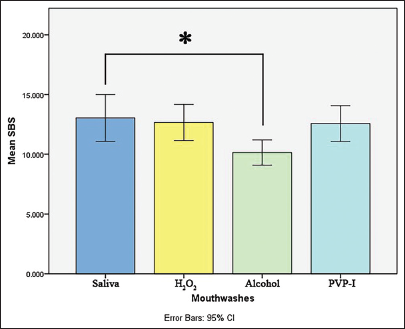
- Shear bond strength (Megapascal) of the bracket exposed to different mouthwashes. The alcohol group showed significantly lower SBS than the artificial saliva group (*P < 0.05). SBS: Shear Bond Strength; H2O2: Hydrogen Peroxide, PVP-I: Povidone-Iodine, CI: Confidence Interval.
The distribution and percentages of ARI scores are detailed in [Table 1]. The Chi-square test revealed no significant differences among the four groups. In all groups, ARI scores of 1 and 2 were the most frequent. Interestingly, ARI score 3 was predominantly observed in the saliva group, while ARI score 0 was most prevalent in the alcohol group.
| Groups | ARI scores | |||
|---|---|---|---|---|
| 0 (%) | 1 (%) | 2 (%) | 3 (%) | |
| I: Saliva | 0 (0) | 5 (33.33) | 6 (40) | 4 (26.67) |
| II: H2O2 | 1 (6.67) | 8 (53.33) | 4 (26.67) | 2 (13.33) |
| III: Alcohol mouth rinse | 4 (26.67) | 7 (46.67) | 4 (26.67) | 0 (0) |
| IV: PVP-I | 2 (13.33) | 5 (33.33) | 5 (33.33) | 3 (20) |
This table presents the frequency distribution of the ARI in the study groups (n=15). Statistical analysis was conducted using a Chi-square test (χ2). ARI: Adhesive remnant index, H2O2: Hydrogen peroxide, PVP-I: Povidone-Iodine
DISCUSSION
During the COVID-19 pandemic, various types of mouthwash, including PVP-I, H2O2, and alcohol, have been recommended to minimize viral transmission in dental settings. This study aimed to assess the impact of these pre-procedural mouthwashes on the SBS of orthodontic brackets. The findings revealed that the use of mouthwashes resulted in decreased SBS, with a significant reduction observed in the alcohol group. Consistent with previous in vitro studies,[14,15] the SBS in the alcohol-containing mouthwash group was lower compared to other mouthwash groups. In addition, research by Lee et al.[16] demonstrated that a 75% ethanol solution can reduce SBS by 30–50% compared to water-stored specimens, attributed to ethanol diffusion-induced microcracking in composite material.[17] The ethanol content in mouth rinses has been observed to soften the composite resin used for bonding orthodontic brackets and dissolve its bisphenol A glycidyl methacrylate component, potentially explaining the observed decrease in SBS following the use of alcohol-containing mouth rinses.[14,18] Despite the utilization of an alcohol mouthwash containing 21.6% ethanol in our study, it exhibited adverse effects on the SBS of orthodontic brackets. Therefore, there is a need for concern regarding the use of alcohol-containing mouthwashes in patients undergoing orthodontic treatment.
Despite the observed decrease in SBS following the use of preprocedural mouthwashes, our investigation revealed that the application of H2O2 and PVP-I did not have an adverse effect on the SBS of orthodontic brackets. This finding is consistent with the study conducted by Ghobadi et al.[19] who suggested that H2O2 and PVP-I mouthwashes may serve as alternatives for orthodontic patients seeking antiviral properties against COVID-19 without compromising the SBS of metal orthodontic brackets. In contrast, previous studies have demonstrated that the use of 1.5% H2O2 and 0.2% PVP-I before bracket bonding leads to a reduction in SBS.[20,21] They observed a thin hybrid layer with short resin tags in the H2O2 groups, while the PVP-I groups exhibited many gaps in the hybrid layer with diminished resin tag formation.[20] These discrepancies in outcomes may be attributed to variations in testing protocols employed across studies, thereby influencing the observed results. In our study, brackets were bonded before exposure to H2O2 and PVP-I mouthwashes to simulate the rinsing process between orthodontic adjustment visits. This approach aimed to provide insights into the effects of these mouthwashes on SBS under conditions representative of clinical practice.
The success of fixed orthodontic treatment critically depends on achieving an optimal bond strength between orthodontic brackets and enamel. Excessive bond strength risks damaging enamel during debonding, while insufficient strength may lead to bracket detachment during treatment. Hence, determining the appropriate value of bond strength is essential to prevent these complications. Reynolds and von Fraunhofer[22] proposed a SBS range of 6–8 MPa for clinical applicability, while Diedrich[23] recommended a range of 5–10 MPa for orthodontic bracket placement. Our study demonstrated that the bond strength of all groups fell within this clinically acceptable range. Despite alcohol-containing mouthwashes causing a significant reduction in the SBS of orthodontic composites, this decrease remains within acceptable limits. Thus, the use of alcohol-containing mouthwashes could be deemed acceptable within defined parameters.
The ARI could serve as a valuable indicator of adhesion failure. When such failure occurs between the bracket and the adhesive material, it can potentially safeguard the enamel surface from damage during bracket debonding. However, this may prolong treatment duration as it necessitates additional time for the removal of residual adhesive. Conversely, if adhesion failure occurs between the enamel surface and the adhesive material, even minimal residual adhesive material can lead to enamel surface damage during bracket debonding. Our findings indicated that the ARI score of 0 was most prevalent in the alcohol mouthwash group, while other groups tended to have higher ARI scores, indicating more composite material remaining on the enamel surface after debonding. Although less adhesive remaining on the tooth surface after debonding may facilitate more efficient cleanup,[24,25] it also poses a greater risk of tooth surface damage, including enamel crack and fracture. Therefore, a fracture occurring in the adhesive may be preferable to enamel failure, as it reduces the risk of damage to the tooth surface. However, it is important to note that the ARI does not necessarily correlate with the SBS value of the adhesive.[26]
The strength of this study lies in its comprehensive comparative analysis of three distinct mouthwashes – an alcohol-containing mouthwash, H2O2, and PVP-I – and their effects on the SBS of orthodontic brackets within a uniform experimental framework. By evaluating these agents under standardized conditions, the study enables clinicians to make more informed decisions regarding preprocedural mouthwash selection. In addition, the exploration of alternatives to alcohol-based solutions broadens the scope of recommended antiviral agents in dental settings. This diversification is crucial for patients who are sensitive to alcohol and for practices aiming to minimize the use of alcohol-based products. The findings demonstrate that effective preprocedural mouthwashes can be used without compromising the integrity of orthodontic treatments, thereby achieving a critical balance between infection control and treatment efficacy during the pandemic.
While our current study provided valuable insights into the impact of preprocedural mouthwashes on orthodontic bracket bond strength, its primary limitation lies in the difficulty of comparing an in vitro investigation with clinical practice conditions. Factors such as temperature, moisture, and chemical interactions present in saliva can significantly influence the effects of mouth rinses on SBS. Saliva has the potential to dilute or buffer mouth rinse solutions, and the salivary pellicle may offer a protective effect. In addition, the absence of mechanical stresses from mastication and oral hygiene practices in vitro means that factors influencing bracket longevity and performance are not fully represented. [27,28] Recognizing these limitations is essential for the accurate interpretation of our findings and underscores the need for cautious application to clinical scenarios. Consequently, extensive clinical trials conducted over extended durations are necessary to fully evaluate the in vitro effects of preprocedural mouth rinses on bond strength and bracket failure rates in orthodontic patients. In addition, further investigations with varying bonding systems and different concentrations of mouthwashes would provide valuable insights.
CONCLUSION
The alcohol mouthwash showed the lowest SBS, indicating caution in its use during fixed orthodontic treatment due to its potential to compromise bond strength. Conversely, 1% H2O2 and 0.5% PVP-I mouthwashes did not negatively affect the SBS of metal orthodontic brackets. This suggests that they could be viable alternatives for orthodontic patients seeking antiviral properties against COVID-19.
Ethical approval
The research/study was approved by the Institutional Review Board at the Faculty of Dentistry/Faculty of Pharmacy, Mahidol University, number COE.No.MU-DT/PY-IRB 2021/018.2106, dated June 21, 2021.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429-37.
- [CrossRef] [PubMed] [Google Scholar]
- Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71:841-3.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical significance of a high SARS-CoV-2 viral load in the saliva. J Korean Med Sci. 2020;35:195.
- [CrossRef] [PubMed] [Google Scholar]
- Early viral clearance among COVID-19 patients when gargling with povidone-iodine and essential oils: A clinical trial. Int Med J. 2020;27:651-4.
- [CrossRef] [Google Scholar]
- Lowering the transmission and spread of human coronavirus. J Med Virol. 2021;93:1605-12.
- [CrossRef] [PubMed] [Google Scholar]
- Can povidone iodine gargle/mouthrinse inactivate SARS-CoV-2 and decrease the risk of nosocomial and community transmission during the COVID-19 pandemic? An evidence-based update. Jpn Dent Sci Rev. 2021;57:39-45.
- [CrossRef] [PubMed] [Google Scholar]
- Safety issues relating to the use of hydrogen peroxide in dentistry. Aust Dent J. 2000;45:257-69.
- [CrossRef] [PubMed] [Google Scholar]
- Hydrogen peroxide and viral infections: A literature review with research hypothesis definition in relation to the current covid-19 pandemic. Med Hypotheses. 2020;144:109910.
- [CrossRef] [PubMed] [Google Scholar]
- Broad-spectrum microbicidal activity, toxicologic assessment, and materials compatibility of a new generation of accelerated hydrogen peroxide-based environmental surface disinfectant. Am J Infect Control. 2006;34:251-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9.
- [CrossRef] [PubMed] [Google Scholar]
- Is hydrogen peroxide an effective mouthwash for reducing the viral load of SARS-CoV-2 in dental clinics? Saudi Dent J. 2022;34:237-42.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333-40.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of various commercially available mouthrinses on shear bond strength of orthodontic metal brackets: An in vitro study. Indian J Dent Res. 2013;24:616-21.
- [CrossRef] [PubMed] [Google Scholar]
- An in vitro evaluation of shear bond strength of orthodontic brackets after mouth rinse. J Contemp Dent Pract. 2018;19:862-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of food and oral simulating fluids on dentine bond and composite strength. J Dent. 1994;22:352-9.
- [CrossRef] [Google Scholar]
- Effect of food and oral simulating fluids on structure of adhesive composite systems. J Dent. 1995;23:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of two mouth rinses on shear bond strength of orthodontic brackets: An in vitro study. Virtual J Orthod. 2011;16:1-7.
- [Google Scholar]
- The effect of hydrogen peroxide and povidone-iodine on the shear bond strength of orthodontic brackets: An in vitro study. Open Access Maced J Med Sci. 2022;10:274-80.
- [CrossRef] [Google Scholar]
- How does antiseptic mouthwashes against SARSCOV-2 affect the bond strength of universal adhesive to enamel? Microsc Res Tech. 2022;85:1199-208.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of recommended mouthwashes on the shear bond strength of orthodontic brackets during the COVID-19 pandemic: An in vitro study. Front Dent. 2023;20:42.
- [CrossRef] [Google Scholar]
- Direct bonding of orthodontic attachments to teeth: The relation of adhesive bond strength to gauze mesh size. Br J Orthod. 1976;3:91-5.
- [CrossRef] [PubMed] [Google Scholar]
- Enamel alterations from bracket bonding and debonding: A study with the scanning electron microscope. Am J Orthod. 1981;79:500-22.
- [CrossRef] [PubMed] [Google Scholar]
- Shear bond strength and residual adhesive after orthodontic bracket debonding. Angle Orthod. 2006;76:694-9.
- [Google Scholar]
- Shear bond strength comparison of two adhesive systems following thermocycling. A new self-etch primer and a resin-modified glass ionomer. Angle Orthod. 2007;77:337-41.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo and in vitro study of the shear bond strength of brackets bonded to enamel using halogen or LED light. World J Orthod. 2009;10:21-8.
- [Google Scholar]
- Shear bond strength and bonding properties of orthodontic and nano adhesives: A comparative in-vitro study. Contemp Clin Dent. 2019;10:600-4.
- [CrossRef] [PubMed] [Google Scholar]
- Bracket bond failures: Incidence and association with different risk factors-a retrospective study. Int J Environ Res Public Health. 2023;20:44-52.
- [CrossRef] [PubMed] [Google Scholar]







