Translate this page into:
A case of maxillary protrusion and excessive overjet treated successfully by implantation of a temporary anchorage device

*Corresponding author: Hitoshi Kawanabe, Department of Oral Growth and Development, Ohu University School of Dentistry, Koriyama, Fukushima, Japan. kawanabe5515@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kawanabe H, Oka S, Fukui K. A case of maxillary protrusion and excessive overjet treated successfully by implantation of a temporary anchorage device. APOS Trends Orthod 2022;12:306-10.
Abstract
This case report describes the treatment of a 15-year-old girl showing Angle’s Class II Division 1 malocclusion with maxillary prognathism and marked labial inclination of the maxillary anterior teeth, which was characterized by a large overjet, overjet occlusion, and mild crowding in the lower jaw. Our treatment completed without root resorption as a result of the combined use of a wire mechanism and anchors has rarely been reported before. The left and right maxillary first premolars were extracted, a temporary anchorage device (TAD) was used for space closure, and oral hygiene maintenance guidance was provided. The total treatment time was approximately 2 years and 7 months. Ideal overjet and overbite relationships were established, and the facial profile improved substantially. The 2-year follow-up assessment showed a morphologically and functionally stable result. For patients with marked maxillary prognathism, orthodontic treatment using TADs enables simultaneous and efficient maxillary anterior tooth retraction and reduction of overjet. Moreover, this treatment has the potential to shorten the treatment duration and contribute to the long-term stability of excessive overjet correction.
Keywords
Excessive overjet
Orthodontic anchorage procedures
Angle’s class II
Tooth movement technique
INTRODUCTION
Adults with maxillary protrusion often arrive at the hospital with a chief complaint of poor esthetics. We demonstrate a simple and fast method of correcting maxillary prognathism caused by the marked labial inclination of the maxilla using a temporary anchorage device (TAD), orthodontic anchor screws, and a lingual multi-bracket appliance with excessive overjet.
CASE REPORT
Diagnosis and etiology
A female patient aged 15 years and 3 months consulted the outpatient clinic of our hospital with a chief complaint of a protruding mouth. She had a convex facial profile and symmetric frontal view, but both the upper and lower lips were protruded [Figure 1]. The upper and lower lips protruded +3 mm and +4 mm, respectively, with respect to the E-line. Cephalometric analysis showed a slight tendency of maxillary prognathism (ANB angle, +4°) [Figure 2 and Table 1]. The U1-FH angle was 134°, and U1 to the facial plane distance was 17 mm, showing marked labial inclination of the anterior maxillary teeth. Clinical examination showed Angle’s Class II molar relationship on both sides [Figure 1]. The overjet was 14.5 mm, and the overbite was 5 mm. Model analysis showed an arch-length discrepancy of +2.0 mm in the maxilla and −3.0 mm in the mandible. No abnormality of the temporomandibular joint was identified in the panoramic radiographs [Figure 2].
| Measurement | Pre-treatment | Post-treatment |
|---|---|---|
| 15 years 3 months | 18 years 1 month | |
| Angular measurements (°) | ||
| SNA | 80 | 79.5 |
| SNB | 76 | 76 |
| ANB | 4 | 3.5 |
| MP angle | 25.5 | 28 |
| IMPA | 94 | 96 |
| U1-FH | 134 | 103.5 |
| L1-FH | 56 | 54 |
| Linear (mm) | ||
| U1 to facial plane | 17 | 6 |
| L1 to facial plane | 3 | 4 |
| Overjet | 14.5 | 2.5 |
| Overbite | 5 | 2 |
ANB: Angle between the lines AN and NB, L1-FH: L1 to the FH plane, MP: Mandibular plane, IMPA: Incisor mandibular plane angle, SNA: Angle between the lines SN and NA, SNB: Angle between the lines SN and NB, U1-FH: Angle between the axis of the upper incisor and the FH line

- Pre-treatment facial photographs (a and b). The lateral view showed a convex facial type, with the upper lip protruding +3 mm and the lower lip protruding +4 mm with respect to the E-line. The nasolabial angle was 93°. Intraoral photographs after treatment (c-g). Correction of proclined maxillary anterior teeth with an Angle’s Class II Division 1 molar relationship.
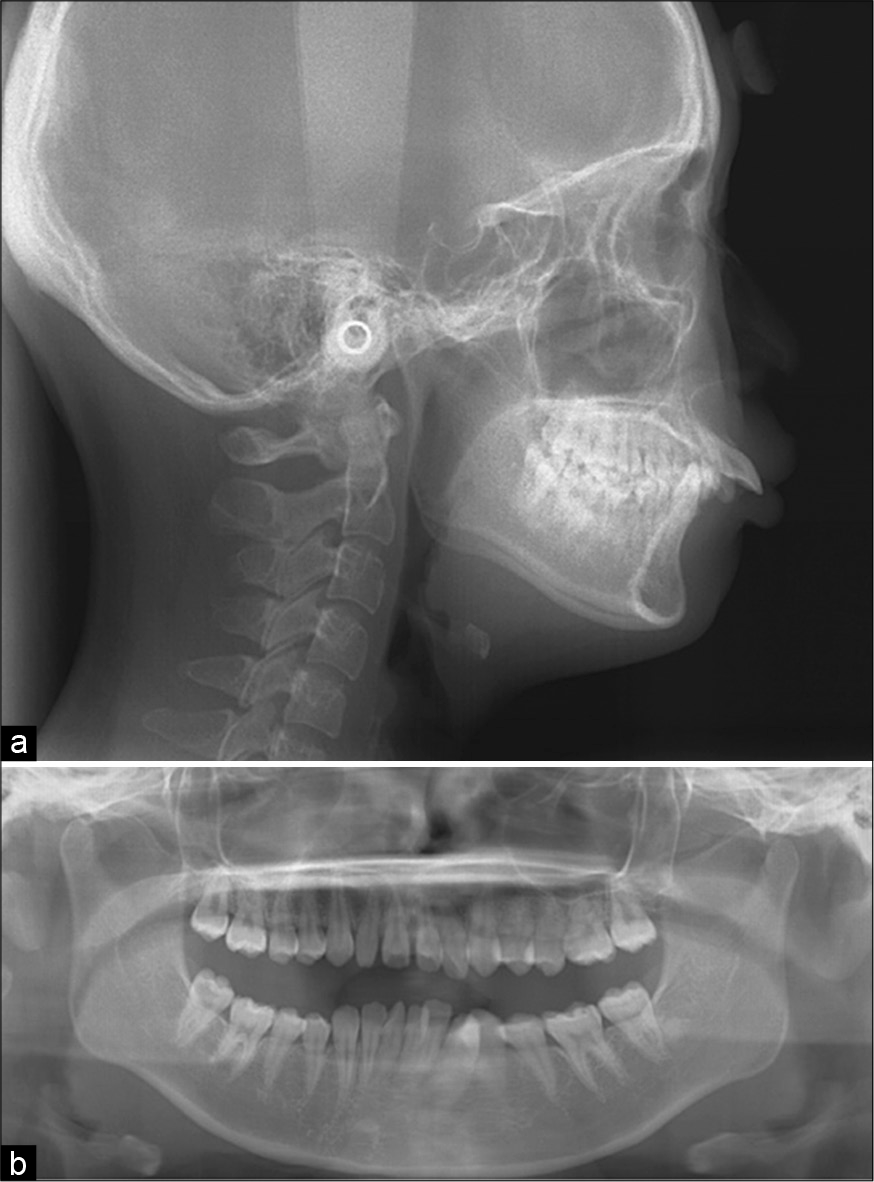
- (a-b) Pre-treatment lateral cephalogram. Proclined anterior maxillary teeth and lip protrusion before surgery. Pretreatment panoramic radiographs. Non-concurrent tooth axis and crowding in the anterior mandibular teeth. No abnormalities in the temporomandibular joint.
The patient was diagnosed with dental maxillary prognathism with mandibular crowding and presented with protrusion of the upper teeth. The patient provided informed consent for treatment and the publication of this case report.
Treatment objectives
The treatment objectives were to retract the anterior maxillary teeth, correct mandibular crowding, obtain a good facial profile, achieve acceptable occlusion with a functional Angle’s Class II molar relationship, and correct facial protrusion to address the patient’s esthetic and social concerns using a lingual multi-bracket appliance. To retract the anterior maxillary teeth, the left and right maxillary first premolars were extracted, and the mandible was treated without extraction.
Treatment alternatives
TADs can efficiently achieve maximum fixation. However, since TAD implantation requires surgery, monitoring for infection is essential. Another treatment method, alveolar osteotomy, can reduce treatment duration, but is invasive.
Treatment progress
Multibracket treatment was initiated in the maxilla. Bilateral maxillary first premolars were extracted. An orthodontic anchor screw (manufactured by Proseed: Dual-top screw; diameter, 1.6 mm; major axis, 8 mm) was inserted between the second premolars and first molars on both sides of the maxilla as a fixing source.
A reverse curve 0.016 × 0.022 stainless steel wire was used and vertical closure was performed. Using the TAD as a fixation source, the mandibular anterior teeth were moved lingually and the crowding of the anterior maxillary teeth was corrected.
For the final detailing, a 0.017 × 0.025 stainless steel wire was used. For retention, a circumferential-type retainer was used for the upper jaw and a canine-fixation-type retainer was used for the lower jaw. The total duration of treatment was 2 years and 7 months.
Treatment results
Retraction of the upper and lower lips significantly improved the facial profile, including the lateral profile. Correction of maxillary anterior protrusion and labial inclination of the mandibular anterior teeth and slight expansion of the mandible improved the excessive overjet. Because of the reduction in the proclination of the anterior maxillary teeth, there was an improvement in lip protrusion [Figure 3]. In the cephalometric analysis, we observed clockwise rotation of the mandible with extrusion of the molars [Figures 3 and 4]. In addition, improvement in the tooth axis was observed by the lingual movement of the anterior maxillary teeth and reduction of the labial inclination of the mandibular anterior teeth [Figure 5]. Although the post-operative panoramic radiographs showed mesial inclination of the maxillary lateral incisors, the overall outcome was satisfactory [Figure 6]. Superposition of cephalograms obtained before and after the treatment showed 0.5 mm extrusion and 1.0 mm mesial movement of the maxillary first molar.

- Post-treatment facial photographs (a and b). The facial profile is a typical Japanese slightly convex profile. The upper and lower lips are 0 mm relative to the E-line, which is an ideal profile. The nasolabial angle is 107°, which is very close to the standard value. Post-treatment intraoral photographs (c-g). 4 years and 5 months after treatment, proper overjet and overbite have been established. An excellent occlusal relationship between the maxilla and mandible is evident. Diagram of the mechanics used in the treatment (h).
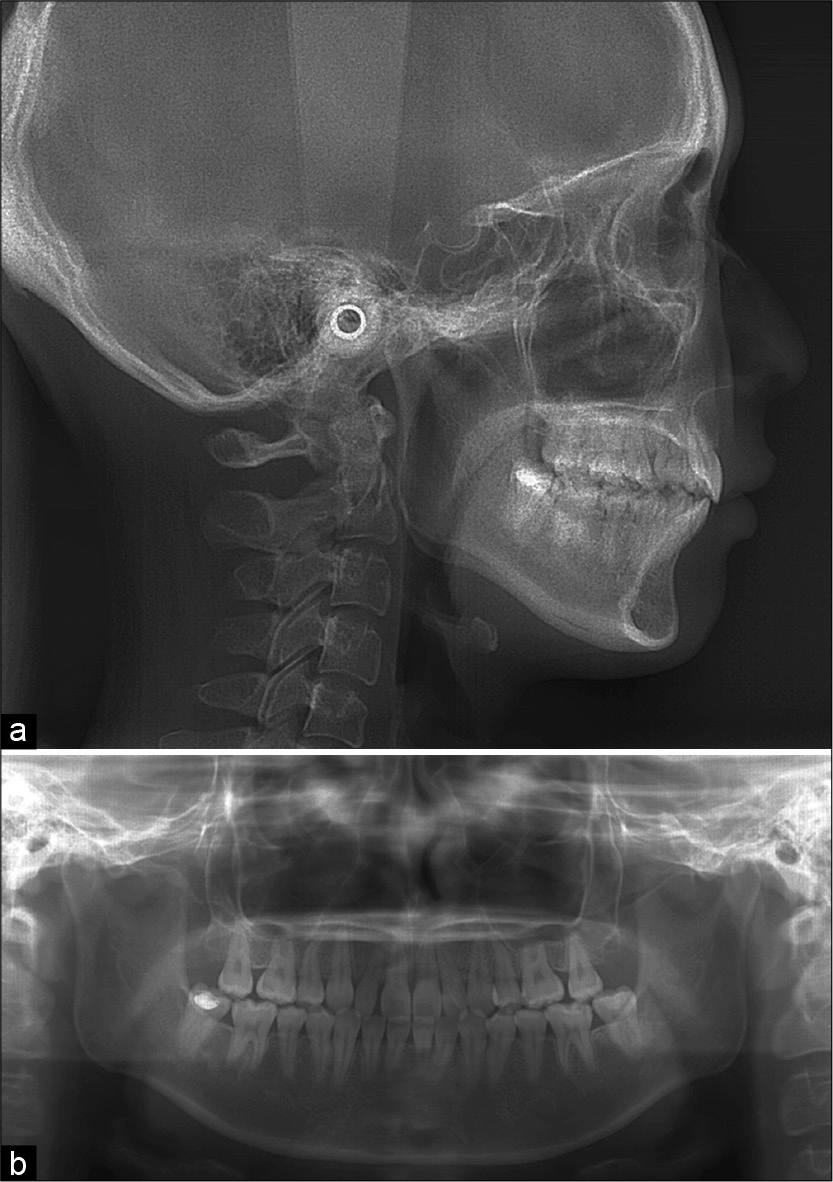
- (a) Post-treatment lateral cephalograms and (b) post-treatment panoramic radiographs. The tooth axes are well-aligned, and parallelism of the roots is evident. The treatment successfully completed without root resorption.
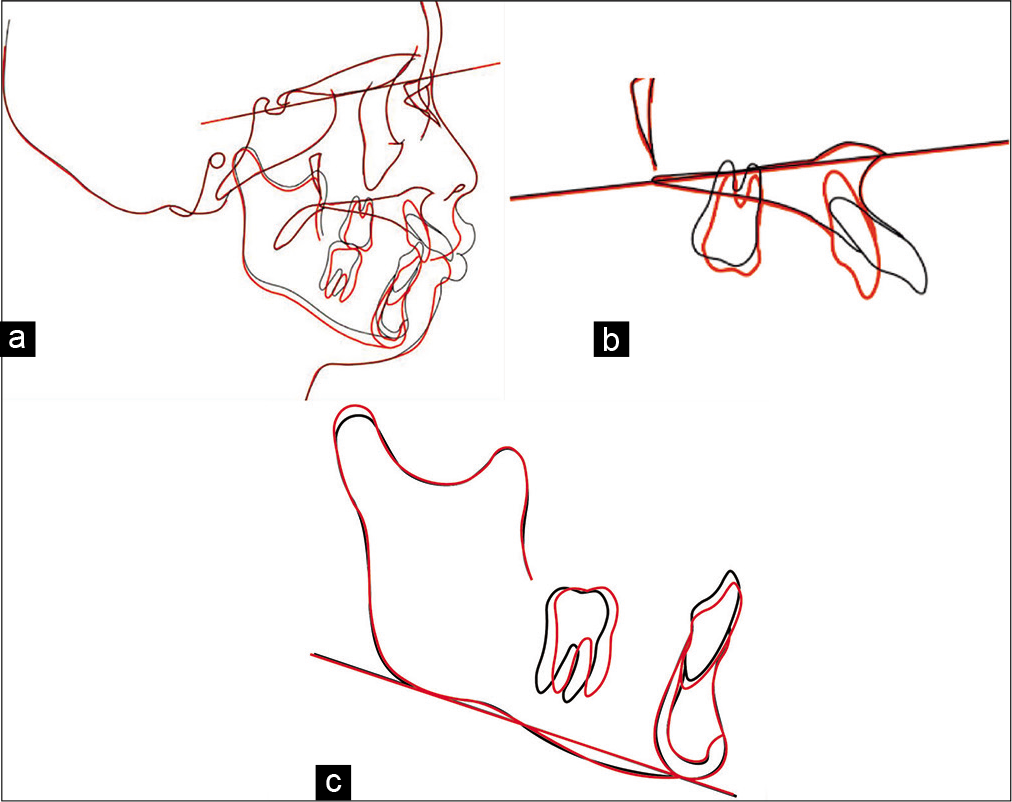
- Cephalometry showing superimposition of the pretreatment (black line) and post-treatment planes (red line). (a) On the sella-G-nasion plane at the sella. (b) On the palatal at the ANS. (c) On the mandibular plane at the mention. Posterior movement of the maxillary anterior teeth was achieved successfully.
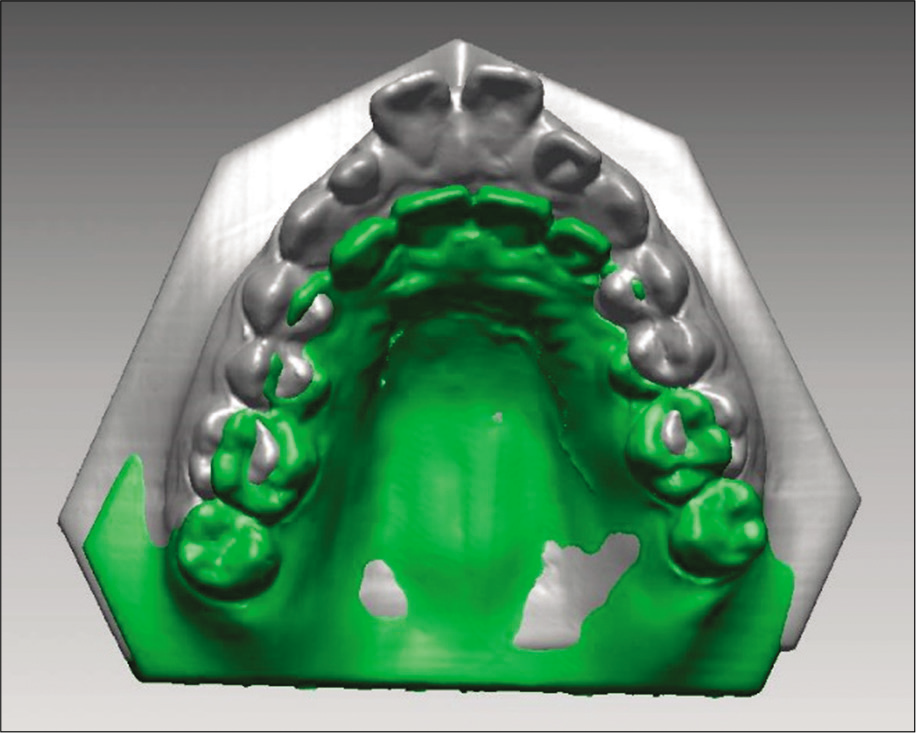
- Superimposed three-dimensional teeth model data. Gray represents the pretreatment data and the green represents the post-treatment data. The superposition of the molars showed that the anterior teeth had been retracted significantly after treatment.
Although a slight labial inclination of the anterior maxillary teeth was observed after 2 years since the initiation of retention treatment, the excellent occlusal state was maintained. Moreover, the patient was satisfied with the treatment.
DISCUSSION
The most notable result in the present case was the change in the lateral profile, as the patient desired. Such decisions on the pace of the treatment plan contributed to changing the profile safely without any need for surgery.
Kuroda et al. reported that the mesial movement of the molars averaged 0.7 mm and the vertical ejection was 0.4 mm using TADs.[1] In the present case as well, the molars protruded by approximately 0.5 mm, as evident from the superimposition before and after the treatment cephalograms, and a slight clockwise rotation of the mandible occurred. The amount of mesial movement was 1.0 mm, which was adequate for maximum fixation. Kawahara et al. reported the use of TADs to retract and reduce the proclination of anterior teeth.[2] Similarly, in our case, improvement in the tooth axis and control of the overbite could be achieved by applying a reducing force simultaneously as the anterior maxillary teeth retracted.
Our results for the improvement in the soft-tissue profile indicated that the lingual movement of the lips occurred with the lingual movement of the teeth. In this case, the anterior maxillary teeth were retracted by 11.5 mm, while the upper lip was retracted by 5 mm, and the results showed no statistically significant difference. For the E-Line, Motohashi et al. reported that the lower lip is 2.60 ± 1.65 mm, which is the preferred lateral form for Japanese people.[3] In the present case, good results were obtained for the position of the anterior teeth relative to the E-Line from +4 mm to 0 mm and from +3 mm to 0 mm for the upper and lower lips, respectively.
More than 2 years have passed since the final prosthesis, and marked improvements considered satisfactory by both the treatment team and the patient have been noted in this period.
CONCLUSION
For patients with marked maxillary prognathism, orthodontic treatment using TADs enables efficient simultaneous maxillary anterior tooth retraction and reduction of proclination. Thus, we established functional occlusion and an excellent soft-tissue morphology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Class II malocclusion treated with miniscrew anchorage: Comparison with traditional orthodontic mechanics outcomes. Am J Orthod Dentofacial Orthop. 2009;135:302-9.
- [CrossRef] [PubMed] [Google Scholar]
- A case report of bimaxillary protrusion with Angle Class I using temporary anchorage device (TAD) [Article in Japanese] Matusmoto Dent. 2018;44:7-17.
- [Google Scholar]
- A study on preferred aspects based on E-Line (1st report) [Article in Japanese] Dentistry. 1977;64:988-95.
- [Google Scholar]






