Translate this page into:
A severe skeletal Class III malocclusion treated with Le Fort I combined with sagittal split ramus osteotomy, mandibular body ostectomy and tongue reduction surgery. A case report

*Corresponding author: Carmen Karadeniz, Private practice, Brisbane, Queensland, Australia. gonzales_carmenb@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Hotokezaka H, Karadeniz C, Hotokezaka Y, Matsuo T, Yoshida N. A severe skeletal Class III malocclusion treated with Le Fort I combined with sagittal split ramus osteotomy, mandibular body ostectomy and tongue reduction surgery. A case report. APOS Trends Orthod 2022;12:221-9.
Abstract
This case report describes the orthodontic-orthognathic management of a 17-year-old male patient with extremely severe skeletal Class III malocclusion due to a marked mandibular protrusion with a small and narrowed upper jaw which increased the remarkable concave facial profile. Dental articulation was entirely lacking, resulting in great difficulty in masticating food. A two-jaw surgery combined with mandibular body ostectomy was performed to correct mandibular asymmetry and the severe sagittal skeletal discrepancy (Wits appraisal –36.5 mm and ANB angle –14.3°). Bi-maxillary surgery was performed in two-stages; the first surgery consisted of maxillary advancement with Le Fort I osteotomy followed by a second surgery where a combination of sagittal split ramus osteotomy (SSRO) and mandibular body ostectomy was performed to correct the severe mandibular prognathism. A partial glossectomy was also carried out to address macroglossia. After a total treatment time of 32 months, a Class I occlusion with a favorable facial profile and lip competence were obtained. The occlusion was made approximately ideal, and mastication improved remarkably. Three years after retention, the occlusion was stable and no relapse was observed. The patient’s complaints and orthodontic problems were completely resolved. Therefore, a combination of two-jaw surgeries with Le Fort I maxillary osteotomy, mandibular SSRO, mandibular ostectomy, and glossectomy may be a viable option in the correction of extremely severe anteroposterior skeletal discrepancy.
Keywords
Severe skeletal
Class III
Orthodontic/orthognatic
Management
INTRODUCTION
Combined orthodontic and orthognathic surgical treatment has been reported for the correction of skeletal Class III discrepancies with mandibular prognathism. Sagittal split ramus osteotomy (SSRO) is the popular method for treating mild-to-moderate mandibular prognathism. However, two-jaw surgery has been by far the most common type of orthognathic surgical treatment.[1,2] A combination of Le Fort I osteotomy for maxillary advancement and SSRO, are often required for adult patients with excessive anteroposterior skeletal Class III discrepancy, because such cases frequently have skeletal deformities combining the maxilla and mandible. Nevertheless, excessive mandibular setback causes a stretching of the masticatory muscles, which can result in the forward relapse of mandible.[3,4] Furthermore, excessive mandibular setback has been associated with narrowing of airway dimensions[5,6] However, a direct cause-and-effect relationship between the mandibular setback and development of sleep apnea has not been clearly established.[7]
Other additional ostectomies in combination, that is, Le Fort I and SSRO two-jaw surgery, have been proposed to reduce a large amount of mandibular setback when correcting an excessive anteroposterior discrepancy. A mandibular setback of 15 mm might be the maximum in patients with narrow rami.[8] Practically, bimaxillary surgery is usually applied for cases with a mandibular setback in excess of 15–20 mm.[9] However, the method is not fully established in cases with anteroposterior discrepancy of more than 20 mm, because such severe mandibular setback cases are rarely seen in real clinical situations.[9,10]
In this case report, we describe a combination of Le Fort I osteotomy for maxillary advancement, SSRO, mandibular body ostectomies and reduction glossectomy performed in a patient diagnosed with extremely severe skeletal Class III malocclusion who had an anteroposterior discrepancy of Wits appraisal –36.5 mm, ANB angle –14.3° and facial asymmetry.
DIAGNOSIS AND ETIOLOGY
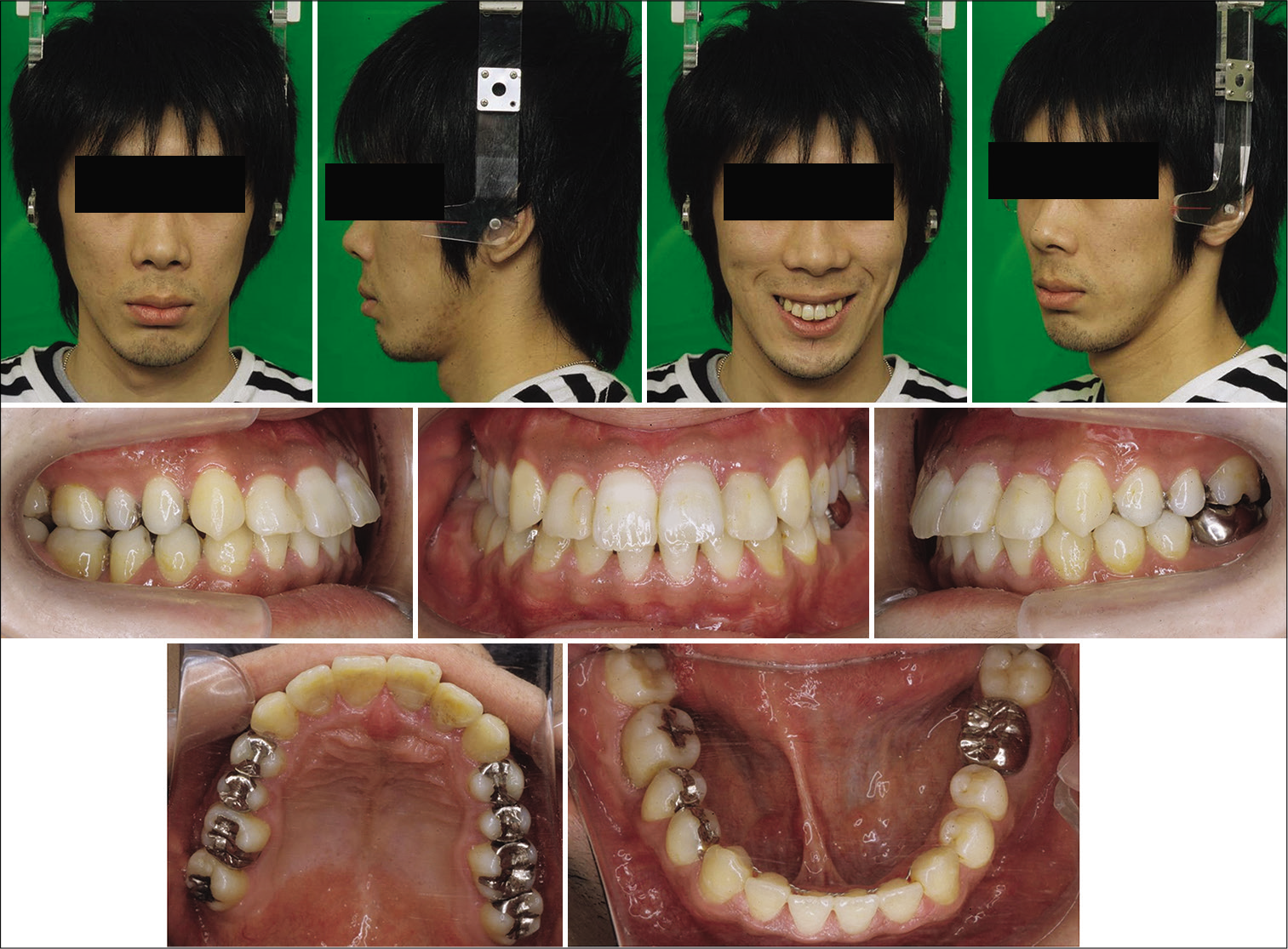
A 17-year-old male presented to the Department of Orthodontics and Dentofacial Orthopedics at Nagasaki University, Graduate School of Biomedical Sciences for treatment. He had noncontributory medical history including acromegaly and his body mass index (BMI) was 16.8 indicating underweight. His chief complaint was difficulty in chewing food due to his “underbite;” and he also wanted to improve his facial appearance. Facial analysis showed an extreme skeletal Class III skeletal pattern with severe mandibular prognathism, maxillary retrusion, anterior and posterior crossbite, lip incompetence, mandibular deviation toward the left side, and an increased lower face height. Intraorally, Angle Class III malocclusion was characterized by anteroposterior discrepancies of 22 mm on the left and 25 mm on the right; a vertical deformity (deep bite) and a transverse deformity (posterior crossbite). The maxillary dental midline was coincident with the facial midline; however, the mandibular dental midline was shifted 6 mm to the left. Overjet and overbite were –19.0 and +9.5 mm, respectively. The intercuspation at centric occlusion was very poor and unstable. Mild crowding (–4 mm) and severe crowding (–14 mm) were present in the mandibular and maxillary arch, respectively.
The panoramic radiographs showed multiple restorations, crowns, and root canal treatments. His oral hygiene was poor, and several secondary caries and gingivitis were observed [Figures 1-3].
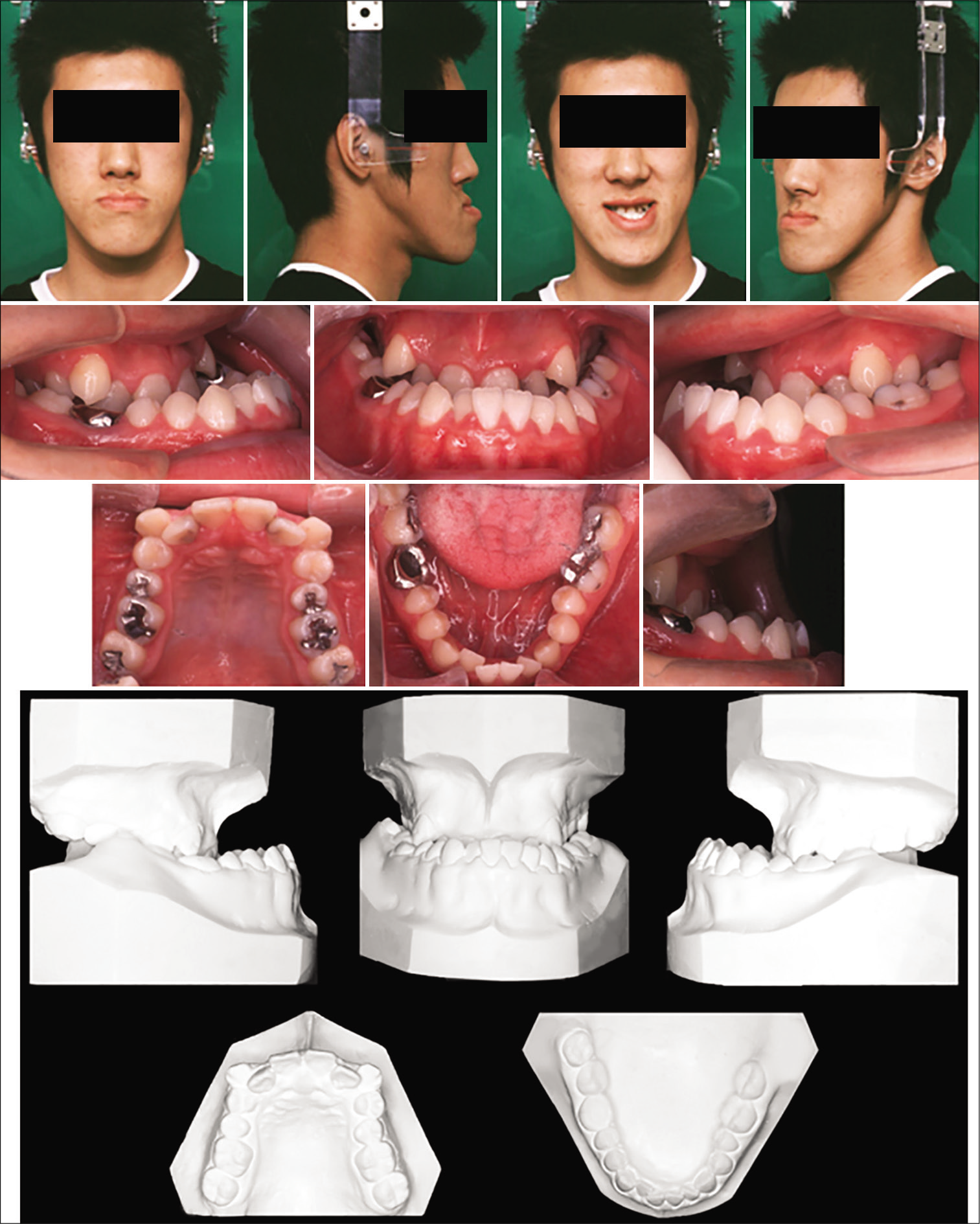
- Pretreatment facial, intraoral photographs, and dental casts.

- Pretreatment radiographs; lateral and posteroanterior cephalograms and panoramic radiographs.
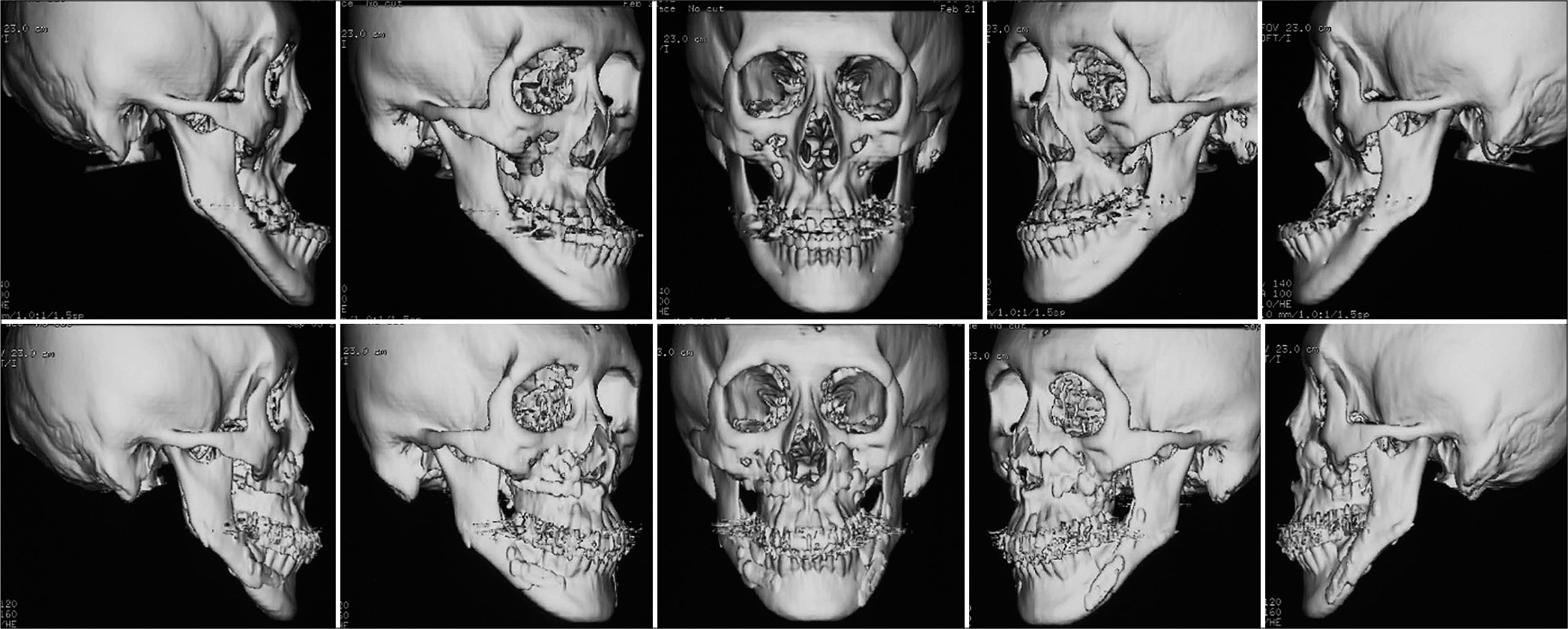
- Presurgery (upper) and Posttreatment (lower) 3D images of CT radiographs.
A lateral and frontal cephalometric analysis confirmed the severe maxillomandibular skeletal discrepancy with a SNA angle of 72.0°, a SNB angle of 86.1°, an ANB angle of –14.1°, and a Wits appraisal of –36.5 mm. The mandibular plane angle was 35.9°, and the gonial angle was 146.1°. The mandibular body length (Pog-Go, 98.4 mm) was increased compared with the ramus length (Cd-Go, 63.6 mm). The mandibular incisors were inclined lingually, at an angle of 60.3° to the mandibular plane. The upper lip was retrusive, and the lower lip was protrusive. The mandible was shifted 6 mm to the left [Figure 3 and Table 1].
| Measurement | Mean±S.D. | Pre treatment | Post treatment |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.8±3.1 | 72.0 | 80.8 |
| SNB (°) | 78.6±3.1 | 86.1 | 75.7 |
| ANB (°) | 3.3±2.7 | –14.1 | 5.1 |
| Wits (mm) | 0.7±2.2 | –36.5 | –11.2 |
| Mandibular plane (°) | 26.3±6.3 | 35.9 | 44.8 |
| Gonial angle (°) | 131.0±5.6 | 146.1 | 151.0 |
| Gn-Cd (mm) | 128.5±4.4 | 154.6 | 135.8 |
| Pog-Go (mm) | 82.1±3.8 | 98.4 | 83.1 |
| Cd-Go (mm) | 69.6±4.9 | 63.6 | 59.1 |
| Dental | |||
| U1 to SN (°)€ | 103.1±5.5 | 102.9 | |
| L1 to mandibular plane (°) | 94.7±7.2 | 60.3 | 76.1 |
| Soft tissue | |||
| Upper lip to E-line (mm) | 1.0±2.0 | –6.7 | 2.7 |
| Lower lip to E-line (mm) | 2.0±3.0 | 5.5 | 4.6 |
Wolford and Cottrell[11] described 18 clinical features of macroglossia to determine whether a tongue reduction is necessary. Eight of these features were observed in this case: (1) a wide, broad, and flat tongue; (2) open bite; (3) mandibular prognathism; (4) Class III malocclusion; (5) chronic posturing of the tongue between the teeth at the rest; (6) buccal tipping of posterior teeth; (7) increased transverse width of dental arch; (8) instability in orthodontic treatment. All these features were observed at the initial evaluation and were still significant following pre-surgical orthodontic treatment. At that point, we reviewed the diagnosis, orthodontic problems, and recommended a tongue reduction surgery.
TREATMENT OBJECTIVES
Based on the cephalometric findings and full orthodontic records, this patient was diagnosed with a skeletal Class III malocclusion with maxillary retrusion and a prognathic mandible. The treatment objectives were as follows: (1) Anteroposterior, correct the skeletal Class III jaw relationship; (2) Vertical, correct the deep bite; (3) Transverse, coordinate the upper and lower dental arches and correct the mandibular deviation; (4) Eliminate dental crowding; (5) Decompensate the mandibular incisors to an upright position; (5) Obtain lip closure at rest.
TREATMENT ALTERNATIVES
The following treatment alternatives including the option and implications of no treatment were discussed with our patient before obtaining informed consent.[12] (1) No treatment would have worsened the patient’s difficulty chewing and would not have addressed patient’s chief complaints. Due to the severity of the class III dentofacial deformity, a two-jaw surgery was considered appropriate. (2) One stage maxillary and mandibular orthognathic surgery, without segmental ostectomies; and (3) two-stage surgeries; the first surgery consisting of Le Fort I maxillary advancement osteotomy followed by a second surgery where a combination of SSRO and mandibular body ostectomy.
Both surgical options included a partial glossectomy. The advantages of option 2 were an overall short treatment time and no ostectomies. However, this treatment option would not be sufficient to achieve the treatment objectives and would have decreased the likelihood of success. On the other hand, option 2 involved a long treatment duration, mandibular ostectomies with the extraction of severely carious mandibular first molars.
Based on the severe midface and mandibular skeletal discrepancies, a two-jaw surgery with a LeFort I osteotomy was deemed the preferred treatment option. In the mandible, due to the extremely severe mandibular prognathism a SSRO and mandibular body ostectomies were necessary to correct the anteroposterior discrepancy. In a conventional orthodontic treatment plan, two maxillary premolar extractions would have been contemplated. However, if the maxillary first premolars were extracted in this case, a maxillo-mandibular movement of more than 30 mm would have been required to correct the excessive sagittal discrepancy. Therefore, a compromised result with proclined upper incisors was considered a reasonable option to reduce the risks and complications of orthognathic surgery.
The following treatment sequence was planned: (1) Decompensation and alignment of the dental arches by preoperative orthodontic treatment; (2) Maxillary advancement (8.0 mm) by a Le Fort I osteotomy; (3) mandibular setback combining two surgical approaches, that is, SSRO and mandibular body ostectomies.
TREATMENT PROGRESS
Pre-surgical orthodontic treatment
The pre-operative orthodontic treatment was performed with pre-adjusted 0.018-inch edgewise full fixed appliances.
Decompensation and alignment of the dental arches were carried out for 16 months.
Surgical procedures
Le Fort I osteotomy was performed with an 8.0 mm advancement by rigid fixation with bone mini plates. A combination surgery with mandibular body ostectomies and SSRO was designed to obtain a total mandibular setback of 17.5 mm. The mandibular body was shortened by 9.0 mm on each side by the ostectomy, and the amount of mandibular setback by SSRO was 10.0 mm to the right and 7.0 mm to the left to correct the facial asymmetry caused by mandibular shift to the left. The mandible on the right side was overcorrected by 2.0 mm to a half unit Class II molar relationship because the amount of posterior movement by SSRO was greater on the right.
Mandibular body ostectomies were performed with extraction of the lower first molars. The neurovascular bundle was carefully preserved, and the anterior and posterior segments were fixed by mini plates. This approach allowed for a telescoping effect that occurs when a narrow anterior segment in the premolar area is retracted to approximate wider posterior segments. Simultaneously, this medial movement with slight compression and rotation of the proximal segments resulted in the correction of the transverse discrepancy. The final inter-molar width between the lower third molars decreased by 4.0 mm by rotating the posterior segments lingually. Intermaxillary fixation by elastics was carried out for 4 weeks.
Tongue reduction surgery
The middle dorsal part of the tongue was resected following the method of Harada and Enomoto.[13] In brief, a wedge-shaped strip along the middle of the tongue and a crescent-shaped strip on the posterior portion of the dorsum were removed [Figure 4]. The total weight of the excised tissue was 9 g. The swelling of the tongue gradually decreased and completely resolved 1 month after tongue reduction surgery.
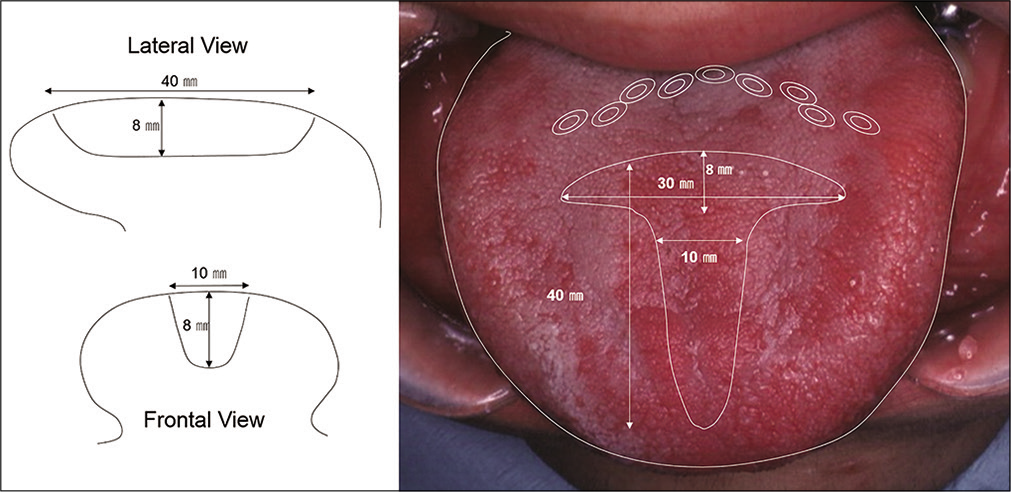
- Scheme of tongue reduction. Illustration demonstrating the incisions for the tongue partial reduction. Dotted lines represent the excised portion of the tongue.
Post-surgical orthodontic treatment
About 6 weeks after the surgery, postsurgical orthodontic treatment was resumed with a maxillary 0.017 × 0.025 SS alloy wire and a mandibular 0.016 NiTi archwire. Orthodontic treatment was completed 14 months after the surgery. The appliances were removed after 32 months of active treatment. Fixed lingual retainers were bonded to the lingual surfaces of the anterior teeth in both arches. A maxillary removable wraparound retainer (Begg retainer) was prescribed to be worn all day except during meals and tooth brushing for the first 6 months and every night thereafter.
TREATMENT RESULTS
The posttreatment photographs showed that facial asymmetry was corrected, and the overall treatment was successful in normalizing the main dental and skeletal relationships. The overcorrected molar relationship was stable, and an acceptable occlusion in all three planes of space was obtained. The mastication was drastically improved, and lip competence at rest was also obtained. The maxillary dental midline coincided with the facial and mandibular midlines. The maxillary incisor exposure was increased at rest and while smiling [Figure 5].
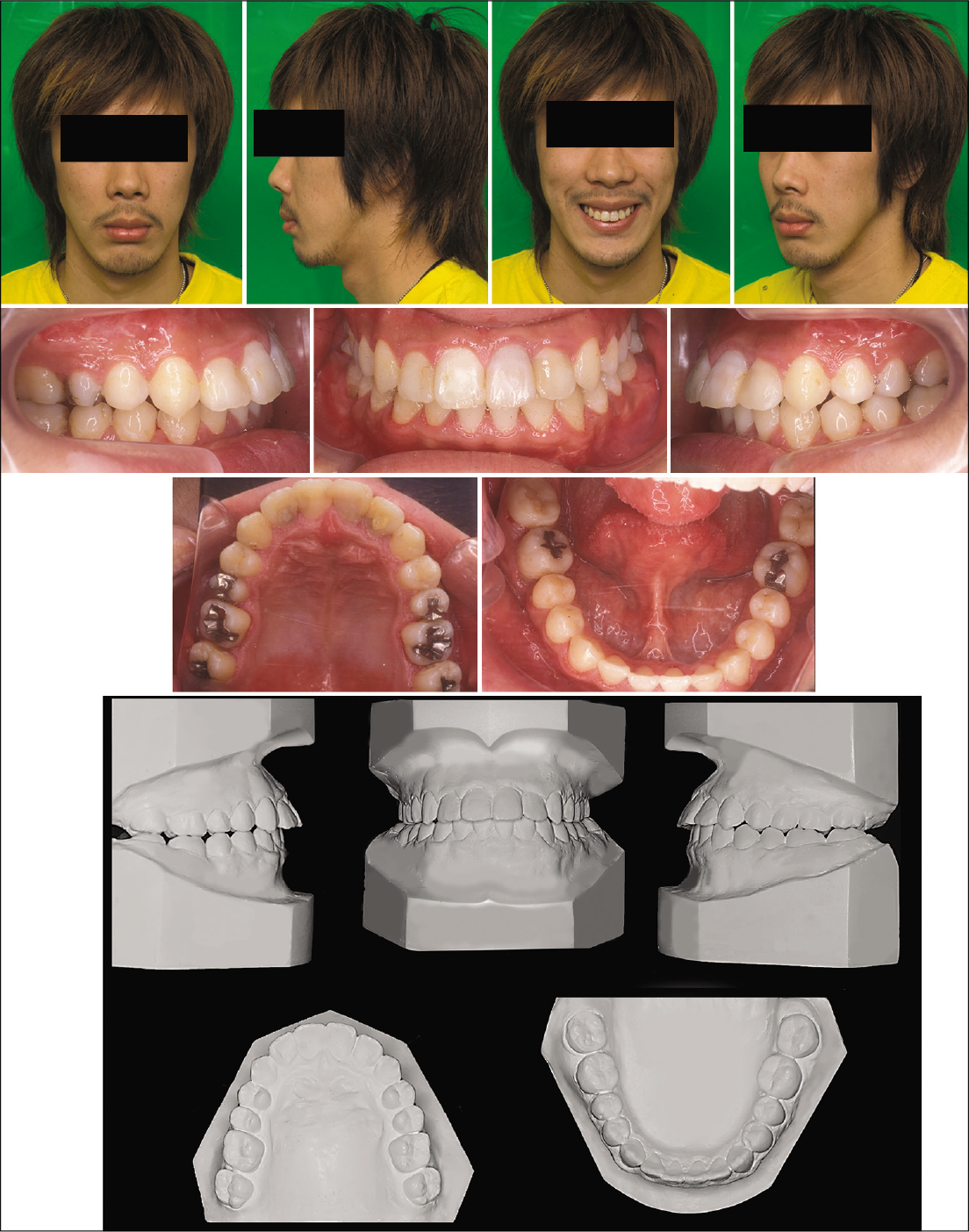
- Posttreatment facial, intraoral photographs and dental casts.
Superimposition of the cephalometric tracings showed that the maxilla was moved 7 mm forward, and the mandible was set back and rotated clockwise. Cephalometric changes included an increase in the ANB angle from –14.1° to +5.1°. The upper incisor to SN plane angle increased from 102.9° to 110.1°. The mandibular length (Cd-Gn) decreased from 154.6 to 135.8 mm [Figures 6 and 7, Table 1].

- Posttreatment radiographs; lateral and posteroanterior cephalograms and panoramic radiographs.
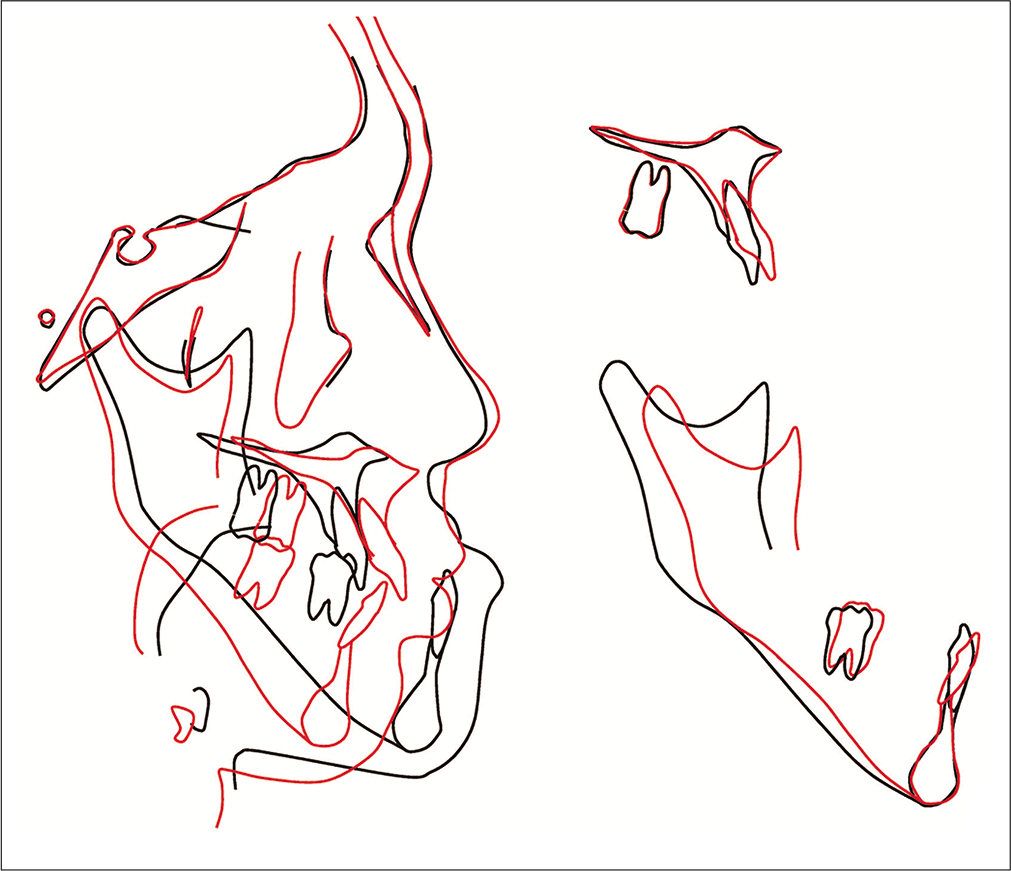
- Superimposition of pretreatment and posttreatment cephalometric tracings. The lower first molar is traced in the pretreatment and the second molar is traced in the posttreatment.
Angle Class I molar and canine relationships were established on the left hand side and a slight surgical overcorrection in the transverse plane led to a half unit Class II molar relationship on the right hand side.
Three years after debonding, the results were stable, and the patient was very satisfied with his mastication, speech and the improvement of his facial appearance [Figures 8 and 9].
- Facial and intraoral photographs 3 years after retention.

- Three years’ postretention radiographs; lateral and posteroanterior cephalograms and panoramic radiographs.
A comparison of the change in tongue size is shown in [Figure 10].

- Comparison of the tongue size pretreatment (left) and posttreatment (right).
DISCUSSION
Our patient showed a severe Class III skeletal malocclusion associated with esthetic problems, mandibular asymmetry, masticatory dysfunction, lip incompetence at rest, and several secondary caries lesions. SSRO has become one of the most common methods for treatment of mandibular prognathism. However, SSRO alone is not indicated in cases of severe mandibular prognathism requiring more than 15 mm of posterior mandibular repositioning because the areas of bony contact would be very small as the mandible is rotated and moved backward to produce the desired occlusal relationships.[14] When mandibular setback in excess of 15–20 mm is expected, bimaxillary alternatives should be considered. A large mandible with a normal gonial angle may well take a 20 mm setback. However, 15 mm might be the maximum amount for mandibular setback in narrow rami and high angle deband 3 years after debonding on lateral cephalometric patients.[15]
On average, our patient presented with a sagittal discrepancy of 22.5 mm. Surgical procedures are not fully established in cases with severe anteroposterior discrepancy of more than 20 mm. Therefore, a combination of Le Fort I osteotomy with maxillary advancement, SSRO, mandibular body ostectomy, and partial tongue reduction was adopted due to the extremely severe anteroposterior discrepancies of 20 mm on the left and 25 mm on the right. Because of the complexity of the case, it was difficult to perfectly predict the amount of surgical movement, and this was one of the main reasons why a half- Class II on the right side was considered acceptable. An overcorrection ending in a Class II on the right side was contemplated due to the possibility of relapse that did not occur. The ostectomies involving the mandibular first molars were based on the diagnosis of secondary carious lesions affecting both mandibular first molars. After the surgical orthodontic treatment, the anteroposterior skeletal discrepancy was improved. The cephalometric changes included an increase in the ANB angle from –14.1° to +5.1° and Wits from –36.5 mm to –11.2 mm.
Although several studies on airway changes following mandibular setback surgery have shown that the posterior movement of the mandible usually narrows the airway, bimaxillary surgery promotes less decrease on the upper airway than mandibular setback surgery alone for the correction of the skeletal Class III malocclusion.[16] In this case, the upper airway area was measured at baseline, at deband 3 years after debonding on lateral cephalometric radiographs. Although a 2D representation of a 3-dimensional (3D) structure causes severe limitations as distortion, differences in magnifications, superimposition of the bilateral craniofacial structures; there is a significant positive relationship between nasopharyngeal airway size on a headfilm and its true volumetric size from a CBCT scan.[17]
When 3 years post-retention measurements were compared to baseline, a slight increase (11.3%) in the upper pharyngeal space was observed. Meanwhile, a decrease of 29.8% and 26% was observed in the middle and lower pharyngeal space areas, respectively [Figure 11]. However, there was no specific complaints or signs that indicated any association of the slight reduction of pharyngeal space areas and obstructive sleep apnea. In addition, there was no change in the patient’s BMI between the first visit and before the surgeries. However, a slight increase in the BMI was observed at the time of retention (BMI = 18.2) and 3 years post-retention (BMI = 19.1). This correlated with the self- reported decrease in chewing time. Therefore, chewing function improved significantly following orthognatic surgeries.
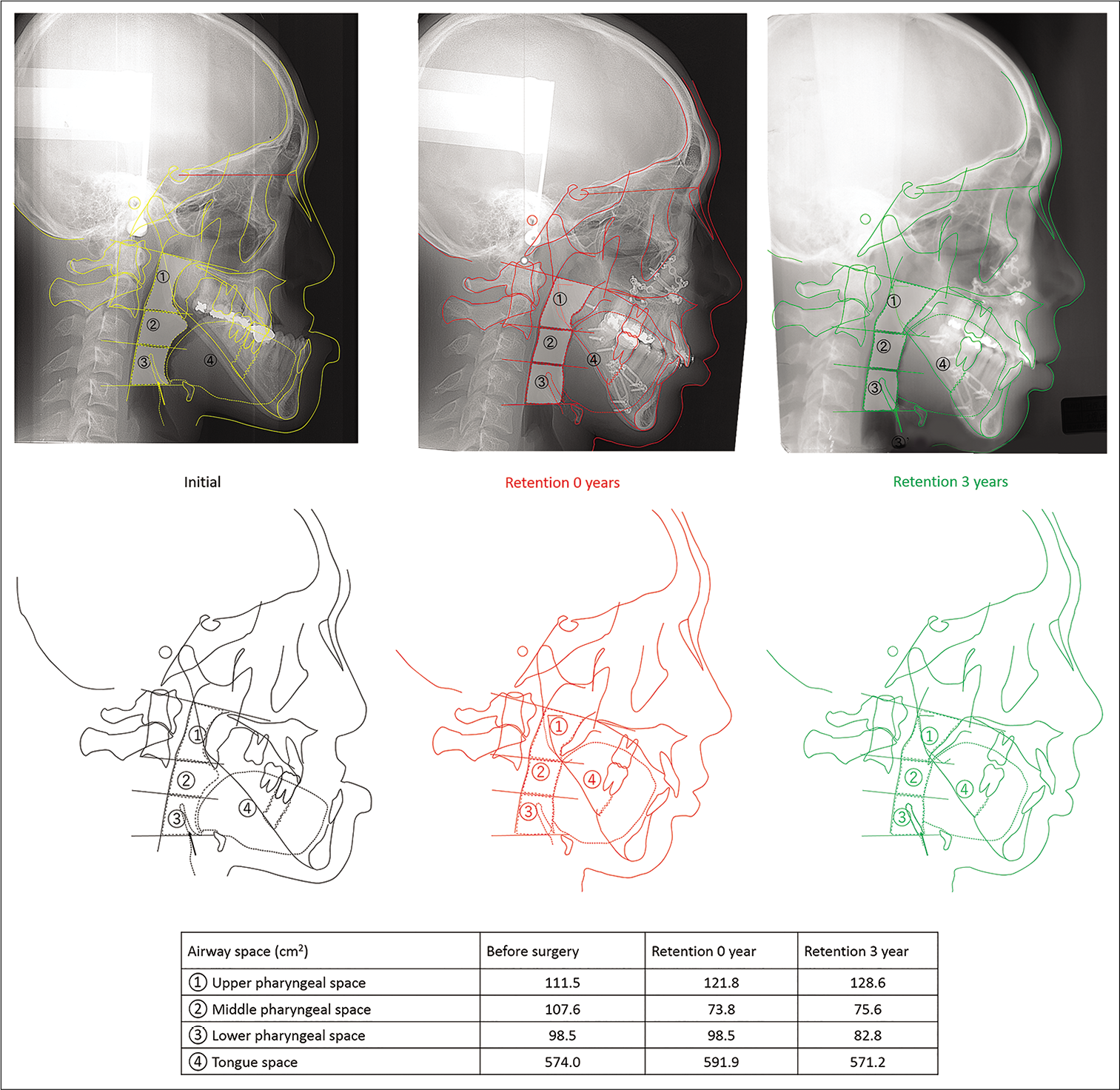
- Changes in the upper airway area. Initial (yellow), at deband (red) and 3 years post-retention (green). (1) Upper pharyngeal space the pharyngeal space between the lines of PNS to the apex dentis of axis and the lower faces of axis articulares to uvula. (2) Middle pharyngeal space; the pharyngeal space between the lines of the lower faces of axis articulares to uvula and the lower face of the third vertebrae cervicales. (3) Lower pharyngeal space between the lines of the lower face of the third vertebrae cervicales and the lower face of the fourth vertebrae cervicales to hyoid bone.
The partial tongue reduction aimed to decrease the tongue size because mandibular setback osteotomies produce positional changes of the tongue that can contribute to relapse.[18] Bimaxillary surgery resulted in good occlusal stability and the surgical reduction of the size of the tongue may have assisted in postoperative adaptation of the tongue and minimized relapse of the postsurgical mandibular position.
It can be argued that the final incisor position could have been improved with maxillary first premolar extractions. However, if the maxillary first premolars were extracted, this would have created more than 30 mm of maxillo-mandibular discrepancy that would have to be resolved with challenging orthognathic surgeries. Therefore, a compromised result with labially inclined upper incisors was considered appropriate in this case to reduce the risk of relapse and complications of orthognathic surgery. Due to the severity of skeletal discrepancies, the preparation of this case was challenging; individual variation response after bi-maxillary surgeries and the predictability of soft tissue changes is not a precise science.[19]
CONCLUSION
This case reports shows a Class III malocclusion patient with excessive anteroposterior skeletal discrepancy treated with Le Fort I maxillary advancement, sagittal split ramus osteotomies, mandibular body ostectomies, and tongue reduction surgery. Therefore, a combination of several surgeries may be required in the correction of extremely severe Class III skeletal discrepancies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There is no conflict of interest.
References
- Modern trends in Class III orthognathic treatment: A time series analysis. Angle Orthod. 2016;87:269-78.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in surgical-orthodontic management of Class III malocclusions in Western Australia. Australas Orthod J. 2020;36:62.
- [CrossRef] [Google Scholar]
- Factors contributing to relapse in rigidly fixed mandibular setbacks. J Oral Maxillofac Surg. 1989;47:451-6.
- [CrossRef] [Google Scholar]
- Evaluation of skeletal stability following surgical correction of mandibular prognathism. Br J Oral Maxillofac Surg. 2000;38:305-11.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular setback for surgical correction of mandibular hyperplasia-does it provoke sleep-related breathing disorders? Int J Oral Maxillofac Surg. 1996;25:333-8.
- [CrossRef] [Google Scholar]
- Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282-5.
- [CrossRef] [Google Scholar]
- Why most patients do not exhibit obstructive sleep apnea after mandibular setback surgery? Maxillofac Plast Reconstr Surg. 2020;42:7.
- [CrossRef] [PubMed] [Google Scholar]
- A Colour Atlas and Textbook of Orthognathic Surgery: The Surgery of Facial Skeletal Deformity London: Wolfe Medical; 1985.
- [Google Scholar]
- Treatment of severe mandibular prognathism in combination with maxillary hypoplasia: Case report. J Craniomaxillofac Surg. 2002;30:226-9.
- [CrossRef] [PubMed] [Google Scholar]
- Severe skeletal Class III malocclusion treated with 2-stage orthognathic surgery with a mandibular step osteotomy. Am J Orthod Dentofacial Orthop. 2014;145:S125-35.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996;110:170-7.
- [CrossRef] [Google Scholar]
- Valid consent and orthodontic treatment. Australas Orthod J. 2021;35:35-45.
- [CrossRef] [Google Scholar]
- A new method of tongue reduction for macroglossia. J Oral Maxillofac Surg. 1995;53:91-2.
- [CrossRef] [Google Scholar]
- Obwegeser II method for correction of mandibular prognathism. J Maxillofac Surg. 1980;8:288-93.
- [CrossRef] [Google Scholar]
- Corrective surgery of the mandible, ramus osteotomies In: A Colour Atlas and Textbook of Orthognathic Surgery Weert. London, United Kingdom: Wolfe Medical Publications; 1985. p. :171-89.
- [Google Scholar]
- Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal Class III malocclusion: A systematic review and meta-analysis. Int J Surg. 2017;38:31-40.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:468-79.
- [CrossRef] [PubMed] [Google Scholar]
- Partial glossectomy to stabilize occlusion following surgical correction of prognathism: Report of a case. Oral Surg Oral Med Oral Pathol. 1969;27:707-15.
- [CrossRef] [Google Scholar]
- Morphologic and functional implications of the surgical-orthodontic management of mandibular prognathism: A comprehensive review. Am J Orthod Dentofacial Orthop. 1993;103:439-47.
- [CrossRef] [Google Scholar]






