Translate this page into:
Cervicomental angle changes observed after mandibular advancement surgery – A systematic review

*Corresponding author: Vini Rughwani, Department of Orthodontics and Dentofacial Orthopedics, Dr. D Y Patil Vidyapeeth, Pune, Maharashtra, India. vinirughwani@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rughwani V, Durkar S, Deshmukh S, Jethe S, Rahalkar J, Kharche A. Cervicomental angle changes observed after mandibular advancement surgery – A systematic review. APOS Trends Orthod 2021;11(2):156-60.
Abstract
Purpose:
In adults, correction of such a jaw base relation is done by bilateral sagittal split osteotomy and mandibular advancement which often causes change in the cervicomental angle that might not be within the acceptable and aesthetic range. The objective of this systematic review was to evaluate the changes observed in cervicomental angle after mandibular advancement surgery.
Data Sources:
Based on the available data, we conducted an electronic database PubMed search, based on the search of published data from 1994 to 2017, six strategies were designed using two keywords, and four articles were shortlisted for systematic review.
Study Eligibility Criteria:
Studies that provide information on cervicomental angle changes after mandibular advancement surgery, published from 1994 to 2017.
Results:
The search yielded 168 articles, of which four were included based on the selection criteria. These articles described that the cervicomental angle observed after mandibular advancement surgery falls between 95° and 125°.
Conclusion:
Cervicomental angle decreases as the mandible is advanced to correct the jaw base Class II relation to Class I. Acceptable range is found to be between 95° and 125°.
Implications:
An esthetic look is the desire of every patient that reports to the clinics for an orthodontic correction. Surgical correction is an integral part of the treatment. While advancing the mandible, change is observed in the cervicomental angle. Knowing the acceptable range of this angle will help the orthodontist and the oral surgeon to plan the advancement accordingly.
Keywords
Cervicomental angle
Skeletal Class II
Bilateral sagittal split osteotomy
Chin-throat anatomy
Mandibular advancement
INTRODUCTION
Skeletal Class II jaw base relation is one of the most common scenarios experienced in clinical orthodontic practice. Such a jaw base relation could be due to (a) retrognathic mandible, normal maxilla (b) normal mandible, prognathic maxilla, and (c) combination of both.
Such a skeletal relationship, if found in growing children, can be corrected by growth modulation, whereas such a relation in adults can be corrected only by orthognathic surgery.
Mandibular advancement is the most frequently performed procedure for correction of skeletal Class II jaw base relation in adults with retrognathic mandible. Forward movement of mandible in orthognathic correction of skeletal dysplasia produce changes in the chin and lips that have been found in the previous studies.[1]
Predicting soft-tissue changes in relation to surgical skeletal correction is important while deciding the treatment protocol. Several soft-tissue analyses[2-6] have been developed to accurately predict the treatment outcome, however, focused on the region between glabella and soft-tissue chin.[1]
The morphology of the neck and its changes with the submental region has a great effect on the aesthetics of the lower face, and the chin-throat angle (CTA) is an important determinant of facial profile attractiveness. A number of etiological factors may be involved in creating a poor aesthetic silhouette of the chin-throat region, which include the tonicity and laxity of the submental-cervical skin, the suprahyoid muscle support, excessive submental, supraplatysmal and subplatysmal fat deposits, the size of the submandibular glands, the spatial position of the hyoid bone, and the skeletal framework of the mandible and chin. Forward positioning of mandible and/or advancement osseous genioplasty tend to improve the chin-throat aesthetics.[7]
Many experimental linear and angular measurements have been used to judge cervical and facial esthetics and to evaluate the soft tissue response to surgical correction protocol.[8] Despite the fact that there are numerous clinical reports of patients opting for various surgical procedures to change the submental cervical contour,[9-12] the submental cervical area has had a little consideration in radiographic analysis.
Each facial factor, such as the submental-cervical angle, has an “average” value or “norm” for a given population, which is age, gender, and racial specific. Each parameter has a range of normal variability, with the existence of a facial irregularity often subsequent to a significant deviation of one or more facial parameters from the accepted norm for that group of people. In clinical scenarios, it is important to determine at which point the deviation of a facial parameter moves from the acceptable range of variability to being perceived as a facial irregularity.[13]
The terms submandible-neck, chin-neck region, cervical angle, cervicomental, and submental area are all terms that mean the same and point toward the same anatomical area[1] that is formed by the cervical plane and the submental plane. The normal cervicomental angle ideally has been reported to be 90°.[14-16] Ellenbogen and Karlin[17] concluded that a cervicomental angle in the range of 105–120° is acceptable. Sommerville et al.[18] found that the ideal cervicomental angle to be 126° for men and 121° for women.
The objective of the study was to evaluate the changes observed in cervicomental angle after mandibular advancement surgery.
METHODS
Study design/sample
To address the research purpose, the investigators designed and implemented a systematic review. The study population was composed of publications concerned with the accuracy of virtually planned orthognathic surgery. Articles published until from 1994 to 2017 were considered. To be included in the study sample, publications had to fulfill the following criteria: The study is published in English and articles describe cervicomental angle and mandibular advancement. Articles were excluded as study subjects if they were case reports or series, protocol descriptions and no validation were performed of the used planning or assessment methods and articles that did not describe cervicomental angle or mandibular advancement. Quality assessment of the included study was carried out and investigators agreement regarding quality was tested.
Variables
The participants indicated for mandibular advancement surgery were considered. The main outcome was the changes observed in cervicomental angle.
Data collection methods
A primary PubMed search was performed using the following strategy so that the resulting study should contain one MeSH Term, one primary keyword, and one secondary keyword.
MeSH terms: Mandibular Advancement OR Lower Jaw Surgery AND Cervicomental Angle OR Chin Throat Anatomy.
Primary keywords: Mandibular Advancement OR Cervicomental Angle.
Secondary keywords: Bilateral Sagittal Split Osteotomy OR Mandibular Surgery OR Lower Jaw Surgery OR Lower Jaw Advancement OR Orthodontic Surgery.
Boolean operators were used to merge the search terms in the following manner: (Mandibular Advancement [MeSH Terms]) OR (Lower Jaw Surgery [MeSH Terms]) AND (Cervicomental Angle OR Chin Throat Anatomy).
The second step was to apply filters in PubMed, namely, the Language and Study design. Title screening of resulting studies was performed by one the observers to fetch only relevant studies. Found articles were retrieved in full text, their reference lists were examined for related studies.
Resulting relevant studies were subjected to abstract screening to see if they fulfilled the inclusion criteria or not, this screening was performed by two observers. If the abstract was not available or does not contain enough information, the full text of the article was retrieved and read for evaluation.
Data analysis
Initial data extraction was done by 1 author and then a secondary check for the accuracy of extracted data was performed and a consensus reached by two investigators.
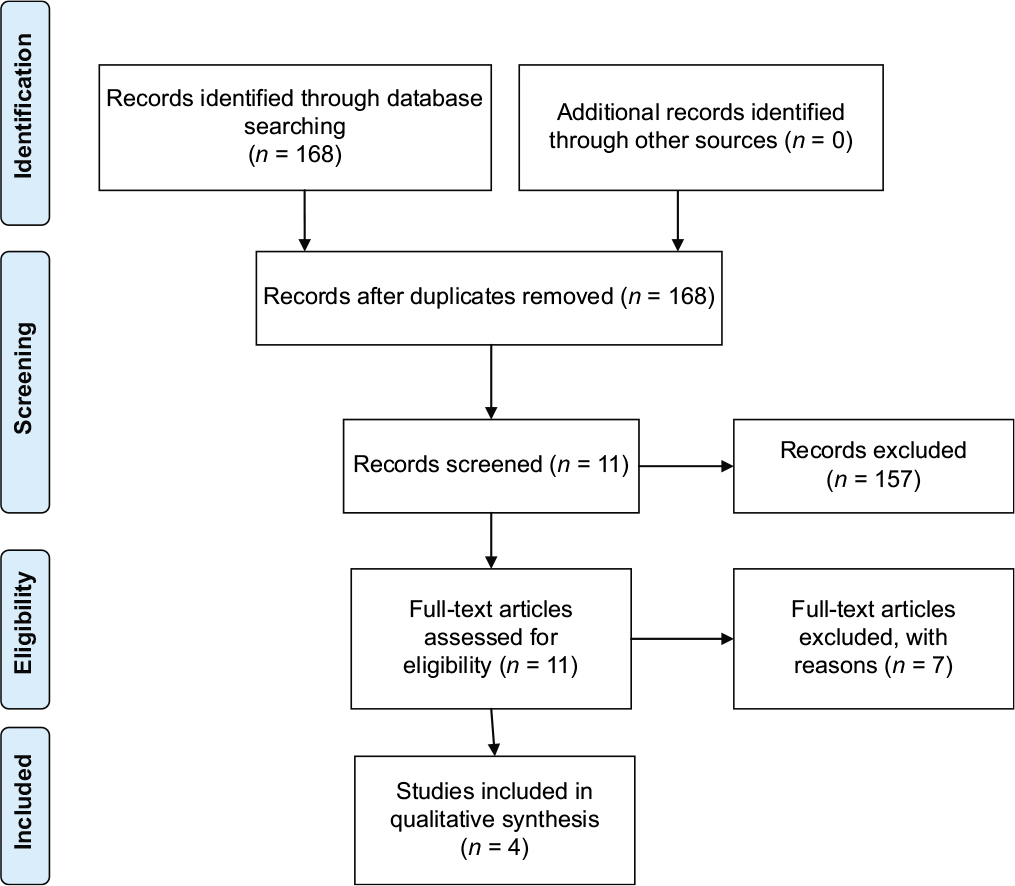
PRISMA 2009 Flow Diagram
RESULTS
Search results
The primary PubMed search revealed 168 studies after applying the language and study design filters. Title screening uncovered only 11 relevant articles as the other articles evaluating mandibular advancement did not evaluate cervicomental angle.
Full texts of the 11 studies were retrieved and four studies were finally included as the other studies did not quantify cervicomental angle.
DISCUSSION
In adult subjects having skeletal Class II malocclusions with mandibular deficiency, there traditionally are two possible treatment modalities. The first modality is camouflage orthodontics–extraction of upper premolars allowing retrusion of the upper anterior (ANT) teeth to normalize the overjet and cover the underlying skeletal problem. The second modality is orthognathic surgery to reposition the mandible anteriorly.[19]
In this systematic review, an exhaustive literature search attempted to find studies that evaluated the changes observed in the CTA after mandibular advancement surgery. In all studies, the method used to analyze the CTA was well stated and validated. No study declared blinding of measurement or analysis. Out of the four studies included, three were retrospective studies while one was a questionnaire analysis describing the facial attractiveness as rated by clinicians and laypeople [Table 1].
| Study id | Author and publication | Participants | Sample size | Intervention | Investigation | Results |
|---|---|---|---|---|---|---|
| 1 | Hayes et al., 1994[1] | Patients undergoing mandibular advancement | 24 | Mandibular advancement | Lateral cephalograms | On advancing the mandible, superior-anterior movement of hyoid bone is seen. With hyoid bone moving toward sella and posterior nasal spine, cervicomental angle becomes more acute leading to improvement in angle and reduction in convexity of profile. A decrease of 1.5° can be observed with 1 mm advancement of mandible |
| 2 | Mommaerts et al., 2004[20] | patients undergoing mandibular advancement | 40 | Bilateral sagittal spilt osteotomy | Lateral cephalograms | In cases treated with mandibular advancement with chin setback, the cervicomental angle remained acute. In mandibular advancement with posterior rotation, no change in cervicomental angle was observed and it remained more acute. In dentoalveolar mandibular osteotomy, the cervicomental angle showed improvement. In maxillomandibular posterior rotation, the cervicomental angle remained more acute |
| 3 | Naini et al., 2015[13] | patients undergoing mandibular advancement | 75 | Photographs | Mandibular advancement surgery is required except in cervicomental angle ranging between 110° and 120° | |
| 4 | Haddad and Ghafari, 2017[21] | patients undergoing mandibular advancement | 63 | Lateral cephalograms and photographs | The correlation between cervicomental angle and anterior were higher after surgery than before surgery |
Hayes et al. (1994)[1] quantified the changes seen in CTA and the lip-CTAs in response to forward positioning of mandible and hyoid bone positional changes. They concluded that on mandibular advancement, the hyoid bone moves toward sella, basion, and posterior (POST) nasal spine by 3.7 mm, with 1 mm of superior-ANT movement of hyoid bone, cervicomental angle reduced by 1.83°. As the hyoid bone moves 1 mm toward sella or posterior nasal spine, the cervicomental angle reduces by 2.13° and 1.94°, respectively. For each degree of reduction in lip-CTA, the cervicomental angle goes down by 0.77°. According to their findings, for each millimeter that the mandible is taken ahead, the cervicomental angle will go down by approximately 1.5°.
Mommearts et al. (2004)[20] performed a retrospective study of patients with deep bite hypoplastic mandible and evaluated the cervicomental angle, gonial angle, antegonial notch, lower lip position, and ANT mandible bowing after forward repositioning of mandible. They found that in groups with mandibular advancement/chin setback osteotomy and mandibular advancement-POST rotation, there was no significant change in the cervicomental angle in 30–40% participants but it became more acute in 50–60% participants, in dentoalveolar mandibular osteotomy group, there was slight improvement observed in cervicomental angle in 50% participants and no change observed in remaining 50% whereas, in maxillomandibular POST rotation group, cervicomental angle became more acute in all the participants post-surgery. They concluded that procedures that involve a setback of the chin along with mandibular advancement are potentially prone to create or increase submental fullness. It makes the cervicomental angle more obtuse making it difficult to manage, even with liposuction techniques.
Naini et al. (2015)[13] evaluated the influence of the submentalcervical angle on perceived attractiveness and threshold values of desire for surgery. They included 35 clinicians and 75 laypeople to guarantee 80% in the effectiveness of this questionnaire. This investigation showed that a submental cervical angle of 90–100° is considered to be the most attractive and up to 105° is considered acceptable. Angles above this value begin to be considered as unattractive, though up to 120° is deemed only little unattractive by the layman and clinician groups, but very unattractive by the patient group. By 125–130° all groups perceive the submental-cervical angle as very/extremely unattractive. In terms of threshold values of desire for surgery, for patients the threshold value of desire for surgery was 110°, for lay people the threshold value was 115° and similarly 120° for clinicians.
Haddad and Ghafari (2017)[21] determined if a new facial line (T), tangent to the throat, intersects the mandibular border in ANT and POST parts in proportions varying with facial configuration, and evaluated the association between chin projection and throat inclination and the potential for the T-line to reflect this association. They observed that patients with mandibular deficits are found to have a cervicomental angle of 90°. The Class II obtuse angle was less acceptable than either of the others, a conclusion agreeing with the other study done by the perception of a CTA angle of 110° as “slightly unattractive,” the “very,” and “extremely” unattractive set measured at 125° and 130°.[14] This finding supports the concept of more geometric delineation (expansion) of hard and soft tissues as being more esthetic than the constriction of skeletal volume.[18] A more obtuse CTA represents a constitutional limitation to ideal correction of the chin-throat zone in this dysmorphology, barring the surgical correction, whereby, on average, the post-treatment CTA (reduced by more than 15°) was closer to the Class I readings. In the younger sample, CTA decreased after treatment (from 127° to 115°), also closer the Class I values.[22]
CONCLUSION
Adult patients with deficient mandible require mandibular advancement for skeletal correction. Such patients often have an obtuse cervicomental angle giving an anesthetic and aged look. Mandibular advancement makes the cervicomental angle more acute, bringing it toward the normal range of 95–125°, which is perceived as attractive and gives a youthful neck appearance. Therefore, while evaluating soft tissues cephalometrically and planning mandibular advancement, the amount of correction required for the cervicomental angle should be taken into consideration.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The quantification of soft tissue cervicomental changes after mandibular advancement surgery. Am J Orthod Dentofacial Orthop. 1994;105:383-91.
- [CrossRef] [Google Scholar]
- Soft-tissue profile change associated with surgical correction of the prognathic mandible. Am J Orthod. 1974;65:483-502.
- [CrossRef] [Google Scholar]
- Soft tissue changes in relationship to movement of hard structures in orthognathic surgery: A preliminary report. J Oral Surg. 1974;32:891-6.
- [Google Scholar]
- Soft tissue profile change produced by reduction of mandibular prognathism. Angle Orthod. 1972;42:227-35.
- [Google Scholar]
- A cephalometric analysis of the long-term, soft tissue profile changes which accompany the advancement of the mandible by sagittal split ramus osteotomies. J Craniomaxillofac Surg. 1987;15:127-31.
- [CrossRef] [Google Scholar]
- The short-term and long-term soft-tissue profile changes accompanying mandibular advancement surgery. Am J Orthod. 1983;84:29-34.
- [CrossRef] [Google Scholar]
- Esthetic contour analysis of the submental cervical region: A study based on ideal subjects and surgical patients. J Oral Maxillofac Surg. 1994;52:704-13.
- [CrossRef] [Google Scholar]
- Submental liposuction extraction with hard chin augmentation. Arch Otolaryngol. 1984;110:454-7.
- [CrossRef] [PubMed] [Google Scholar]
- Suction lipectomy of the neck. Plast Reconstr Surg. 1985;76:882-9.
- [CrossRef] [PubMed] [Google Scholar]
- Suction assisted lipectomy of the face and neck. J Oral Maxillofac Surg. 1988;46:546-58.
- [CrossRef] [Google Scholar]
- Submentalcervical angle: Perceived attractiveness and threshold values of desire for surgery. J Maxillofac Oral Surg. 2016;15:469-77.
- [CrossRef] [PubMed] [Google Scholar]
- Plastic correction of double chin. Importance of the position of the hyoid bone. Plast Reconstr Surg. 1963;31:45-50.
- [CrossRef] [PubMed] [Google Scholar]
- The anatomical basis for common cosmetic anterior neck deformities. Ann Plast Surg. 1979;2:381-8.
- [CrossRef] [PubMed] [Google Scholar]
- Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg. 1980;66:826-37.
- [CrossRef] [PubMed] [Google Scholar]
- Morphology of the submental and neck region. Int J Adult Orthodon Orthognath Surg. 1988;3:97-106.
- [Google Scholar]
- Orthognathic surgery and dentofacial orthopedics in adult Class II Division 1 treatment: Mandibular sagittal split osteotomy versus Herbst appliance. Am J Orthod Dentofacial Orthop. 2004;126:140-52. quiz 254-5
- [CrossRef] [PubMed] [Google Scholar]
- Surgical options in deep-bite mandibular deficiency with prominent chin-aesthetic considerations. J Craniomaxillofac Surg. 2004;32:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- Chin-throat anatomy: Normal relations and changes following orthognathic surgery and growth modification. Angle Orthod. 2017;87:696-702.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular deficiency syndrome, III surgical advancement of the deficient mandible in growing children: Treatment results in twelve patients. Oral Surg Oral Med Oral Pathol. 1978;45:364-77.
- [CrossRef] [Google Scholar]






