Translate this page into:
Current status of clinical orthodontics in European and American countries

*Corresponding author: Kazuo Tanne, Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University Graduate School of Medical Sciences, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8553, Japan. tanne@hiroshima-u.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Tanne K. Current status of clinical orthodontics in European and American countries. APOS Trends Orthod 2020;10(4):204-23.
Abstract
Current status of clinical orthodontics in European and American countries was examined by means of a questionnaire survey through internet. In the European and American countries, most popular technique in daily orthodontic practice is preadjusted straight wire edgewise technique. In major developed countries in Europe and America, the treatment fee is considerably high, whereas the fee is relatively low in the countries under development and/or after economic crisis. Rate of non-extraction treatment among all the cases treated with multi-bracket appliances is significantly higher in Europe and America than in Asia except in a few countries. In the European and American countries, treatment system for jaw deformity patients is well developed with higher availability of the social health insurance than in Asia. The maximum CLP prevalence of 0.200 is found in Germany and Austria and the mean is around 0.140 or one to 700 births. In general, CLP treatment is covered by social health insurance in European and American countries. In Europe and America, lingual orthodontic technique has not become popular because patients never want to hide orthodontic appliance. Higher cost of lingual appliance and lack in information and technical skills may be the reasons of less frequent use of lingual appliance. Many interviewees replied that usage of TADs has not become so popular in USA and Canada as compared to that in Asia. In another word, the initial fascination with TADs wore off and are now used in selected patients as needed. This may be due to more harmonious maxillofacial structure with longer and wider dentitions in Caucasians which also results in higher rate of non-extraction treatment with multibracket appliances in European and American countries.
Keywords
Orthodontic treatment fee
Rate of non-extraction treatment
CLP prevalence
Lingual orthodontics
Temporary anchorage devices
INTRODUCTION
Orthodontic treatment has been distributed widely according to the development of technology in the field of mechanical engineering, material science, and informatics. It is thus anticipated to know how highly advanced orthodontic techniques and appliances are applied to daily orthodontic practice. However, the current status of clinical orthodontics in many countries is unclear and beyond our understanding. From these considerations, I have conducted an internet interview survey to elucidate the current status of dental and/or orthodontic professionals including the education in the Asian Pacific region and already published an article on this subject.[1]
In addition, the current status of dental and orthodontic education in Europe and America has already been examined and reported in an article,[2] demonstrating the following findings. The size of orthodontic society and the number of orthodontic department or dental school are smaller in Europe than in the USA. In Europe and South America, it takes 5–6 years to complete undergraduate dental education for dentist. Meanwhile, in Canada and the USA, dental school system has been developed, requiring 8-year education to become dentist. For orthodontic specialists, in general, it takes 3 years on average in European and American countries with an exception of 4-year training in Switzerland. Most societies in European and American countries have two important issues such as inappropriate orthodontic treatment and incorrect use of aligners by general practitioners. The most important strategy is to appeal the public that orthodontic treatment should be executed by orthodontic specialists. It is shown that the educational systems for dentist and orthodontist have well been developed in every country in the world, although the strength is somewhat different from country to country.
Thus, this article was designed to elucidate the current status of clinical orthodontics in the European and American countries and compare the outcome with that in the Asian Pacific region.[1]
MATERIALS AND METHODS
Internet interview
A questionnaire was sent to the following interviewees in the European and American countries and collected through internet [Figure 1].
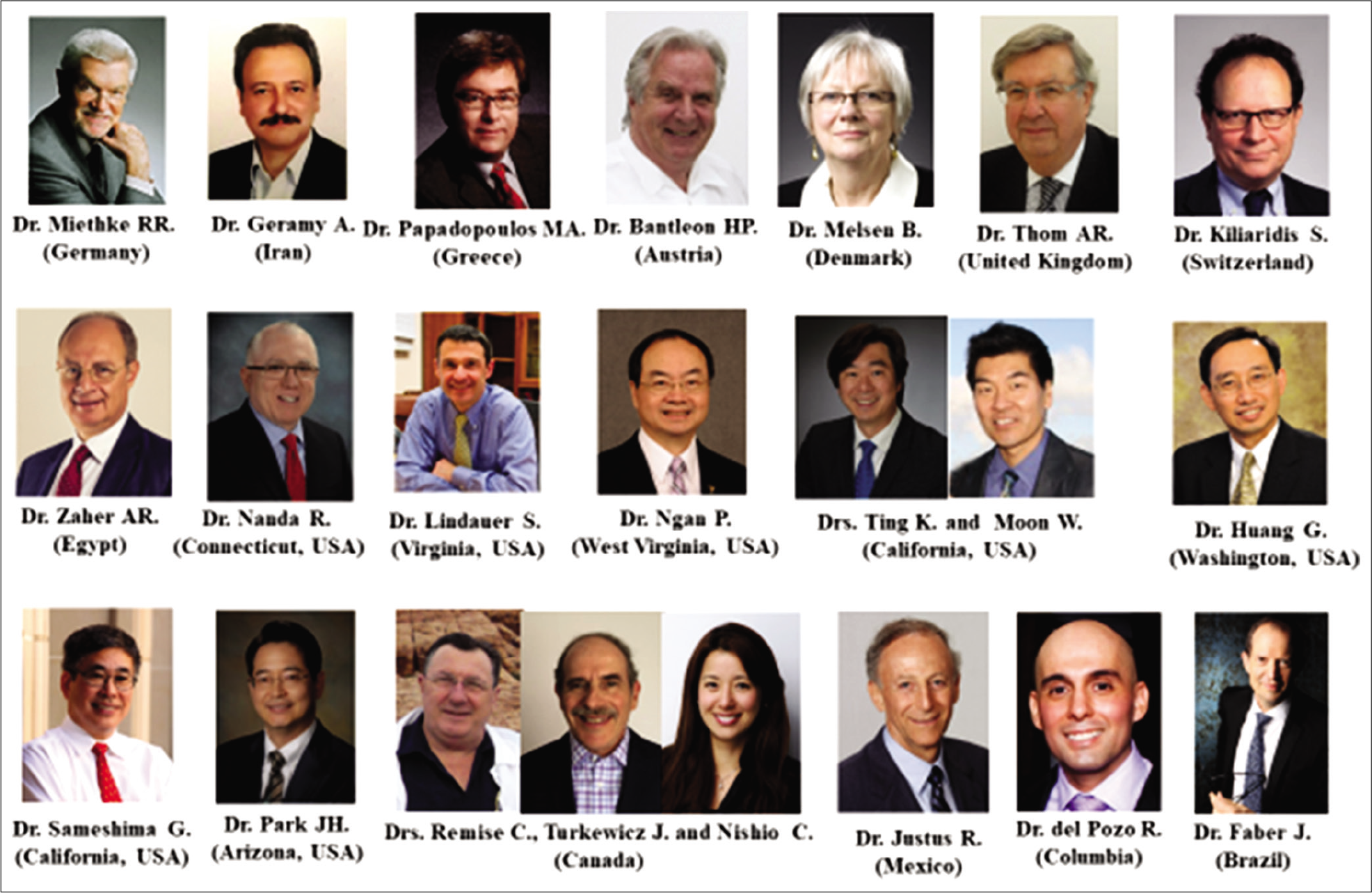
- A list of interviews in the European American countries.
Dr. Rainer-Reginald Miethke (Germany)
Dr. Allahyar Geramy (Iran)
Dr. Moschos A. Papadopoulos (Greece)
Dr. Hans-Peter Bantleon (Austria)
Dr. Birte Melsen (Denmark)
Dr. Allan R. Thom (United Kingdom)
Dr. Stavros Kiliaridis (Switzerland)
Dr. Abbas R. Zaher (Egypt)
Dr. Ravindra Nanda (Connecticut, USA)
Dr. Steven Lindauer (Virginia, USA)
Dr. Peter Ngan (West Virginia, USA)
Drs. Kang Ting and Won Moon (California, USA)
Dr. Greg Huang (Washington, USA)
Dr. Glenn Sameshima (California, USA)
Dr. Jae Hyun Park (Arizona, USA)
Drs. Claude Remise, Jack Turkewicz and Clarice Nishio (Canada)
Dr. Roberto Justus (Mexico)
Dr. Rodrigo Iván del Pozo Ayabaca (Columbia)
Dr. Jorge Faber (Brazil)
The interview was designed to ask about the following questions through the internet.
Therapeutic system or clinical technique successfully used for good treatment outcome and orthodontic treatment fee on average.
Percentage of non-extraction treatment cases among all the cases treated with multi-bracket appliances.
Treatment of jaw deformity patients and the social health insurance for the treatment.
Prevalence of cleft lip and palate (CLP) and the social health insurance for the treatment.
Current status and future development of orthodontic treatment with lingual appliances.
Current status and future development of orthodontic treatment with temporary anchorage devices (TADs).
Numerical data are summarized in tables. In addition, all the replied information and comments from each interviewee were shown in the text without any substantial modification.
RESULTS
1. Therapeutic system or clinical technique successfully used for good treatment outcome and orthodontic treatment fee on average
[Table 1] shows orthodontic treatment fee on average in each country or each state in the USA. In addition, the replies from each interviewee are presented for better understanding of readers.
| Germany | 3,000–3,500€ |
| Iran | 1,000–3,000 |
| Greece | 2,000–3,000€ |
| Austria | 5,000€ |
| Denmark | 4,500–7,500 |
| United Kingdom | 5,500–9,000 |
| Switzerland | 6,000–10,000 |
| Egypt | 1,200–2,500 |
| United States of America | |
| Univ. of Connecticut | 5,500–7,000 10,000 (Lingual appliance) |
| Virginia Commonwealth Univ. | 4,700–5,200 |
| West Virginia Univ. | 4,000 (Univ. Hospital); 5,500 (Private practice) |
| Univ. of California Los Angeles | 3,000–12,000 |
| Univ. of Washington | 5,000–8,000 |
| Univ. of Southern California | 4,000–6,000 |
| Arizona A.T. Still Univ. | 3,000–9,000 |
| Canada | 7,500–10,000 Canadian dollars |
| Mexico | 800–3,000 |
| Columbia | 400–2,500 |
| Brazil | 1,500–7,000 |
| Unit: US dolllars, if not specified. | |
Germany
Initially, I had a comprehensive training in all kinds of removable plates and functional appliances with Profs. Christian Schulze and Ullrich-Georg Tammoscheit. My training with fixed appliances at Louisiana State University was dominantly influenced by my late friend Dr. Jack Hickham’s directional edgewise orthodontics with extensive use of his variable headgear system. Later, this was complemented by the segmented arch technique of Drs. Burstone and Melsen. I also owe Dr. Rudolf Fränkel personally for an advanced training in functional regulators and Dr. Rudolf Slavicek for my introduction into Crozat appliances. In 2001, I became the first Invisalign provider in all Europe. With all the appliances/ systems, I have treated a good number of patients to their satisfaction. My main belief is to practice orthodontics which is not appliance – but indication driven.
The basic costs for a full fixed appliance treatment for patients under the compulsory public health insurance system vary between 3000 Euros and 3500 Euros, applicable to patients up to the age of 18 years. These costs are often complimented by some 600 Euros–1200 Euros for services/materials which are not covered by the state health insurance policy. The respective amount will be paid privately by the patients’ parents. The fees for privately insured patients with higher incomes are somewhat higher. The same is applied to publicly insured patients older than 18 years (see GOS at No. 7).
Iran
I have used both removable and fixed orthodontic techniques. Both active plates and functional ones are used in my private practice. My fixed orthodontic technique is standard edgewise and a few straight wire techniques such as Damon and Roth.
The treatment fee varies between 1000 and 3000 USD.
Greece
I received my training in orthodontics and my Doctorate Degree Thesis at the University of Freiburg in Germany during the late 80s. At that time, orthodontic training in Germany and most European countries was focused mainly on functional and removable appliances. I was happy to receive my training from my mentor Prof. Thomas Rakosi who was at that time a European expert on functional appliances and cephalometric radiography. Furthermore, Prof. Rakosi was one of the first European professors who invited colleagues such as Drs. Jarabak, Graber, Andrews, and Burstone from the USA to Europe, to share their knowledge on fixed appliances with the students and the German orthodontists. This way I got familiar to and gradually gained a lot of experience with the fixed appliances and the corresponding different techniques such as straight wire appliance and segmented arch techniques. During all the years when practicing orthodontics, I used all these methods with functional removable and fixed appliances and combined them together to achieve successful treatment outcomes for my patients.
The average fees for full orthodontic treatment with fixed appliances for an adolescent patient should be about 2000– 3000€. However, some years ago, before the financial crisis started in Greece, that is, before 2009, the average fees for orthodontic treatment were higher, ranging from 3000 to 5000€.
Austria
Precise treatment planning and integration of patients’ wishes are the keys of success.
The average fee for treatment with fixed orthodontic appliances in adults is 5000€, ceramic braces cause extra costs and lingual appliances are more expensive. Depending on the insurance, patients can request for a government grant. In the future, social insurance will cover the treatment fee for children at the age of 12–18 years, if they have a certain severity of malocclusion (IOTN 4 and 5).
Denmark
During the postgraduate education, functional and fixed appliances, continuous arches or segmented appliances, and labial or lingual are used according to the indication. Each of the postgraduate students starts orthodontic treatment of 50 patients, comprising children and adults. Among the latter, patients with need for surgery, degenerating dentitions, and periodontal and prosthodontic problems are assigned to each student.
About 25% of all children with the most severe problems get free treatment in the public clinics. The treatment fee with full fixed appliance for teenagers and adults in private clinics is approximately 4,500-7,500 US dollars.
United Kingdom
I have retired from clinical practice since obtaining my legal qualification. However, my subspecialty was treating cleft lip and palate and orthognathic treatment. I used straight wire and functional appliances for non-cleft growing individuals.
Fees for orthodontic treatment in private clinic vary enormously depending on location, ranging from 5,500 to 9,000 US dollars.
Switzerland
My education in Göteborg, Sweden, gave me (a) a thorough knowledge in interceptive orthodontics to identify and treat the suitable cases and (b) an extensive knowledge and experience in orthodontic treatment with fixed appliances. The evolution of recent methods in our field has influenced my clinical praxis. However, my adaptation to new orthodontic treatment approaches is based on evidence-based orthodontics. An important factor that influenced through these years my treatment results is a critical way of thinking and the serious criticism I always try to apply to my own treatment results.
The orthodontic fees in the region of Geneva vary from 6,000 to 10,000 US dollars, while in the German speaking part of Switzerland the fee may rise to 20% higher.
Egypt
Faculty members in the department are permitted to attend to private patients. This practice is adopted by the administration to compensate for the low salaries offered in the public universities. I see patients in my office 4 days/ week. My treatment philosophy is to use the simplest plan that can lead to the best outcome. For this, I have modified my appliance prescription several times until I reached a prescription suitable to my needs. I am now using a bidimensional system with an 018” slot on the upper central and lateral incisors to be able to control their torque earlier in treatment and an 022” slot for the rest of the teeth to decrease friction in sliding mechanics. I use a lot of sliding mechanics with elastic modules and Ni–Ti coil springs.
My regular treatment sequence is to first level and align teeth and then followed by reevaluation of the bracket positions for possible faulty ones. After complete alignment, I use stainless steel 0.016” × 0.022” as my working wire to manage spaces and then finishing. I use all auxiliaries as needed such as TADs, Class II and III tractions, especially the fixed ones. I do not recommend extraoral appliances to my patients, especially when certain benefits are added by TADs in use. All my functional treatment and growth modification are handled by pediatric specialists of my colleagues.
Orthodontic fees for cases treated with full fixed appliances are low in Egypt, ranging from US$1,200 to $2,500, depending on the clinician’s expertise and the location of the facilities.
United States of America
University of Connecticut
At the University of Connecticut, we have always followed that biomechanics and esthetic-based treatment are the key to providing optimal individualized treatment. We do not follow a “personality-based technique.” We are also active in using new and innovative ways to use TADs and “Surgery First” techniques. We do not believe in two-phase treatment unless a problem will have bad consequences on future growth or patient has a Class III malocclusion.
Orthodontic fee varies based on the regions of the country. In Connecticut, fee for orthodontic treatment ranges from US$5,500 to 7,000. For lingual orthodontics, it can be US$10,000.
Virginia Commonwealth University
Since I studied under Dr. Charles Burstone at the University of Connecticut, we were always taught to plan treatment based on the individual presentation of each unique patient. We were encouraged to develop individualized treatment goals and then to plan mechanics to achieve those goals. “We have the mechanics to achieve our goals” was the motto of the Department of Orthodontics at the University of Connecticut. I continue to follow those basic principles so I do not have “a cookbook approach to orthodontic treatment.”
However, of course, over the years and with experience, every practitioner discovers strategies that they find successful when treating certain types of cases. Here in the US, many of the patients who present for orthodontic treatment have Class II malocclusions with deep bite and excessive overjet. The orthodontic literature is filled with strategies designed to treat these types of patients.
In a patient with Class II malocclusion and deep bite, my favorite strategy continues to be the one that I learned as an orthodontic resident under Dr. Burstone. If the cause of the deep bite is due partly or mostly to overeruption of the maxillary incisors, it is easy to choose the following treatment plan:
First, I would place a transpalatal arch between the maxillary first molars and activate it to rotate the molars distally to fit more ideally with the mandibular first molars in a Class I position. At the same time, I would align the anterior teeth, either lateral incisor to lateral incisor[12-22] or canine to canine [13-23]. After the molars are fully rotated in about 3 months, I place a heavy anterior segment and then a Burstone’s intrusion arch from the molars and tied to the anterior segment. The intrusion arch causes intrusion of the anterior teeth (more if the 2–2 segment is present and less if the 3–3 segment is used) to correct the deep bite, while at the same time, the molars are tipped distally toward Class I occlusion. In many patients, it is the distal tipping of the molars early in treatment that is the most important ingredient for the success in achieving Class II correction. Hence, even if very little deep bite correction is needed, I will place an intrusion arch just to tip the molars distally but use a large anterior segment from canine to canine so I do not actually see any intrusion of the maxillary anterior teeth. If the patients are young and cooperative, I have them wear headgear to correct the root position of the molars so they are not excessively tipped distally.
With this method, once the molars are derotated and tipped back to Class I occlusion, the premolars also become Class I on their own. Otherwise, some light Class II elastics can be used later to move them distally. It may take several months to derotate the molars, correct the deep bite, and tip the molars back to Class I occlusion, but the patience usually is rewarded. Once these initial corrections have been made, the remainder of the teeth can be bonded and aligned. Then, the case is finished.
Fees for orthodontic treatment around Richmond, Virginia, are between US$5,500 and $6,500, which is a little bit lower than in the surrounding areas. Of course, the fee is different depending on the individual case difficulty and different practitioners might be more or less expensive. The fees at the school, Virginia Commonwealth University, are around 4,700-5,200 US dollars so they are just a little bit less.
West Virginia University
West Virginia University subscribes to Dr. Larry Andrews’ 6 Elements to Orofacial Harmony® in addition to the conventional straight wire appliance technique. The six elements treatment philosophy helps students to make clinical decision such as to how much skeletal and dental expansion is necessary and when is extraction indicated and which tooth to extract.[3]
The average orthodontic fee for comprehensive orthodontic treatment around the state of West Virginia is US$5,500. The fee for the orthodontic resident clinic in university is lower because of the teaching element and is around US$4,000.
University of California, Los Angeles
UCLA does not believe in the “cookbook” method of teaching. We believe in diversity of ideas and try to produce thinking orthodontists. We emphasize “evidence building” as much as, if not more than the “evidence-based” approach to learning orthodontics. We are progressive, yet value fundamental principles. We are at the forefront of microimplant orthodontics, digital technology, 3D analysis, soft-tissue quantifications, etc.
The treatment fees vary greatly in Los Angeles due to the diverse makeup of the city. The fee ranges from US$3,000 to $12,000. UCLA is located in one of the most affluent areas of the city, and the fees in the vicinity will be on the higher end.
University of Washington
I have found the clear aligner technique to be quite successful if the case selection is carefully considered. In my opinion, clear aligner treatment is going to become more and more popular, and eventually, I believe we will be printing aligners and other appliances directly from intraoral scans. The technological advancements we have seen over the past 15 years are only going to continue.
In Washington State, fees for comprehensive orthodontic treatment vary considerably. This is due to diverse economic conditions across the state. Perhaps, a range of fees might be from US$5,000 to $8,000.
University of Southern California
Treatment philosophy in both my practice and the USC program is straight wire with traditional treatment planning based on core values such as goal-oriented treatment. ABO standards are used throughout the diagnosis and treatment planning steps. Quality outcomes are assured through rigorous evaluation of case finishes based on ABO standards. The most popular appliance system in the private practices is the MBT system – Dr. Richard McLaughlin has been one of our faculty members for many years.
Fees in South California range from US$4,000 to $6,000 for teenager/young adult single-phase ordinary case.
Arizona A.T. Still University
Our residents learn a wide variety of techniques under the supervision of our devoted, full-time, and adjunct faculty members. Some of the techniques include Andrews, Alexander, Invisalign, lingual orthodontics, and temporary anchorage devices (TADs).
Treatment fees vary based on complexity, modality, and geographical region and may range from US$3,000 to $9,000 for comprehensive orthodontics.
Canada
During the orthodontic graduate program at the University of Montreal (UdeM), the residents are exposed to a variety of diagnostic techniques, such as Angle, Holdaway, Tweed-Merrifield, Ricketts, Burstone, and MBT. The types of fixed therapeutic appliance systems utilized include Damon, Speed, SmartClip, Empower, as well as Invisalign aligners and fixed and removable functional appliances.
However, our program is heavily weighted toward reviewing and mastering biomechanics theory and its practical clinical applications, to be able to provide efficient tooth movement and to minimize or eliminate negative side effects. Once the case is appropriately assessed and diagnosed and the treatment plan is established, the residents will generally produce successful treatment outcomes, especially when good patient compliance is obtained.
The orthodontic treatment fees vary to a large degree depending on the severity of the case, the projected length of treatment, the city, region, or province where the orthodontist practices. In the province of Quebec, the average fee for orthodontic treatment can vary between $7,500 and $10,000 Canadian dollars. Reduced fees are offered in university orthodontic clinics such as ours where full treatment cost is $4,400 Canadian dollars.
Mexico
I personally use the edgewise standard technique with Lewis brackets. The fee for orthodontic treatment varies greatly in Mexico from $800 to $3,000 US dollars.
Columbia
Since 2010, 50% of my clinical cases were treated with MBT philosophy. In 2013, I had the great opportunity with the sponsorship of 3M to study for 1 week in the city of Presidente Prudente in Brazil with world renowned Dr. Hugo Trevisi as one of the developers of the MBT philosophy. At present, 100% of my orthodontic treatments are done using this philosophy. I am also proud to mention that in all these years, I have treated patients with internal derangement using combined orthodontic mechanics with a pair of miniature splints developed by Dr. Kazuo Tanne and Dr. Eiji Tanaka in Japan.
In my office, the average fee is between US$ 1,000 and 2,000. In Colombia, the average fee is approximately US$ 400–2,500.
Brazil
“Surgery first (SF)” was independently developed by several contributors approximately at the same time. However, a Japanese orthodontist, Dr. Junji Sugawara, was largely responsible for spreading this therapeutic approach worldwide.
I have been using SF approach to treat dentofacial deformities since 2004. In my private practice, 75% of my SF patients require skeletal anchorage, mostly miniplates. The idea came to me when an obstructive sleep apnea syndrome (OSAS) patient was referred to my practice for orthognathic surgery. It was very clear at that time that we could not perform the conventional preparation for orthognathic surgery for patients with OSAS, but the patients would need to be operated immediately.
The literature provides many case reports and case series of Class III patients treated by SF. However, in my opinion, the patients who benefit most from the technique are the Class II patients. A significant proportion of these people have OSAS, no matter if they are Caucasians, Asians, or belong to other ethnic group. Patients with this disease must wear a CPAP during orthodontic preparation for surgery. An additional problem is that a minority of orthodontists addresses sleep-related issues during anamnesis, and an even smaller portion requests polysomnographies from those who have evidence of OSAS. I am very happy with SF treatment results for my Class II patients.
Brazil is a very large and diverse country. Just to exemplify that, the entire Europe – excluding Russia – would fit in Brazil, with enough room to accommodate a few other countries. Hence, there is a wide range in costs and local population income which reflects on orthodontic fees. The total treatment fee varies from US$1,500 to US$7,000.
2. Percentage of non-extraction treatment cases among all the cases treated with multi-bracket appliances.
[Table 2] shows the rate of non-extraction treatment with multi-bracket appliances. The comments from the interviewees are shown below.
| Germany | 90< |
| Iran | 40 |
| Greece | No specific numbers |
| Austria | 85–90 |
| Denmark | 70 |
| United Kingdom | 50 |
| Switzerland | 70–80 |
| Egypt | No specific numbers, but less than in Europe and America |
| United States of America | |
| Univ. of Connecticut | 80–85 |
| Virginia Commonwealth Univ. | 75 |
| West Virginia Univ. | 80 |
| Univ. of California Los Angeles | 70 |
| Univ. of Washington | 70–75 |
| Univ. of Southern California | 65 |
| Arizona A.T. Still Univ. | 70< |
| Canada | No specific numbers, but tends to increase |
| Mexico | 70 |
| Columbia | 60 |
| Brazil | 95< |
Germany
Since I am retired from my university, the Charité Berlin, I work as a part time in the office of one of my former residents. In his office, the extraction rate is probably between 5% and 7%. I guess that it is below 10% in Germany.
Iran
I think that there is a direct relation between insurance coverage for dental irregularities and extraction or non-extraction treatments. Patients come for treatment when the crowding is not tolerable for both the patient and the parents. In this situation, we can expect more extraction patients to be accepted in our clinics. In my private practice, the cases treated under extraction are about 60%.
Greece
The extraction/non-extraction debate has been a subject of controversy since the early days of modern orthodontics.
The balance between these two treatment philosophies has moved from one side to the other throughout the years. However, currently, it seems that the balance has shifted to the non-extraction side. This tendency is also valid for the Greek orthodontists. Unfortunately, specific numbers do not exist. Nevertheless, a comprehensive overview of all currently available approaches to correct Class II malocclusion with non-compliance approaches that decrease or even diminish the need to extract teeth is provided in my book entitled “Papadopoulos MA, editor. Orthodontic treatment for the Class II non-compliant patient: Current principles and techniques. Edinburgh: Elsevier, Mosby, 2006.” These non-compliance approaches enable the orthodontist to better control the outcome of orthodontic treatment and avoid extractions of teeth.
Austria
About 85–90% of the treatments among all treated cases with multi-bracket appliances in our clinic are non-extraction cases.
Denmark
I do not have the exact number, but I guess the number is diminishing following our publications of the detrimental effect of the expansion on the periodontium. A guess would be that 70% of treatments are performed under non-extraction. In my own private practice, a large number of patients are retreated from a non-extraction to extraction treatments due to periodontal problems.
United Kingdom
A recent MSc project at the Eastman Dental Hospital compared extraction versus non-extraction during the period 2005–2010 versus 1995–2000. There was no change noted with about 50%/50% each approach.
Switzerland
Switzerland has followed the pendulum that requested many extraction cases in the past to a substantial decrease in the number of extraction cases nowadays. The non-extraction treatment is the most common approach in approximately 70–80% of the cases. It is clear that there is a big variation in the treatment approaches used among the orthodontists based on their educational background and treatment philosophy.
Egypt
Although I do not have access to the percentage of extraction and non-extraction treatment in Egypt, I can sense that we have a higher percentage of extraction compared to that practiced in America and Europe. I can attribute this to the fact that the average incisors inclination for Egyptian population is slightly more protrusive than in other ethnic groups. The need for premolars extraction rises with the presence of some degree of crowding or lost space due to early loss of deciduous teeth combined with the desire to retract protruded teeth. In addition to these anatomical factors, the general preference among the Egyptian population is to obtain straighter profiles rather than convex or protrusive profiles.
All these reasons influence the clinician’s decision to be more inclined toward extraction treatment plans.
United States of America
University of Connecticut
Percentage of patients who undergo extraction has decreased considerably. In our department, extraction treatment is conducted in about 15–20% of patients.
Virginia Commonwealth University
I know that there are orthodontists in Virginia, and especially in the part of the state that is closest to Washington, DC or North Virginia, who boast that they “never extract teeth.” However, I would say that there is wide variation among practitioners all over the US and throughout Virginia. Because, as “Editor of The Angle Orthodontist,” I am invited to meetings and to lecture in different parts of the world. Thus, I know that in Asia (Japan, China, Taiwan, Korea, and Thailand), the frequency of extraction is much higher than in the US. According to an article by Proffit,[4] the extraction frequency at the University of North Carolina was 76% in 1968 and had decreased to about 28% in the early 1990s. Probably after that, the extraction frequency continued to decrease into the 2000s and has somewhat increased again from its lowest level.
I think that extraction decisions have to be based on individual patient circumstances and should not be determined by an orthodontist’s philosophy not to extract or to always extract. In contemporary practice in the US, these decisions involve patient input, esthetic preferences, as well as dental health concerns. While most of the current evidence does not suggest that periodontal damage occurs by flaring teeth when crowding is treated without extraction, I think that we do not have enough long-term follow-up on patients being treated during the current non-extraction era to know what happens to these teeth over time. Recently, I have had several patients who had been treated under non-extraction by outside orthodontists come to the school, saying that they were unhappy with the result because their teeth appear to be too flared out. This is something I did not see years ago. It is certainly more difficult to obtain good working occlusion with proper guidance when the anterior teeth are flared excessively.
Overall, I think even at the school we are willing to treat more crowded conditions without extractions than we were in the past. Our extraction frequency is probably close to 25%, although this is just the impression I have. I am sure that the rates vary in orthodontic offices around Virginia depending on the practitioners’ preference and the ethnic makeup of the patient population in different areas.
West Virginia University
The percentage of non-extraction treatment is around 80% with multi-bracket appliance in our clinic. This is probably in line with most of the clinics in North America.
University of California, Los Angeles
This percentage fluctuates significantly every year, but the latest was around 70%. I assume that this number will increase in the future due to implant-assisted orthodontics.
University of Washington
The extraction rate fluctuates, but my clinic director has informed me that 25–30% of our patients may be referred for extractions as part of their orthodontic treatment.
University of Southern California
We do not have a recent survey but I would estimate 35% as a rate of extraction treatment. Most of our patients are Hispanic or Asian with crowding and protrusion.
Arizona AT Still University
According to a 2017 AJO-DO article by Jackson et al.,[5] overall orthodontic extraction rates have been mildly decreasing to around 25% since 2006. I would say that more than 70% of the cases in our clinic use non-extraction treatment. I think that our clinic is not different from the state average for orthodontic treatment. However, extraction treatment is still advantageous for patients with significant crowding and protrusion.
Canada
The percentage of extraction cases has likely been reduced due to a variety of reasons, although we do not keep any specific data on this. Some factors, which have played a role in this reduction, are greater emphasis on maintaining adequate facial esthetics including soft-tissue profile and smile esthetics, pre-orthodontic periodontal procedures to increase gingival attachment, and parental hesitation in extracting healthy teeth.
In our graduate clinic, each treatment plan is individualized with respect to the patients’ specific problems, although it is probable that some variation in extraction frequency exists among the different clinicians to supervise the residents.
Mexico
In my clinic, about 70% of cases are treated non-extraction. I could not find any data in the rest of Mexico.
Columbia
I believe that in my clinic the non-extraction cases represent approximately 60% of my cases compared to 40% of extraction cases.
Brazil
We published a few years ago the first article to evaluate the esthetic impact of premolar extractions on the esthetics of the smile. We noticed how negative the extraction was, and we realized that the presence of the orthodontic appliance does not mitigate the negative esthetic impact of the extractions.[6] These results have made me migrate to treatment options without extractions whenever possible.
Very often, I apply miniplates for the retraction of the dental arches to avoid extractions. However, we recently demonstrated that hygiene is an important predictive factor of infection when miniplates are employed.[7] Thus, I use extractions primarily in adolescents since they have worse hygiene on average than adults. As my private practice is focused on adults, less than 5% of my patients are treated under extractions with the exception of third molars.
3. Treatment of jaw deformity patients and the social health insurance for the treatment
Germany
Adult jaw deformity patients in Germany are treated either by camouflage therapy, taking the profile, the periodontium, and the perioral functions into consideration or by combined orthodontic-orthognathic surgery.
Public health insurance will not pay for camouflage treatment of adults but for comprehensive treatment involving jaw surgery (see GOS at No. 3). Privately insured patients will be compensated depending on their policies.
Iran
Adult patients are treated just like young ones in different clinics. Unfortunately, there is not a complete pack of insurance to support orthodontic treatments.
Greece
Skeletal problems in adults are treated in Greece as everywhere in Europe or the USA. If the problem is mild, a dentoalveolar compensation is usually performed only with orthodontic treatment with fixed appliances and possible extractions of teeth. If the problem is mild to moderate, dentoalveolar compensation is performed, but temporary anchorage devices (TADs) such as miniscrew or miniplates may also be used along with fixed appliances with or without extractions of teeth in an effort to avoid surgery. Finally, if the problem is severe, the usual treatment plan includes orthodontic treatment with fixed appliances and orthognathic surgery to manage the skeletal discrepancy.
At present, the national health system in Greece does not cover any kind of orthodontic treatment, no matter if it is provided to young individuals or adults. Thus, patients or their guardians should pay the corresponding treatment fees privately.
Austria
Dentofacial asymmetries can pose a significant challenge to orthodontic treatment and an accurate diagnosis is key to localize the asymmetry and to determine the best treatment strategy. If the skeletal discrepancy is mild to moderate, the clinician will seek the patient’s opinion before deciding on a treatment plan of orthodontic camouflage treatment or of orthodontic treatment combined with orthognathic surgery. For patients whose orthodontic problems are so severe that neither growth modification nor camouflage treatment offers a solution, surgery to realign the jaws or to reposition the dentoalveolar segments is the only possibility. Surgery is not a substitute for orthodontics in these patients. Instead, it must be properly coordinated with orthodontics and other dental treatments to achieve good overall results. The correction of dentoskeletal malocclusions has always had a 3-fold goal of achieving functional efficiency, structural balance, and esthetics. In cases of severe malocclusion with dentoskeletal discrepancy, there are generally only three possible therapeutic options, that is, early modification of growth, orthodontic camouflage treatment through dental compensation, and combined orthodontic alignment and surgical repositioning of the jaw bases. In recent years, an increasing number of patients elect to undergo orthognathic treatment to correct severe malocclusion that is not susceptible to a comprehensive orthodontic solution. To treat complex cases like this, an interdisciplinary approach is essential.
The treatment fee is not completely covered, but there exists a financial support by the social health insurance.
Denmark
Patients with jaw deformities and/or need for surgery are treated for free and paid by social security. The treatments are performed in the dental schools, university hospitals, and partially in private clinics.
United Kingdom
Adult jaw deformity case is treated in hospital departments with joint input between orthodontists and maxillofacial surgeons. If the jaw deformity fulfills certain criteria of esthetic and/or functional requirements, it is usually state funded.
Switzerland
The adult patients seeking treatment for jaw deformities are treated with a combined approach of orthodontic treatment and orthognathic surgery. Most often, the problem is identified during childhood and adolescence, we can initiate a camouflage orthodontic intervention in mild cases according to the patient and parents wish. However, most of the moderate and all the severe jaw deformity cases are planned to be treated by a combined orthodontic and orthognathic surgical approach after the end of their puberty.
The state social insurance (Assurance Invalidité) covers the treatment expenses of these patients under the condition that they are characterized by certain dentofacial morphology and that they are not older than 20 years of age.
Egypt
Schoolchildren have access to free treatment in the students’ hospitals, however, this service is not reachable by all the children because of the lack of funding and shortage in the number of health providers. Orthodontic treatment is also offered for free for a certain number of patients in the various public universities depending on the teaching needs. In addition, some of the large organizations such as military hospitals offer free treatment to their employees and families. Other than that, orthodontic treatment is usually self-funded by the patients in private clinics and hospitals.
The Ministry of Health is also providing orthodontic services in its centers and hospitals, but the service is not well spread and limited only to a few facilities that include a specialist.
For adults with jaw deformities, orthognathic surgery is considered as an esthetic procedure but is not covered by the governmental health insurance.
United States of America
University of Connecticut
Treatment of choice for adult jaw deformity patients is always orthognathic surgery. Some slight to moderate problems are probably treated with camouflage orthodontics only if a patient does not qualify for insurance support or desires not to have surgery. Majority of these patients get insurance support if they exhibit medical problems such as sleep disorders, TMJ symptoms, and mastication issues.
Virginia Commonwealth University
Adult jaw deformity patients can be treated with orthodontic camouflage treatment alone or with a combination of orthodontic treatment and orthognathic surgery. The choice is often left up to the patient unless the magnitude of the deformity makes it impossible to obtain a reasonable result with orthodontic treatment alone. In most patients, however, correcting a true jaw deformity with some assistance from the oral and maxillofacial surgeons leads to a more satisfying result for the patient as well as the orthodontist.
From the range of case reports that appear in the orthodontic journals, I can tell that there are patients all over the world who refuse orthognathic surgery because they are afraid of surgery or because they feel the risks are too great. This occurs even in countries where jaw surgeries are covered under a national health insurance system. In those cases, there may be a suitable alternative plan with orthodontic treatment alone that will result in acceptable occlusion without making the facial esthetics worse. In some patients, however, such treatment may not be possible due to limitations in the amount of tooth movement that can be accomplished without compromising the health of the dentition. For those patients, there may still be a plan that improves the occlusion they currently have but that will most likely leave their occlusion short of ideal. Some orthodontists may refuse to treat patients to a non-ideal situation. Personally, I refused in the past to treat some patients because I felt that treating them without surgery would leave them worse than where they started or because doing so would prevent them from obtaining a better result later if they changed their mind and wanted to eventually pursue orthognathic surgery.
Recent developments in the use of temporary anchorage devices (TADs) have enabled orthodontists to treat some specific types of jaw deformity cases without orthognathic surgery. Specifically, patients with anterior open bites can be treated by intruding posterior teeth much more predictably than in the past because TADs make it possible to do this and get some autorotation of the mandible to correct the open bite. This is much more difficult or impossible if the open bite is associated with skeletal Class III malocclusion. In the literature, cases where the entire maxillary and mandibular dentitions have been moved distally have also been reported, so I guess nothing is impossible.
True skeletal jaw deformities cannot be corrected without jaw surgery in addition to orthodontics. In the US, jaw surgery was a very popular esthetic treatment, especially in the 1990s. Since then, insurance companies to provide health coverage in the US either stopped covering such procedures altogether or reduced the amount they will reimburse oral surgeons for performing these procedures. For some time in the early 2000s, it was extremely difficult to get jaw surgery to be covered at all. However, many companies will now approve some coverage if adequate justification for orthognathic surgery is provided.
Interestingly, in the US, it is the wealthy and the poor who are able to have jaw surgery. However, for middle-class people, it is usually more difficult because it is too expensive. Wealthier people may have better insurance plans which they have paid for or they get through their employer and cover these procedures. Insurance usually covers a percentage of the total cost of surgery, that is, even if 80% is covered, the patient may still have to pay $10,000 or more of the cost and this might be too expensive for many people. On the other hand, the poorest patients are covered by a national health plan that is administered by the individual states in the USA. In many states, including Virginia, jaw surgery will be covered 100% by this insurance up to the age of 19 years if the procedure is justified.
Sadly, long-term planning for a patient who needs orthognathic surgery is often difficult due to the insurance situation in the USA. It happened many times that we prepared the orthodontics by having teeth extracted to perform a certain surgical procedure, however, the insurance was changed and will no longer cover the cost of the surgery. For example, a patient with good insurance starts orthodontics and we intentionally make the occlusion worse to maximize the surgical skeletal change only to find out that the patient can no longer have the surgery. This may happen if the patient’s employer changes insurance coverage for the patient, or if the patient or parents of the patient change jobs and therefore change insurance companies. Even worse, if the parent of a poor adolescent with government coverage gets a better job, they may no longer qualify for government coverage and cannot have the surgery that was planned previously.
West Virginia University
At West Virginia University, the Department of Orthodontics works closely with the Department of Oral and Maxillofacial Surgery. We have orthognathic surgery seminar every Friday morning and go over cases that require surgical treatment for jaw deformity in combination with orthodontics. Surgery first is sometimes indicated for Class III jaw deformity, but most of the cases require a period of presurgical orthodontic treatment before surgical treatment.
Most of the patients undergoing orthognathic surgery have insurance to cover 80% of the cost for the surgical procedure and hospitalization. The state of West Virginia will approve Medicaid benefit for families with low income. However, the surgical procedure must be completed before the age of 21.
University of California, Los Angeles
Orthognathic surgical treatment is common at UCLA, in collaboration with oral surgery. Some are covered by private insurance, and many are covered by government insurance up to a certain age.
University of Washington
Significant skeletal deformities are usually covered by state assistance (Medicaid). CLP treatment and craniofacial care for children and adolescents are also covered.
University of Southern California
All craniofacial patients are seen at major centers (UCLA, USC, Loma Linda, etc.) in South California. Residents rotate through the centers. There is some government support for the patients.
Arizona A.T. Still University
Complex adult cases may be treated with or without orthognathic surgery. Surgery is considered a medical expense, and many times will not be covered by the patient’s insurance. Often, we can perform a non-surgical alternative treatment with minimal compromise.
Canada
In cases that require orthognathic surgery, the patient can choose to be treated either in the university clinic by orthodontic residents or by an orthodontist in private practice. Although the Canadian or provincial government do not cover the orthodontic treatment, some patients have private health insurance that covers part of the orthodontic treatment. While orthognathic surgery is generally covered by government health insurance, most oral and maxillofacial surgeons also charge supplementary fees that the patient is responsible for.
Mexico
Jaw deformity patients are treated with orthognathic surgery. The fee is not covered by any social health insurance and so the patients have to pay it.
Columbia
In my office, jaw deformity patients are treated with preand post-orthodontic mechanics and the social security system in Columbia (called EPS in Spanish) can cover the maxillofacial surgery; but as the social security system in many circumstances is slow and inefficient, many patients prefer to pay the surgery by their own means.
Brazil
Surgical-orthodontic treatment of dentofacial deformities in Brazil is primarily done in private practices. Some public hospitals do all the treatment at no cost to the patient, but a small number of people are reached by this benefit. In general, due to Brazilian laws and health insurance system, patient pays the surgeon’s and orthodontist’s fees. Health insurances cover hospital expenses.
4. Prevalence of cleft lip and palate (CLP) and the social health insurance for the treatment
Prevalence of CLP is listed in [Table 3]. Additional comments for the CLP treatment are shown below.
| Country | Prevalence of CLP (%) |
|---|---|
| Germany | 0.200 |
| Iran | 0.130 |
| Greece | 0.110 |
| Austria | 0.200 |
| Denmark | 0.140 |
| United Kingdom | 0.133 |
| Switzerland | 0.167 |
| Egypt | 0.143 |
| United States of America | 0.167-0.182 |
| Canada | About 0.140 |
| Mexico | 0.100–0.125 |
| Columbia | 0.070 |
| Brazil | 0.154 |
Germany
The rate of newborns with CLP in Germany is around 1:500. Their therapy is normally coordinated beside other specialists between the maxillofacial surgeons, the orthodontists, and speech therapists. An important procedure is late primary osteoplasty of the alveolus to facilitate eruption of the lateral incisors and/or canines.
The security system is quite generous because the fees for orthodontic treatment as well as for all surgical procedures of these individuals are almost fully covered by the insurance companies independent of the age when they are performed.
Iran
It is estimated to be 1.3 in 1000 live births. The cleft lip is 0.37, cleft palate is 0.32, and cleft lip and palate is 0.6 in 1000 of live births according to a published data in a national journal.
Greece
In Europe, according to a broad epidemiologic study that assessed almost 6 million births in 23 EUROCAT registries of cleft palate centers of 14 European countries, it was found that the prevalence of cleft lip and palate (CLP) among newborn babies was 1 per 907 births. These results may be also valid for Greece.
Patients with CLP receive in Greece their surgical- and medical-related treatments usually for free in the context of the national health system. However, for some treatments, patients have to pay a partial amount of the corresponding fees.
In the Department at the Aristotle University of Thessaloniki, during the past 15 years, we are very happy to function a special “Clinic of Craniofacial Anomalies” including CLP patients, which is coordinated by Dr. Ioannidou and myself. In this clinic, all children with CLP without any exception from the northern part of Greece receive not only orthodontic treatment for a minimum fee but also we coordinate their needs to receive dental and surgical treatment since we have a close cooperation with the other departments in the School of Dentistry, including oral and maxillofacial surgery, pediatric dentistry, conservative dentistry, and prosthetics. This way our “Clinic of Craniofacial Anomalies” functions like a CLP center for all patients in the North Greece.
Austria
The prevalence of CLP among newborn babies in our country is about 1:500. About 50% of these patients show a unilateral or bilateral CLP, 30% show an isolated cleft palate, and 20–25% show an isolated cleft lip/jaw. The treatment extends from birth to adulthood. Immediately after birth, infants get a drinking plate. At the age of 3–6 months, surgery is performed to close cleft lip. At the age of 18 months, surgery is performed to close the velum optionally with the insertion of a tympanostomy tube and the hard palate. The best moment for closure and bone grafting of the alveolar cleft is between 9 and 12 years, immediately before the eruption of the upper permanent canines. The orthodontic treatment consists of two stages; early treatment in the mixed dentition (for example, rapid palatal expansion or correction of anterior crossbites) and treatment with fixed orthodontic appliances in the permanent dentition. Most of the time further surgical procedures are necessary to gain better function and esthetics.
In general, there is a financial support by the government for patients with CLP, for orthognathic surgery as well as for orthodontic treatment. Successful treatment is only possible with an interdisciplinary approach.
Denmark
The prevalence is 1.4 per 1000 live birth. The treatment is organized in two centers, one in Copenhagen and one in Aarhus where the cleft team, composed of plastic and maxillofacial surgeons, specialists in orthodontics and prosthodontics, ENT doctors, speech therapists, psychologists, and special nurses, works together. The primary surgery is performed by the same team of plastic surgeons in Copenhagen for all Danish children. The treatment protocol is part of a larger European collaboration: “Eurocleft” and “Scancleft” studies. The treatment is fully supported by the government.
United Kingdom
Approximately 1 in 750 live births are cleft lip and/or palate. Such cases are treated from birth to maturity in designated cleft lip and palate centers by specialists. All treatments are state funded.
Switzerland
The incidence of the CLP babies born every year in Switzerland is 1 out of 600. There are five official centers of treatment in the University of Geneva in the French speaking part, and Universities of Basel, Bern, and Zurich in the German speaking part of the country as well as in the Medical School of the University of Lausanne. The primary surgery for lip and palatal closure varies between the different centers. However, an effort has done to implement the same treatment approaches in the Universities of Geneva and Bern. Meanwhile, the orthodontic interventions are almost similar to in all the five centers.
The state social insurance (Assurance Invalidité) covers all the treatment expenses of these patients up to the 20 years of age.
Egypt
The prevalence of CLP in Egypt is close to the world’s rates and reported to be one in every 700 live births. The treatment of those cases ought to be supported financially by the government in the Ministry of Health hospitals. However, because of the lack of necessary funding to many of those hospitals, these cases are often referred to specialized care units mainly in university hospitals but can still be financially supported by the Ministry of Health. The Department of Maxillofacial and Plastic Surgery in the Faculty of Dentistry, Alexandria University, is considered one of the first established tertiary care units to manage CLP cases. Our department of orthodontics was instrumental in the installation and development of the treatment protocol implemented in this center in 1987. We are continuously cooperating with the other specialties in the management of those cases. We hold together with the department of maxillofacial and plastic surgery, a clinical seminar every 2 weeks to plan the treatment and the follow-up for the cases. Then, the treatment is carried out in the various departments.
United States of America
Incidence of CLP in the US is approximately 1 out of 550–600 births. Treatment fee is almost universally covered by health and welfare agencies of all the 50 U.S. states governments.
Canada
A study published in 2015 assessed the birth prevalence, gender distribution, and pattern of surgical intervention for clefts in Canada. There were 3,015,325 live births in Canada from 1998 to 2007. The mean birth prevalence was 0.82 per 1000 live births for cleft lip with or without cleft palate and 0.58 per 1000 live births for cleft palate. The birth prevalence of cleft lip with or without cleft palate was significantly higher in boys, with a ratio of 1.75:1. While cleft palate was significantly greater in girls, the boy to girl ratio decreased from 0.97:1 in 1998 to 0.59:1 in 2007. The median age of repair in Canada from 1998 to 2007 was 4.7 months for cleft lip and 11.6 months for cleft palate. About 30% of patients underwent cleft palate repair after age 1.[8]
All provinces and territories of Canada have specific programs generally centered in hospital institutions that financially support dental services for the treatment of cleft lip and palate. Although most jurisdictions recognize that some dental coverage is necessary, there is a great variation in the manner in which provinces implement programs, allocate funding for dental services, determine the cutoff age, and decide which treatment services are covered.[9]
Mexico
CLP incidence is 1 in 800–1000 per live births. There are many government hospitals in Mexico that provide free treatment for CLP.
Columbia
The information is very limited due to the fact that only one big national study has been conducted. “It is observed that the prevalence of CLP is 0.07% in the country, while the report of these events is given in smaller proportion if reference is made to cleft lip or palate separately (ENSAB IV, 2016).”
https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENSAB-IV-Situacion-BucalActual.pdf -ENSAB: Estudio Nacional de Salud Bucal.
Brazil
The prevalence of CLP in Brazil is 1:650 birth. The data are from the government web page: http://www.saude.gov.br/atencao-especializada-e-hospitalar/especialidades/cirurgiaplastica-reparadora/fissura-labiopalatal
5. Current status and future development of orthodontic treatment with lingual appliances.
Germany
Since the number of adult patients is increasing, the figure of patients with lingual appliances is also rising. This trend is especially enhanced by modern or individualized bracket systems as Incognito and Win which make handling for the practitioner much easier than before. In addition, because of their small and refined bracket profiles, these appliances became much more acceptable and comfortable for the affected patients, too. On the other side, because of the substantially high costs, the circle of potential patients is limited.
Iran
I think that the lingual technique is not used widely or rare in Iran.
Greece
Adult patients occupy approximately 30% of all patients treated in the orthodontic offices in Greece. Before the economic crisis started in 2009, many adult patients were seeking for orthodontic treatment, and most of them decided to receive treatment with lingual appliances or clear aligners. However, these patients are currently significantly decreased since treatment with these modalities is associated with increased laboratory costs, which significantly increases the fees of orthodontic treatment. Thus, currently most of adults decide, for economic reasons, to receive treatments with other esthetic alternative modalities such as conventional fixed appliances with ceramic or clear brackets. Nevertheless, this will be probably reversed when the financial crisis will be over.
Austria
Lingual appliances were initially merely considered for esthetic reasons and because of the extra costs involved, they are mostly used in the adult patient population. The braces of lingual orthodontic appliances have become more discreet and so comfort has become higher. From the perspective of reducing frequencies of enamel decalcification, the lingual bracket approach seems favorable. Reasons, therefore, may be seen in enhanced saliva wetting and self-cleansing of enamel surfaces. There has been a paradigm shift in orthodontics to the use of lingual fixed appliances as opposed to conventional labial fixed appliances in the treatment of malocclusion. The positioning of the braces has become more accurate and reproduceable. Lingual fixed appliances can produce comparable treatment outcomes as labial fixed appliances over similar treatment time periods and therefore are an alternative treatment modality for patients to consider. More people wish to have an invisible treatment. I think that the cosmetic orthodontics will become even more popular.
Denmark
A handful of private offices is offering lingual treatment and a few cases are treated at the university. The demand is slowly increasing.
United Kingdom
Lingual appliances are almost exclusively used for private adult patients, but not funded by NHS/State.
Switzerland
The use of lingual orthodontic appliances is the real esthetic solution during an orthodontic treatment. This treatment approach offers a substantial help to adult individuals where visible “braces” are not tolerated. However, the request of such a treatment is limited due to the expensive treatment fees, at least 50% higher than the labial appliances, and the limited promotion by the reluctant orthodontists who hesitate to undertake such a treatment, either due to lack of knowledge and experience or the doubt of the treatment results of their first cases during their learning curve. One more unfavorable factor for the lingual treatment is the ergonomics of the treatment position and the chair time requested for this treatment. The use of lingual appliances tends to undergo a small increase, especially among the younger colleagues, after the inclusion of this treatment method in the curriculum of the postgraduate education, as is the case in our university. The newly graduated orthodontists are more keen to implement lingual techniques than the senior colleagues. Nevertheless, the lingual appliances do not seem to conquer the market and replace the labial appliances in the near future.
Egypt
Relatively low price range for orthodontic treatment in Egypt limits the use of expensive treatment modalities such as lingual technique and aligners. Most of the practitioners who provide lingual treatment have received their training outside the country. The lingual technique is not incorporated in the orthodontic training for the graduate students. However, the Egyptian Orthodontic Society has organized several courses for the various lingual techniques to educate the practitioners, whereas there are no specialized laboratories to provide the setup of lingual appliances in Egypt. Hence, all cases have to be sent for the setup of lingual appliances to laboratories outside the country, especially in Europe. The laboratories fees are expensive as they are set according to the orthodontic fees that are applied in Europe and are too high for the Egyptian market fees.
Many patients refrain from accepting treatment with lingual appliances just because the large difference in fees compared to the labial appliances. I believe that, with the improvement of the economic status in Egypt, the patient’s esthetic demands will increase and they will be willing to pay a reasonably higher fee for lingual treatment. The Department of Orthodontics in Alexandria University has organized a short introductory course on lingual treatment for its residents and has set up a task force composed of junior faculty members in collaboration with colleagues from France and Morocco. This would be the first program in Egypt to include lingual orthodontic treatment in its curriculum.
United States of America
University of Connecticut
Lingual appliance in the US never became very popular and it lags in its usage compared to European and Asian rim countries. Most of the orthodontic offices do not offer at all.
Virginia Commonwealth University
When I was a resident in the 1980s, lingual appliances were becoming popular and I was eager to try them after I graduated. However, right about that same time, ceramic brackets became available and lingual appliances never really took off.
Now, in some parts of the world, especially Europe as far as I know, lingual appliances have become a bigger part of the orthodontic market. Certainly, in the US, there has been an effort by companies to make lingual appliances a bigger share of the market. The manufacturers offer customized appliances, indirect bonding protocols, and prefabricated wires to make the process easier for practitioners. Patients seek lingual appliances because of their esthetic advantages, being on the inside of the teeth where no one can see them. In addition, it has been claimed that they offer the benefit of keeping the buccal surfaces clean and more accessible for performing oral hygiene procedures. In other words, if the patient has poor oral hygiene during orthodontic treatment, white spot lesions will form on the lingual surfaces of teeth and not be an esthetic problem.
In Richmond, Virginia area, there are only a few orthodontists that offer lingual appliances as a treatment option for their patients. My guess is that the esthetic appliance of choice in our area is clear aligners. At VCU, we have a couple of our part-time faculty members who are treating a limited number of patients in their practices with lingual appliances. They have been able to help the residents in our program treat some patients as well. In general, there seems to be a lot of difficulty by the patients in getting used to having the brackets on the lingual at first. Patients need encouragement to get through this difficult period. Likewise, orthodontists also have to treat a sufficient number of patients so that they and their staff can become comfortable with the lingual treatment procedures which are very different from traditional braces.
West Virginia University
Lingual appliances are not used extensively in our clinic or the state of West Virginia due to low demand in esthetic treatment. The use of lingual appliance is limited to the anterior teeth in conjunction with indirect bonding.
University of California, Los Angeles
The lingual appliance has not been very popular in the US when compared to that in other developed countries. However, we are teaching lingual techniques at UCLA because we have many international students.
University of Washington
We do not train our students in the lingual technique at this time, although they do receive some lectures on this topic.
University of Southern California
Residents have 2–3 cases treated with lingual appliances. They use a new appliance invented and patented by one of our faculty and scientists from the engineering school. There are no plans to expand the number of cases. Lingual is still not very popular in the USA.
Arizona A.T. Still University
We use lingual appliances in our clinic, but they are not very common. We have 1–2 patient/s/year who select this option. Most of our patients prefer Invisalign treatment.
Canada
Although some orthodontists offer treatment with lingual appliances, this appliance is not used so frequently in Canada. This evidence may be due to many factors, including the high cost of the treatment and the difficulty in the lingual orthodontic technique.
Mexico
Lingual appliances are being used in Mexico but I could not find data on percentage of use.
Columbia
As lingual orthodontic appliances or brackets in Colombia and in other South American countries continue to be very expensive, the usage is very limited.
Brazil
There is a growing demand for more esthetically pleasing orthodontic appliances by our population. This has boosted the use of lingual appliances in Brazil in the past decade. Neymar, Brazilian famous football player, underwent orthodontic treatment with lingual braces when he was a teenager in São Paulo. However, appliances with fully customized brackets are relatively expensive for a large part of our population. It is not very clear what are the future developments for lingual braces in Brazil and in the world. At present, they compete with aligners which have grown in quality and use.
6. Current status and future development of orthodontic treatment with temporary anchorage devices (TADs).
Germany
As in all orthodontically advanced countries, TADs are becoming more and more popular in Germany. However, only about 3% of all orthodontists insert miniscrews themselves. The majority of orthodontic specialists have these auxiliaries placed by oral surgeons.
I do not really like the term TAD because there are numerous adjuncts in orthodontics which serve temporarily as anchorage. A more appropriate term for these devices seems to be miniscrews because that is what they are.
Iran
TAD was introduced in our market a few years ago and spread among clinicians. It was considered to revolute our clinical judgments and treatment procedures. It was successful to show such ability in its appearance. Now, my colleagues and I continue to work without considering TAD as an inseparable step of our treatment plan. There are some others who believe in their abilities.
Greece
In addition to conventional orthodontic implants which have been used for anchorage purposes during the past decades, miniplates and miniscrew implants have been widely utilized as intraoral temporary anchorage devices (TADs) for the treatment of various orthodontic problems. All these modalities may provide temporary stationary anchorage to support orthodontic tooth movements in the desired direction without the need for patient compliance in anchorage preservation, reducing the occurrence of side effects as well as the total treatment time. A comprehensive overview of all currently available approaches to correct Class II malocclusion with these modalities is provided in my recently published book entitled “Papadopoulos MA, editor. Skeletal anchorage in orthodontic treatment of Class II malocclusion: Contemporary applications of orthodontic implants, miniscrew implants and miniplates. Edinburgh: Elsevier, Mosby, 2014.”
Despite the many advantages of TADs, however, similarly to other European countries, I do not think that they find a wide spread use in the everyday clinical practice of the orthodontists in my country. In addition, only a small portion of orthodontists inserts the miniscrew implants themselves, while the majority of orthodontists refer their patients to oral surgeons or periodontists to insert them on their behalf. Finally, the utilization of miniplates is even lower than that of the miniscrew implants among Greek orthodontists. Only a small minority of colleagues takes advantage of their use in their everyday clinical practice, while all of them refer their patients to oral and maxillofacial surgeons for the insertion and removal. The decreased use of miniplates may be related to the increased costs as well as to the invasive procedures needed both for the insertion and removal.
Austria
Due to perennial clinical experience and numerous investigations, TADs have become an indispensable component of modern orthodontic treatment.
Denmark
It is hard to say I would guess that 50% of orthodontists are using TADs, mostly the younger generation. At the postgraduate education, they all get some experience both in insertion and biomechanics.
United Kingdom
Headgear is rarely used. TADs have superseded, however, at present, TADs do not attract additional State/HS funding.
Switzerland
TADs provide opportunities to overcome treatment difficulties that were unsolved in the past. However, we have to admit that the vast majority of the malocclusions that demand an orthodontic treatment can be solved with conventional orthodontic means without the need to apply TADs.
Besides the huge contribution of the TADs to help us to solve previously unsolved problems, they can facilitate treatment procedures that demanded in the past certain complicated methods. However, the price we have to pay for these advantages is the “atrophy” of certain clinical skills that the orthodontists are not required to implement often. This is not a real problem until the time when the orthodontist will be forced to use a complex method in a case where the TADs cannot be used.
Thus, I consider that TADs will be a useful weapon in our treatment armamentarium, but I do not consider it as “the panacea” for all the orthodontic problems.
Egypt
The use of TADs is still not widespread in clinical orthodontic practice in Egypt. This is mainly for two reasons; there is an extra cost for the insertion of the miniscrews and a required additional training. The Egyptian Orthodontic Society has previously organized several training courses for the insertion of the miniscrews with various experts from around the world. This initial training was followed by advanced courses on the use and biomechanical principles of the treatment in conjunction with TADs. Yet, many clinicians are not incorporating TADs in their treatment protocols. However, most of the younger generations who are educated and trained to use TADs are using them extensively. Of course, the use of TADs is now embedded in the graduate training in the various programs that form the specialists. I believe, that in the near future, with continuous training and practice, more colleagues will be inclined to exploit the TADs assistance for their treatment.
United States of America
University of Connecticut
Usage of TADs is not as popular in the USA as you may find in Asian countries such as Japan and Korea. In my estimation, all orthodontic programs are currently teaching application of TADs. I feel that the younger generation of orthodontists will use more in the future. We, at University of Connecticut, are at the leading edge of innovative use of TADs in wide variety of patients.
Virginia Commonwealth University
TADs became commonly used, at least at VCU, in 2006. Before that, we had used some palatal implants but it was still quite ordinary to have the surgeons place the implant, wait for healing, send the attachments to be made in a laboratory, etc. When miniscrews first became available, we would refer patients to the oral surgeons to have them placed. For the patients, it was an added expense and it took time to go to the oral surgeon to have the miniscrew inserted as a separate procedure.
Around that same time, the VCU Department of Orthodontics sponsored a continuing education program for orthodontists in the Richmond area focused on TADs. We invited speakers from other parts of the US who were using TADs in their practices to come and lecture on how to place and use them. Many of the orthodontists in Virginia came to that meeting and I believe that marked the changing point from when TADs went from a rare addition to orthodontic treatment reserved for certain patients, to a more common adjunctive device for obtaining better treatment results almost routinely.
Following the initial surge in TAD use in the late 2000s, I think practitioners in Virginia realized that they did not need TADs in every patient to achieve excellent results. In other words, the initial fascination with TADs wore off and they are now used in selected patients as needed. Certainly, at VCU, we do not hesitate to place them when we feel the patient will benefit from having them but we do not use them if we can achieve the same results using conventional biomechanical principals. I think Dr. Burstone would agree. Some orthodontists still feel more comfortable having them placed by an oral surgeon or periodontist but, I think, most are placing them in their own offices themselves when patients need them.
West Virginia University
The use of TADs as anchorage device for orthodontic treatment is a routine procedure incorporated in the orthodontic treatment plan. Orthodontic residents take a cadaver course to learn how to place TADs and know the applications and limitations of using this tool to expand the scope of orthodontic or orthopedic treatment.
The greatest benefit of TADs is in the treatment of open bite malocclusions. Further, research will elucidate the long-term benefits of posterior molar intrusion and the best location to place TADs for mandibular intrusion.
TADs can be used in conjunction with clear aligners and lingual appliance to improve the comfort and esthetics of orthodontic treatment. Further, research is needed to demonstrate the proper use of these tools in comprehensive orthodontic treatment.
University of California, Los Angeles (UCLA)
UCLA has been the pioneer and trailblazer in this treatment modality. We perform arguably more implant orthodontics than any other institution in the USA. Orthopedic treatment protocols utilizing implants have been taught at UCLA since 2004. The West Coast tends to be more progressive than the rest of the country, and I assume that we do more implant orthodontics than elsewhere.
University of Washington
We do offer TADs to patients when we feel they are indicated. I think our usage at this time is relatively low, but certainly, TADs are more commonly used in our adult population. I believe that we have reached a fairly steady state with TAD usage.
University of Southern California
Residents start only 60 cases. The number of TAD cases is very limited and used only when traditional methods will not work, for example, isolated molar intrusion, molar upright, and anchorage loss. Most orthodontists in California do not use TADs very often.
Arizona A.T. Still University
We utilize a wide variety of TADs ranging from simple anchorage control to total arch distalization. Our residents graduate with the confidence and skills to use TADs in private practice.
Canada
The use of TADs in orthodontic treatment has been increasing and becoming more popular among Canadian orthodontists, although not as widespread as in Asia. However, further studies are necessary to develop more predictable stability and to increase the success of TADs during orthodontic treatment.
Mexico
TADs are being used in Mexico but I could not find data on percentage of use.
Columbia
In the Orthodontic Department of my University, we have good use of TADs (inter-radicular, infra-zygomatic, plates, and so on).
Brazil
TADs were adopted in Brazil very early. Miniplates and miniscrews were incorporated into the daily practice of clinicians around the country. Many articles have been published by Brazilian authors in international scientific journals about this topic. Our future challenge is shared with professionals around the globe: What kind of TAD is best and when?
DISCUSSION AND SUMMARY
According to a previous survey for the Asian Pacific countries, most popular technique frequently used in daily orthodontic practice was pre-adjusted straight wire technique.[1] Such result was similarly found in European and American countries, whereas removal and fixed functional appliances are still popular in Europe following the development of various functional appliances such as Activator, Bionator, and Frankel appliances.
In the Asian Pacific region, orthodontic treatment fee varies around 2,000 USD. The fee is extremely low or approximately 350 USD in India,[1] whereas considerably high treatment fee is found in New Zealand, Hong Kong, and Japan when orthodontic specialists are in charge of the treatment. The biggest challenge of IOS is the financial health of the contemporary Indian orthodontists. Meanwhile, in major developed countries in Europe and America, the treatment fee is considerably high, whereas the fee is relatively low in the countries under development and/or after economic crisis, that is, orthodontic fee is around 4,000-5,000 US dollars on average in Europe and America but substantially lower in Iran, Greece, Egypt, Mexico, and Columbia according to the political and economic status.
The rate of non-extraction treatment among all the cases treated with multi-bracket appliances was significantly higher in European and American countries than in Asian countries[1] except in Iran (40%), the United Kingdom (50%), and South California (65%) where people with Asian and Hispanic origins are living. Such higher rate of non-extraction treatment surely leads to easier orthodontic treatment and more frequent use of aligners in the European and American countries. On the contrary, in Asian countries, patients exhibit more complicated problems in the maxillofacial and dentoalveolar structures, and hence, more complicated and comprehensive orthodontic treatment is required under extraction. In addition, aligner treatment tends to frequently result in failure due to higher rate of extraction treatment for patients with more complicated craniofacial and dentoalveolar structures when applied by general practitioner in particular. Such problem has already been noticed in various countries in the world as was reported in a previous article.[2]
In the European and American countries, treatment strategy for jaw deformity patients has well been developed and the treatment is covered with the social health insurance. In the Asian Pacific region, meanwhile, surgical orthodontic treatment with orthognathic surgery is used successfully for jaw deformity patients, whereas in developing countries, the treatment has just introduced and will become more popular in near future.[1] Social health insurance system is not available in most Asian countries.
The prevalence of CLP varies from 0.10 to 0.20% in Asian Pacific region.[1] In the countries excluding Japan, Macau, New Zealand, Sri Lanka, and Taiwan, treatment of CLP was not covered by social health insurance. Meanwhile, the maximum CLP prevalence of 0.200 is found in Germany and Austria, and the mean is around 0.140 or one to 700 births in Europe and America. It is noticed that CLP prevalence in Europe and America was almost similar to that in Asia. It is also noted, in general, that CLP treatment is covered by social health insurance in European and American countries but not in Asian countries.[1]
Lingual orthodontic technique is popular and well accepted by adult patients in Asian counties, but is still under development in the remaining countries due to lack in information and technical skills and the high cost.[1] It is very interesting to know another reason from Thai Association of Orthodontists that patients like to have braces on the labial surfaces of their teeth as fashion statement as well as to show social status and thus less people are for the lingual orthodontics. Meanwhile, in Europe and America, lingual orthodontic technique has not become so popular because patients never want to hide orthodontic appliance. In fact, in the postgraduate orthodontic program, lingual orthodontic technique has not been well instructed.
It is of a great interest in a scientific aspect to know a comment from Dr. Hans-Peter Bantleon “Reasons therefore may be seen in enhanced saliva wetting and self-cleansing of enamel surfaces. There has been a paradigm shift in orthodontics to the use of lingual fixed appliances as opposed to conventional labial fixed appliances in the treatment of malocclusion. The positioning of the braces has become more accurate and reproduceable. Lingual fixed appliances can produce comparable treatment outcomes as labial fixed appliances over similar treatment time periods and therefore are an alternative treatment modality for patients to consider.” Dr. Steven Lindauer also documented “It has been claimed that they offer the benefit of keeping the buccal surfaces clean and more accessible for performing oral hygiene procedures.” Thus, it is indicated that lingual appliances are more optimal for the maintenance of oral hygiene.
In a biomechanical aspect, application of intrusion and extrusion forces to the anterior teeth from lingual appliances is more optimal than that from conventional labial appliances. The reason is found in a biomechanical study with finite element analysis,[10] reporting that lingual appliance makes it available to apply intrusion and extrusion forces through the long axis of tooth without producing labiolingual tipping of tooth appeared by the loading of intrusion and extrusion forces from labial bracket systems.
Recent topic in orthodontics with a great concern is TADs or MIAs, which have been successfully used and contributed to optimal orthodontic treatment. Thus, TADs or MIAs have gained a greatest interest or concern in many Asian Pacific countries because, in these countries, skeletal and tooth-jaw discrepancies are more severe due to smaller depth of the maxillofacial and dentoalveolar structures than in Caucasians in Europe and America.
However, as pointed by several interviewees, it should be noted not to use TADs in cases without any need and indication or to limit the application to absolutely needed and scientifically indicated cases.[1] Dr. Steven Lindauer also reported “We don’t hesitate to place them when we feel the patient will benefit from having them but we don’t use them if we can achieve the same results using conventional biomechanical principals.”
In addition, it is shown that usage of TADs has not become so popular in the USA and Canada as is found in Asian countries such as Japan and Korea. This may be reconfirmed by such comment as “Following the initial surge in TAD use in the late 2000s, orthodontic practitioners realized that they didn’t need TADs in every patient to achieve excellent results, that is, the initial fascination with TADs wore off and they are now used in selected patients as needed.” This may be due to more harmonious maxillofacial structure with longer and wider dentitions in Caucasians which also results in higher rate of non-extraction treatment with multi-bracket appliances and more frequent and easier usage of aligners which has taken a place of esthetic lingual appliance. It is hopefully anticipated that aligner is well combined with bracket system to create more optimal outcome of orthodontic treatment in near future.
CONCLUSION
In the European and American countries, most popular technique is pre-adjusted straight wire edgewise technique.
In major developed countries in Europe and America, the treatment fee is considerably high, but low in the remaining countries under development and/or after economic crisis.
Rate of non-extraction treatment is significantly higher in Europe and America than in Asia.
In the European and American countries, treatment system for jaw deformity patients is well developed with higher availability of the social health insurance.
The maximum CLP prevalence of 0.200 is found in Germany and Austria and the mean is around 0.140 or one to 700 births. CLP treatment is covered by social health insurance in most European and American countries.
In Europe and America, lingual orthodontic technique has not become so popular.
TADs are less popular in the USA and Canada than in Asia.
Acknowledgment
I would like to express a sincere appreciation to all the interviewees for their kindest help and cooperation for the publication of this article.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Current status of orthodontic professionals in the Asian Pacific Region. APOS Trends Orthod. 2016;6:58-77.
- [CrossRef] [Google Scholar]
- Current status of dental and orthodontic education in European and American countries. APOS Trends Orthod. 2019;9:211-22.
- [CrossRef] [Google Scholar]
- Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthod. 1994;64:407-14.
- [Google Scholar]
- Extraction frequencies at a university orthodontic clinic in the 21st century: Demographic and diagnostic factors affecting the likelihood of extraction. Am J Orthod Dentofacial Orthop. 2017;151:456-62.
- [CrossRef] [PubMed] [Google Scholar]
- Esthetic effect of orthodontic appliances on a smiling face with and without a missing maxillary first premolar. Am J Orthod Dentofacial Orthop. 2009;135:S55-60.
- [CrossRef] [PubMed] [Google Scholar]
- Infection predictive factors with orthodontic anchorage miniplates. Semin Orthod. 2018;24:37-44.
- [CrossRef] [Google Scholar]
- The epidemiology of cleft lip and palate in Canada, 1998 to 2007. Cleft Palate Craniofac J. 2015;52:417-24.
- [CrossRef] [PubMed] [Google Scholar]
- An Environmental Scan of Cleft Lip and Palate Clinics and Dental Benefit Programs in Canada Canada: Health Canada, The Canadian Association of Public Health Dentistry; 2009.
- [Google Scholar]
- Biomechanical responses of tooth to orthodontic forces applied at the lingual bracket positions. J Osaka Univ Dent Sch. 1992;32:6-13.
- [Google Scholar]






