Translate this page into:
Early intervention of unerupted maxillary central incisor: A case series

*Corresponding author: Chong Jun Ai, Clinical Oral Health Sciences, IMU University, 126, Jalan Jalil Perkasa 19, Bukit Jalil, 57000 Kuala Lumpur, Federal Territory of Kuala Lumpur, Malaysia. chongjunai@imu.edu.my
-
Received: ,
Accepted: ,
How to cite this article: Jun Ai C, Eng Ching M. Early intervention of unerupted maxillary central incisor: A case series. APOS Trends Orthod. doi: 10.25259/APOS_142_2024
Abstract
Early intervention of an impacted maxillary central incisor is crucial to avoid space loss with tipping of the adjacent teeth and allows normal root development. This case series demonstrates the clinical considerations of a surgical-orthodontic approach in managing this eruption anomaly and its challenges. All three cases involved young patients aged 7–9 years with an impacted upper left central incisor and a positive history of dental trauma. An upper sectional fixed appliance was bonded to facilitate the closed eruption of the impacted central incisor. The treatment duration increases when more space is required for the impacted tooth. There was a marginal gingival discrepancy of all the treated central incisors with vertical relapse seen upon review, indicating the need for a careful surgical approach with good hygiene maintenance and a bonded retainer as retention. Early referral for the management of an impacted maxillary central incisor through a surgical-orthodontic approach is often successful, but treatment risks, duration, and retention regimen should be discussed with the parents for informed consent.
Keywords
Incisor
Impacted
Esthetics
Child
INTRODUCTION
An eruption anomaly of the upper central incisor is suspected in a child between 7 and 9 years, where the lower incisors had already erupted a year prior, and the contralateral incisor had erupted 6 months earlier.[1] Impacted upper central incisors are the third most common impaction (0.06–0.2%) after the upper canines (2%) and third molars (24%).[1] The main etiology of impacted central incisors is obstruction and trauma.[2] Dental trauma to the anterior region could displace the underlying central incisor’s tooth germ and disrupt its development, leading to root dilaceration or enamel hypoplasia.[3]
Early intervention of an unerupted maxillary central incisor can prevent midline shift, loss of space due to tipping of adjacent teeth, and possible deviation of the eruptive pathway of the ipsilateral canine.[4,5] In addition, timely intervention, which is before the closure of the apical foramen, can allow normal root development.[6] This is because it has been shown that an impacted central incisor has a shorter root length of 2.13–3.22 mm than the contralateral tooth.[6] Furthermore, an unerupted maxillary central incisor can compromise a child’s esthetic, phonation, and alveolar ridge formation.[2] This case series aims to illustrate the clinical considerations of early intervention of unerupted maxillary central incisors and their challenges.
CASE REPORTS
Case 1
An 8-year 6-month-old healthy Chinese boy with a history of falls presented with a concern of “a gap between his front teeth.” Extraorally, the patient presented with a Class I skeletal pattern, average vertical proportions, and an average smile line. Intraorally, he had an unerupted upper left central incisor and a 1.5 mm space deficiency in that region. There was a Class I molar relationship with coincident midlines, increased overjet, and average overbite with poor oral hygiene. A palpable bulge could be felt labially in the area of the unerupted tooth. The dental panoramic radiograph revealed a horizontally impacted upper left central incisor with an open apex at the level of the middle third of the adjacent incisor root, giving a good prognosis for orthodontic traction into the arch. The root length of the impacted central incisor was shorter than the erupted contralateral central incisor as measured in the cone beam computed tomography slices [Figure 1].
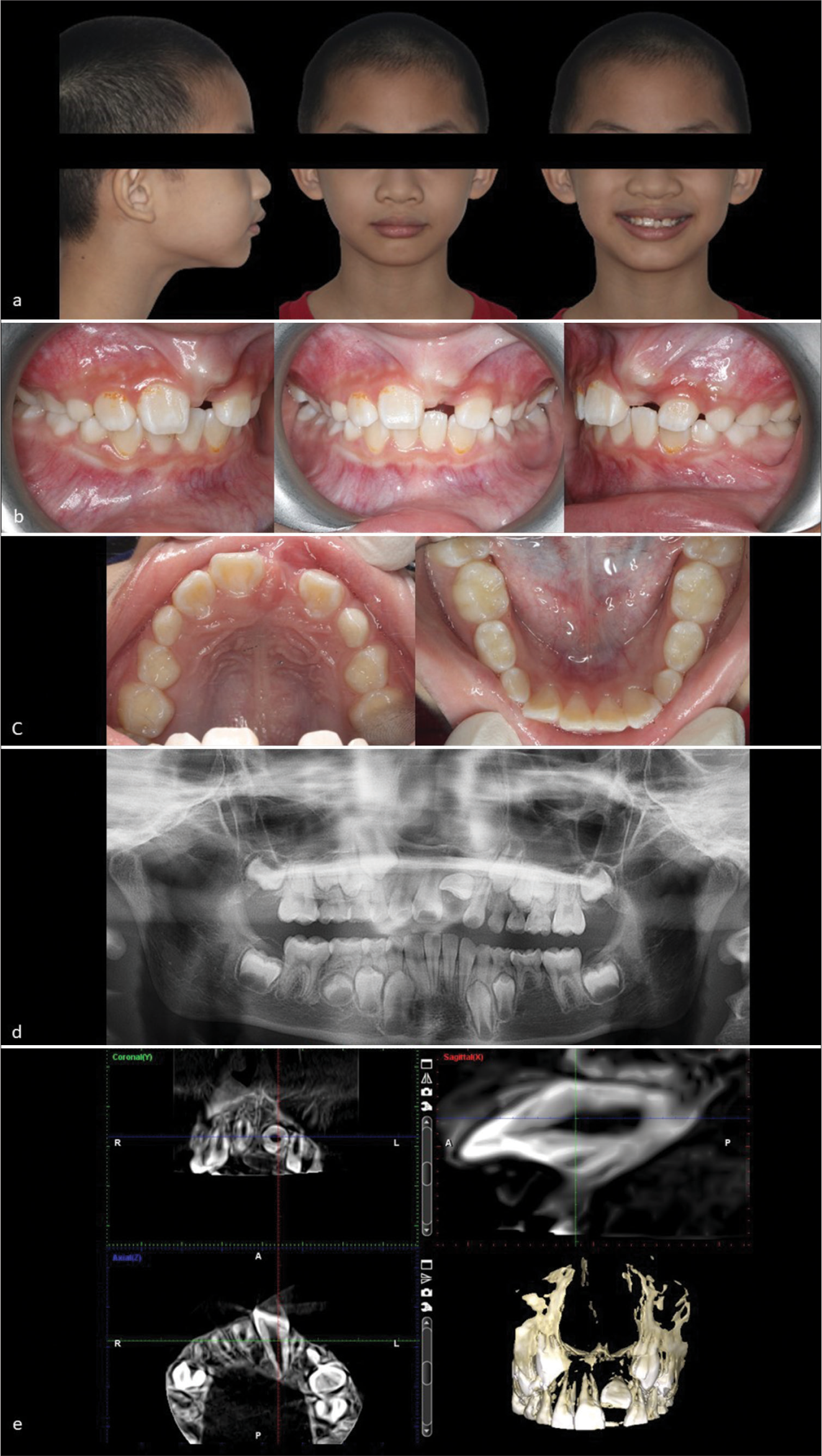
- 8-year 6-month-old boy who presented with an unerupted upper left central incisor. (a) Extraoral photographs (from left to right) showing a class I skeletal base with average vertical proportions at the profile view, competent lips at non-smiling frontal view, and unesthetic appearance with a clinically missing upper left central incisor at smiling frontal view. (b) Intraoral photographs (from left to right) showing right buccal, frontal, and left buccal intraoral view of a labial bulge at the unattached mucosa at the upper left central incisor region. (c) Intraoral photographs (from left to right) showing upper occlusal view depicting a mild space deficiency with an unerupted upper left central incisor and a lower occlusal view depicting mild crowding with mesiolingual rotation of the lower right lateral incisor. (d) The pre-operative dental panoramic radiograph reveals a horizontally impacted upper left central incisor, congenitally missing lower left second pre-molar and the adjacent upper incisors with open apices. (e) The pre-operative cone beam computed tomography slices illustrate a non-dilacerated impacted upper left central incisor with a short root.
Treatment objective and treatment options
A surgical-orthodontic approach to bring the upper left central incisor into the arch will provide complete alignment of natural teeth without a need for any prosthesis. Another treatment option was to surgically remove the impacted central incisor, followed by prosthetic rehabilitation. This alternative option will be a restorative burden for the child as the interim prosthesis will require frequent changes with growth until the patient is able to receive a dental implant. In addition, significant alveolar ridge resorption would have occurred from the early removal of the impacted tooth, compromising the esthetic outcome. Surgical repositioning of the impacted tooth could be another option, but it is technically demanding with the risk of ankylosis, loss of vitality, and root resorption.
Treatment progress
The parents consented to the orthodontic alignment of the impacted upper left central incisor. A closed surgical eruption technique was performed under local anesthesia whereby a flap was raised, and a modified chain made of a metal button and ligature wire was bonded onto the labial surface of the unerupted tooth. Then, the flap was sutured back into its former position, and the end of the chain was secured to the upper left lateral incisor [Figure 2a]. After 2 weeks postoperatively, conventional metal brackets with McLaughlin, Bennett, Trevisi (MBT) prescription 0.022 × 0.028-inch slot (Mini-Diamond series, Ormco Corp. Glendora, California, USA) were bonded on the upper arch, and a 0.014-inch nickel titanium archwire (NT3, American Orthodontics, Sheboygan, Wisconsin, USA) was used to align the arch. Space was gained before the alignment of the impacted tooth through proclination of the upper incisors with an open coil spring on a 0.018-inch stainless steel wire (American Orthodontics, Sheboygan, Wisconsin, USA) which acted as the base archwire. Then, a piggyback technique was used in which a 0.012-inch nickel titanium archwire (NT3, American Orthodontics, Sheboygan, Wisconsin, USA) was placed through the modified chain bonded onto the impacted tooth as a continuous force to bring the tooth occlusally. The nickel-titanium archwire was overlayed onto the base archwire to prevent deformation of the arch form. Once the tooth appeared through the oral cavity, the piggyback technique was continued with a 0.012-inch nickel-titanium wire secured with composite to the top of the metal button [Figure 2b]. Then, the left central incisor bracket was properly bonded, and a continuous 0.012-inch nickel titanium archwire was used to align the tooth. The archwire was gradually increased to 0.018-inch stainless steel. Finally, a four-link power chain was used to gather the incisors together before debond [Figure 2c]. The near-end dental panoramic radiograph revealed successful alignment of the upper left central incisor with a similar root length as the contralateral incisor [Figure 2d].

- 8-year 6-month-old boy who presented with an unerupted upper left central incisor. (a) Frontal photographs showing initial and final outcome of the closed surgical exposure with bonding of a modified chain attachment. (b) Mid-treatment intraoral photographs showing piggy-back mechanics of which a light 0.012-inch nickel titanium wire was attached onto the highly placed upper left central incisor over a 0.018- inch stainless steel base archwire. (c) Near-end intraoral photographs showing consolidation of the upper incisors with a power chain on a 0.018-inch stainless steel archwire. (d) Near-end treatment dental panoramic radiograph reveals successful alignment of the upper left central incisor with similar root length as the contralateral incisor. (e) Upper left central incisor in alignment with the adjacent central incisor but mild gingival discrepancy is seen at debond. (f) Vertical relapse of the upper left central incisor is seen at 6-month review. (g-i) Extraoral smiling photographs (from left to right) showing the pre-treatment, debond, and 6-month review, respectively.
Treatment results
The upper fixed appliance was debonded after 7 months of treatment [Figure 2e]. A fixed retainer was not placed due to the patient’s poor oral hygiene. Consequently, there was a vertical relapse of the upper left central incisor upon 6-month review [Figure 2f]. However, the parents were still satisfied with the outcome as compared to preoperatively [Figure 2g-i].
Case 2
A 9-year 2-month-old medically fit Chinese boy presented with a concern of an unerupted front tooth. He had a history of falls leading to a disto-incisal fracture of the upper right central incisor a year ago. Extraorally, he had a Class II skeletal base with average vertical proportions and a protrusive upper lip [Figure 3a]. Intraorally, he had an unerupted upper left central incisor, which was palpable at the labial sulcus, increased overjet and overbite, and space deficiency of 3.5 mm [Figure 3b]. The upper incisors were responsive to vitality testing with no tenderness on percussion. Radiographically, the impacted upper left central incisor was horizontally impacted, and the contralateral central incisor showed a closed apex with normal root length [Figure 3c and d].

- 9-year 2-month-old boy who presented with a positive trauma history and impacted upper left central incisor. (a) Extraoral photographs (from left to right) showing a Class II skeletal base with average vertical proportions at the profile view, incompetent lips at rest, and a guarded smile due to unerupted upper left central incisor. (b) Intraoral photographs showing a mesiopalatal rotated upper right central incisor with a distoincisal edge fracture, unerupted upper left central incisor with a labial bulge, space deficiency due to mesial tipping of the upper left lateral incisor, and arrested caries on the deciduous molars. (c) The periapical radiograph shows a horizontal impaction of the upper left central incisor and adequate space made for its alignment. (d) The dental panoramic radiograph reveals a horizontally impacted upper left central incisor toward the midline with no root resorption of the adjacent central incisor.
Treatment objective and treatment options
Various treatment options were offered, like Case 1, and the parents decided on closed surgical exposure with the bonding of an attachment on the impacted upper left central incisor for orthodontic alignment.
Treatment progress
Upper passive self-ligating pre-adjusted edgewise brackets with MBT prescription 0.022 × 0.028-inch slot (Damon Q™ System, Ormco Corp. Glendora, California, USA) were bonded, and a 0.013-inch copper-nickel-titanium archwire (Ormco Corp. Glendora, California, USA) was ligated. Subsequently, space was created for the upper left central incisor using a push coil on a 0.018-inch stainless steel archwire (American Orthodontics, Sheboygan, Wisconsin, USA) [Figure 4a]. Once adequate space was created, the patient was referred for closed surgical exposure and bonding of a gold chain (American Orthodontics, Sheboygan, Wisconsin, USA). The chain was activated via a piggyback technique using a 0.013-inch copper-nickel-titanium archwire with the 0.018-inch stainless steel wire as the base archwire. The number of chain links seen in the oral cavity was counted, noted, and removed sequentially at each visit, signifying active movement of the impacted incisor [Figure 4b]. This was continued until the tooth appeared in the oral cavity and was occlusal enough for a continuous 0.013-inch copper-nickel-titanium archwire to be ligated to a bracket on the labial surface of the left central incisor. The orthodontic traction of the impacted tooth took approximately 8 months.
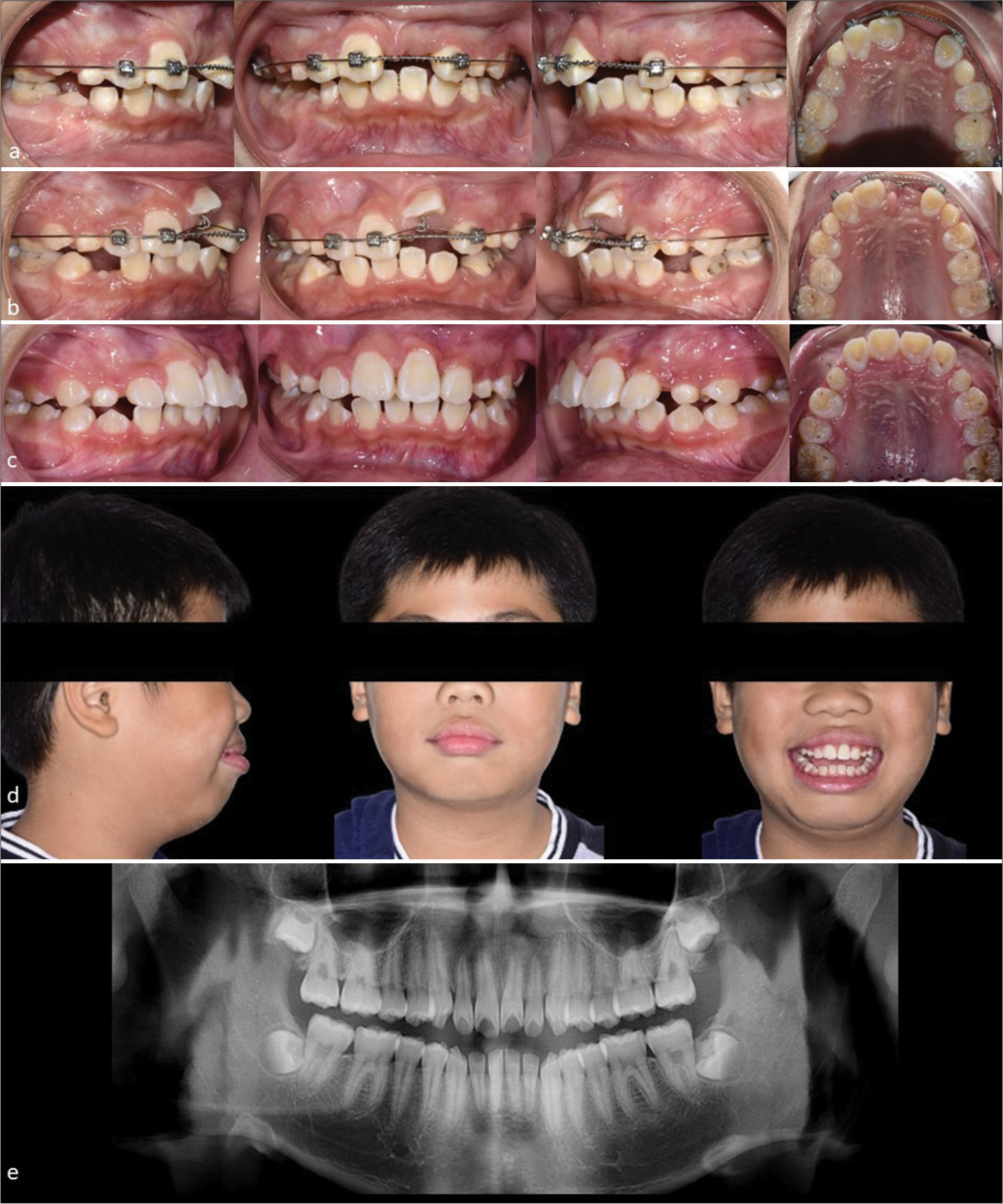
- 9-year 2-month-old boy who presented with a positive trauma history and impacted upper left central incisor. (a) Mid-treatment intraoral photographs showing adequate space creation of upper left central incisor with push coil on a 0.018-inch stainless steel archwire. (b) Intraoral photographs taken 11 months into treatment showing use of 0.013-inch copper-nickel-titanium wire through the gold chain of the upper left central incisor over a 0.018-inch stainless steel base archwire. (c) The upper left central incisor was successfully aligned into the arch with minimal gingival discrepancy as compared to the contralateral central incisor at debond. (d) Extraoral photographs showing protrusive soft tissues but a pleasant smile with the upper incisors aligned. (e) The dental panoramic radiograph after 3-year post-treatment reveals a minor vertical relapse of the upper left central incisor and a shorter root length compared to the adjacent central incisor.
Treatment results
The upper fixed appliance was debonded after 16 months of treatment. There was a slight marginal discrepancy between the gingiva contour of the central incisors, but the parents were pleased with the results as it was not too noticeable upon smiling [Figure 4c and d]. The post-operative dental panoramic radiograph taken 3 years, after debond, showed a vertical relapse of the upper left central incisor with a shorter root length compared to the upper right central incisor [Figure 4e].
Case 3
Parents of a 7-year 8-month-old healthy Chinese girl came with a concern about their daughter’s slow eruption of the upper left front tooth. She had a history of falls during childhood. The child had a Class I skeletal base with average vertical proportions [Figure 5a]. Intraorally, she presented with early mixed dentition, impacted upper left central incisor, and unerupted first permanent molars. There were carious and mobile upper deciduous lateral incisors and a large restoration on the lower left first deciduous molar with poor oral hygiene [Figure 5b and c]. The dental panoramic radiograph revealed a horizontally impacted upper left central incisor, missing lower second premolars bilaterally, and large radiopacity coronally involving dentin and pulp with advanced root resorption of the lower left deciduous first molar [Figure 5d]. The cone beam computed tomography slices confirmed a shorter root length of the impacted upper left central incisor in comparison to the adjacent erupted central incisor and a slightly curved root [Figure 5e].
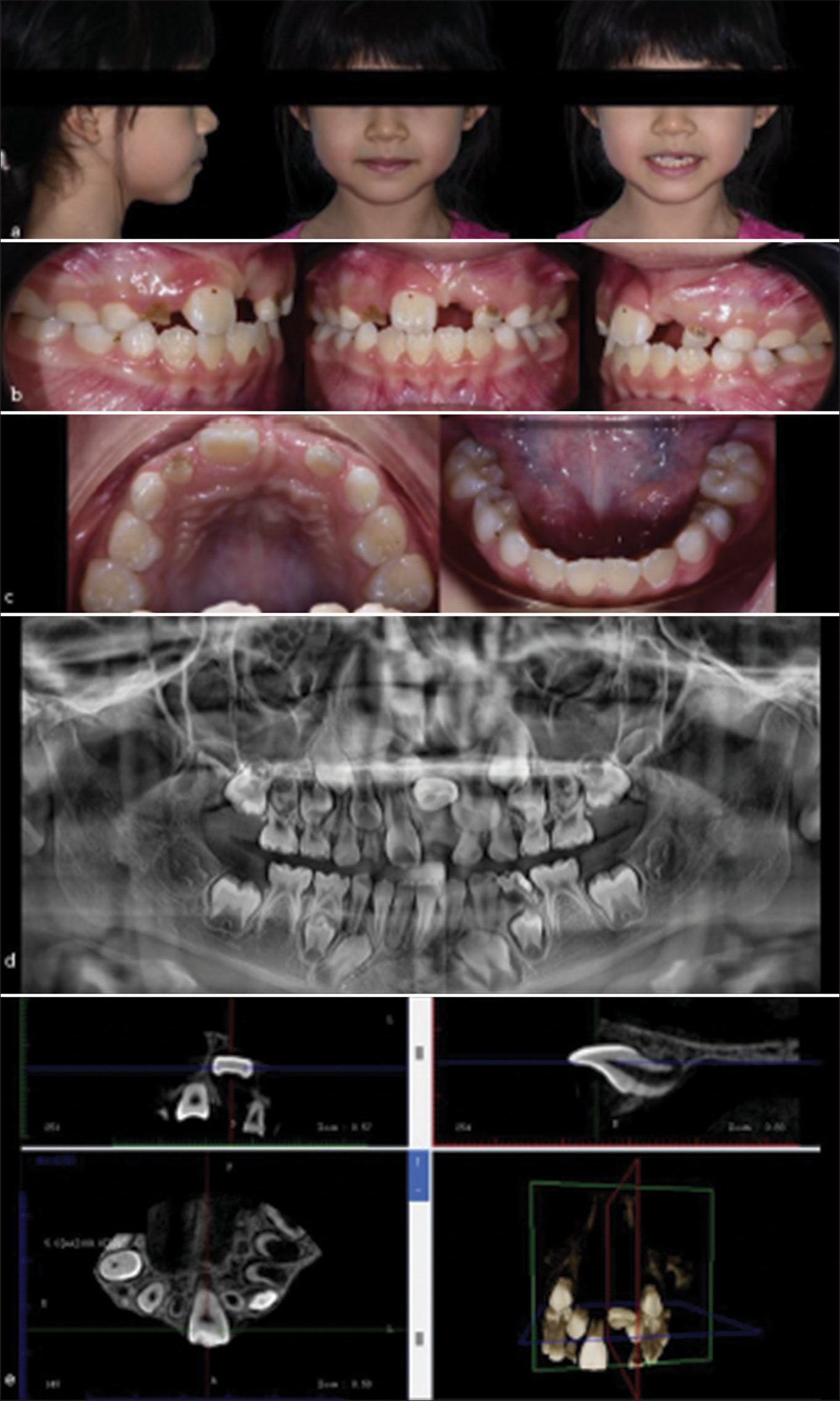
- 7-year 8-month-old girl presented with a horizontally impacted upper left central incisor. (a) Extraoral photographs (from left to right) depicting a skeletal Class I with average nasolabial angle at profile view, competent lips at rest and unesthetic appearance with unerupted upper left central incisor at frontal view when smiling. (b) Intraoral photographs (from left to right) showing right buccal, frontal, and left buccal intraoral view of a clinically missing upper left central incisor, poor oral hygiene, and carious upper deciduous lateral incisors. (c) Intraoral photographs (from left to right) showing upper occlusal view depicting early mixed dentition with erupted permanent right central incisor only with a mild space deficiency for the unerupted upper left central incisor. The lower occlusal view shows erupted permanent incisors with mild rotations and a large glass ionomer cement restoration at the distal of the lower left first deciduous molar. (d) The pre-operative dental panoramic radiograph depicts a horizontally impacted upper left central incisor, congenitally missing lower second pre-molars bilaterally, open apex of the contralateral upper central incisor, and severe root resorption of the upper deciduous lateral incisors indicating proximity to exfoliation time. (e) The pre-operative cone beam computed tomography slices illustrate a horizontal impaction of the upper left central incisor with a short and slightly curved root.
Treatment objective and treatment options
Like the previous cases (Case 1 and Case 2), the treatment objective was to align the impacted upper left central incisor through a surgical-orthodontic approach.
Treatment progress
A closed surgical exposure was performed with a gold chain bonded to the palatal surface of the impacted central incisor (American Orthodontics, Sheboygan, Wisconsin, USA), and the mobile upper deciduous lateral incisors were removed. After 2 weeks postoperatively, all the upper teeth were bonded using pre-adjusted edgewise fixed appliance 0.022 × 0.028-inch slot MBT prescription (Mini-Diamond series, Ormco Corp. Glendora, California, USA). A 0.012-inch nickel titanium archwire (NT3, American Orthodontics, Sheboygan, Wisconsin, USA) was thread through the gold chain link passively and ligated to the brackets. Subsequently, the archwire was changed to an upper 0.018-inch stainless steel wire (American Orthodontics, Sheboygan, Wisconsin, USA) with activation of the gold chain using a 0.012-inch nickel titanium archwire through the piggyback technique. Light continuous traction force was applied for 5 months until the impacted central incisor erupted at a level where a continuous 0.014-inch nickel-titanium wire (American Orthodontics, Sheboygan, Wisconsin, USA) could be ligated. A 0.018-inch stainless steel archwire was ligated in the next visit and the central incisors were brought together with the powerchain. A near-end dental panoramic radiograph was taken, and it showed root parallelism of the upper central incisors with comparable root lengths [Figure 6a].
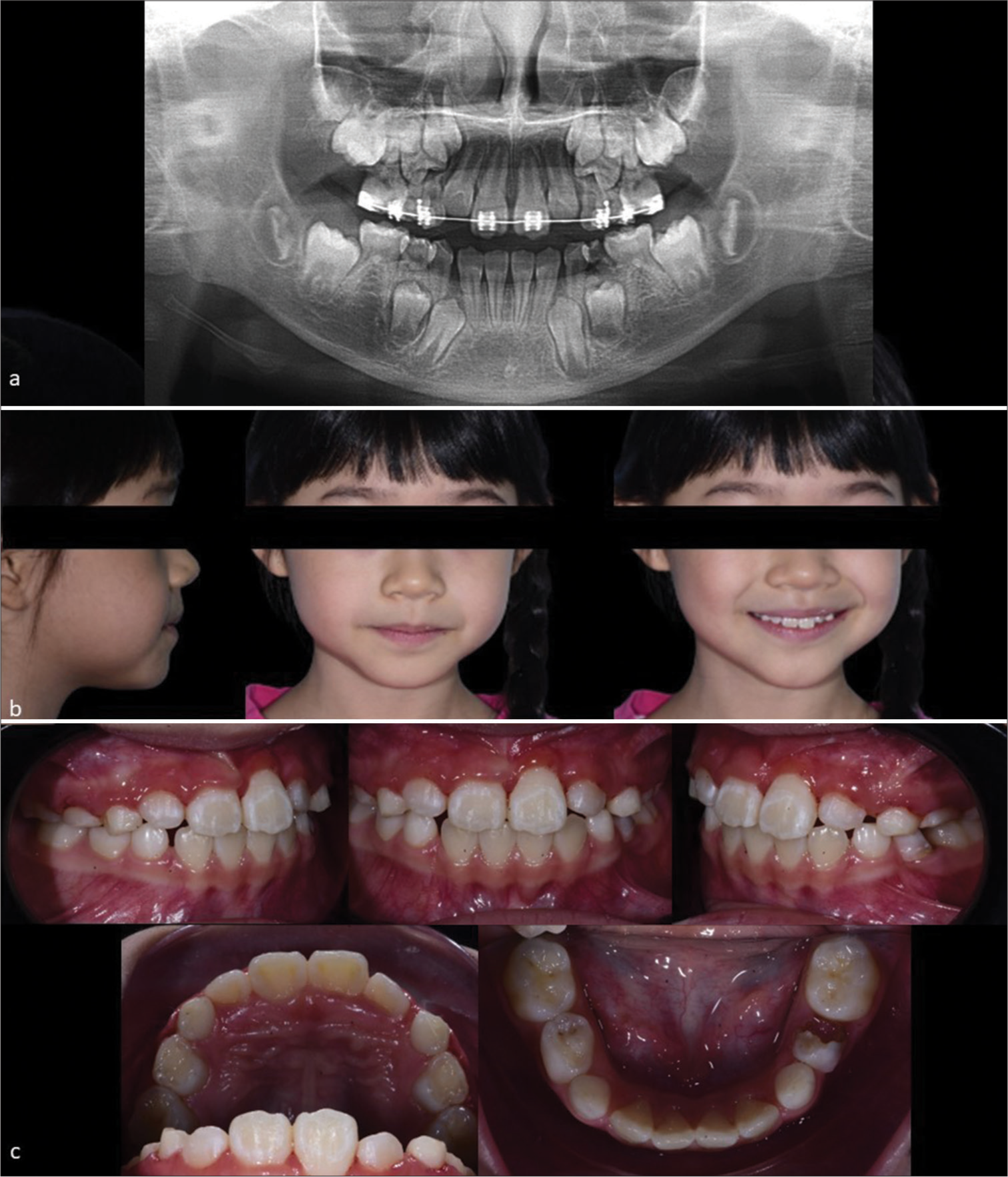
- 7-year 8-month-old girl presented with a horizontally impacted upper left central incisor. (a) The near-end treatment dental panoramic radiograph reveals a well-aligned upper left central incisor with good root parallelism and comparable root length as the adjacent central incisor. (b) Extraoral photographs after removing the fixed appliance illustrate a pleasant result with unchanged Class I profile, competent lips, a consonant smile arc, and average smile line. (c) Intraoral photographs at debond showing increased crown length of the upper left central incisor with gingival recession, average overbite and partially erupted upper lateral incisors. There was a dislodged restoration on the lower left deciduous first molar which was referred to the general practitioner for treatment.
Treatment results
The upper fixed appliance was debonded after 10 months of active treatment. The patient had a pleasing smile despite the increased crown length of the upper left central incisor and unequal gingival margins in comparison to the contralateral central incisor [Figure 6b and c].
DISCUSSION
Management of an impacted maxillary central incisor poses a challenge to the clinician as young patients (8 years old in Case 1, 9 years old in Case 2, and 7 years old in Case 3) are involved and surgical intervention is required. Although treatment success of closed surgical exposure and orthodontic alignment of an impacted maxillary central incisor are high, possible risks such as failure of tooth movement due to ankylosis, external root resorption, irregular root formation, gingival recession, devitalization, injury to adjacent teeth, and alveolar bone loss should be discussed with the parents of the child for informed consent before the procedure.[5,7] In addition, the need for the child’s cooperation to maintain oral hygiene and to care for the appliances should be communicated regularly to ensure a successful treatment.
In the early mixed dentition phase, incorrect bracket placement of the lateral incisor may lead to iatrogenic root resorption by the erupting canines. In case 2, the root of the upper right lateral incisor is seen angulated distally in the panoramic radiograph mid-treatment [Figure 3d]. This could be avoided by switching the lateral incisor brackets to reverse the prescription tip without affecting the torque or the bracket could be positioned mesiogingivally and slightly incisally to reduce the distal root tip.[8] There are many ways to mechanically erupt an impacted central incisor but the use of a piggyback technique as seen in all three cases provides a constant light traction force while the rigid base archwire would limit any unwanted effects on the anchor units.[9] The successfully aligned upper left central incisors showed minor gingival level discrepancies in all cases of which adjunctive periodontal surgery could be performed at a later time during the second phase of treatment. Irregular gingival margins were also found in one-third of the treated cases by Becker et al.[10] Therefore, close detail to surgical techniques such as the site of incision and the maintenance of good oral hygiene throughout treatment may improve periodontal outcomes.[10]
Early referral for the management of an impacted central incisor can reduce the overall treatment time as seen in Case 1 and Case 3 which took 7 months and 10 months, respectively, as compared to Case 2 which took 16 months [Table 1]. This is because additional time is required to create space for the impacted central incisor which was approximately 5 months in Case 2. A study by Chaushu et al. found that an average of 5 months is required to level, align, and open space and an additional 9 months for orthodontic traction after closed surgical exposure which is similar to Case 2.[5] Ideally, orthodontic treatment for phase 1 should be kept at a minimum to reduce the iatrogenic risks of fixed appliances. A vertical relapse was noted in case 1 and case 2 due to the reorganization of the periodontal fibers which could take up to 232 days.[11] Thus, a bonded retainer is advised after aligning the impacted central incisor.
| Case number | Gender | Age | Tooth affected | Treatment length | Outcome of treated central incisor |
|---|---|---|---|---|---|
| 1 | Male | 8 years 6 months | Upper left central incisor | 7 months | Mild gingival discrepancy and vertical relapse at 6-month review |
| 2 | Male | 9 years 2 months | 16 months | Minor vertical relapse and a shorter root length compared to the adjacent central incisor at 3-year review | |
| 3 | Female | 7 years 8 months | 10 months | Increased crown length of the upper left central incisor with gingival recession at debond |
CONCLUSION
Early intervention of an impacted maxillary central incisor through a surgical-orthodontic approach is often successful but treatment risks, duration, and retention regimen should be discussed with the parent for informed consent.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Unraveling impacted maxillary incisors: The why, when, and how. Int J Clin Pediatr Dent. 2021;14:149-57.
- [CrossRef] [Google Scholar]
- Impacted central incisors in the upper jaw in an adolescent patient: Orthodontic-surgical treatment-a case report. Appl Sci. 2022;12:2657.
- [CrossRef] [Google Scholar]
- Strategies for treating an impacted maxillary central incisor. Int Orthod. 2010;8:152-76.
- [CrossRef] [Google Scholar]
- Treatment of an impacted dilacerated maxillary central incisor. Am J Orthod Dentofacial Orthop. 2011;139:378-87.
- [CrossRef] [Google Scholar]
- Impacted central incisors: Factors affecting prognosis and treatment duration. Am J Orthod Dentofacial Orthop. 2015;147:355-62.
- [CrossRef] [Google Scholar]
- The morphology of impacted maxillary central incisors: A systematic review. Medicina (Kaunas). 2022;58:462.
- [CrossRef] [Google Scholar]
- Dental transposition of canine and lateral incisor and impacted central incisor treatment: A case report. Dental Press J Orthod. 2014;19:106-12.
- [CrossRef] [Google Scholar]
- Lateral incisor bracket positioning for phase I treatment. J Clin Orthod. 2021;55:227-8.
- [Google Scholar]
- Closed-eruption surgical technique for impacted maxillary incisors: A postorthodontic periodontal evaluation. Am J Orthod Dentofacial Orthop. 2002;122:9-14.
- [CrossRef] [Google Scholar]
- Toward a perspective on orthodontic retention? Am J Orthod Dentofacial Orthop. 1998;113:507-14.
- [CrossRef] [Google Scholar]







