Translate this page into:
Multislice computed tomography assessment of airway patency changes in the supine position following mandibular setback surgery for mandibular prognathism: A prospective 1-year follow-up study

*Corresponding author: Koji Iwai, Department of Orthodontics and Craniofacial Developmental Biology, Hiroshima University, Hiroshima, Japan. iwai@hiroshima-u.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Iwai K, Ueda H, Nagasaki T, Medina CC, Matsumura Y, Tanimoto K. Multislice computed tomography assessment of airway patency changes in the supine position following mandibular setback surgery for mandibular prognathism: A prospective 1-year follow-up study. APOS Trends Orthod 2021;11(2):106-15.
Abstract
Objectives:
The purpose of this study was to perform a three-dimensional analysis on the pharyngeal airway of supine patients who have undergone mandibular setback surgery, using multislice computed tomography (MSCT). We also measured the respiratory disturbance index pre- and post-surgery, using a portable sleep monitor.
Materials and Methods:
The subjects included two males and nine females who were diagnosed with mandibular prognathism at Hiroshima University Hospital and were scheduled to undergo the bilateral sagittal split osteotomy. Using a CT scanner, baseline MSCT images were obtained from the subjects before surgery for morphological analysis, and then the two further scans were obtained after mandibular setback surgery. All patients were provided with at-hoeme sleep monitor to use it both at baseline and approximately 1 year after surgery.
Results:
Middle and epiglottis pharyngeal space and cross-sectional area were significantly decreased immediately after setback surgery, but did not change further over the 1-year period. Mandibular setback was not associated with the development of sleep breathing disorder (SBD) during the 1-year follow-up period.
Conclusion:
We found no evidence that the reduction in the pharyngeal airway space immediately after mandibular setback surgery recovered significantly during the follow-up period, although mandibular setback was not associated with development of SBD.
Keywords
Airway
Mandibular setback surgery
Multislice computed tomography
Sleep breathing disorder
Sleep monitor
INTRODUCTION
In many Asian countries, mandibular setback surgery alone is performed routinely for correcting mandibular prognathism.[1,2] However, while the recovery of occlusion and improvement of esthetics are obtained by jaw corrective surgery, the soft tissues in the oral cavity and pharynx are forced to change by marked movement of the mandibular bones.[3-6] Tselnik and Pogrel[5] reported that the airway narrows at the oropharyngeal level after mandibular setback surgery is performed, based on a cephalometric study. Park et al.[7] also found oropharyngeal airway narrowing after such surgery in skeletal Class III patients using cone-beam computed tomography (CBCT) images. In recent years, it has been reported that the upper respiratory tract narrows and respiratory function during sleep changes after surgical mandibular setback.[8] Therefore, it has been suggested that the resulting new configuration of the pharyngeal airway may compromise air flow and predispose the patient to sleep breathing disorders (SBDs), including obstructive sleep apnea syndrome (OSAS).[7,9,10]
Contrastingly, several studies have shown that the narrowing of the pharyngeal airway space caused by mandibular setback osteotomy recovers gradually during the follow-up period and resolves over time.[11-14] Moreover, a recent systematic review has concluded that there is no clear association between mandibular setback surgery and the occurrence of OSAS.[15] Thus, whether multilevel compensatory change in the pharyngeal space is related to mandibular setback surgery remains controversial.
The literature contains reports of changes in pharyngeal airway morphology after mandibular setback surgery, estimated from cephalograms[4-6,9-12] and CBCT.[7,15,16] Many features, including changes in the size of the soft palate, inferiorly positioned hyoid bone, and reduced pharyngeal airway patency, are commonly observed in lateral cephalography,[17] which may be performed rapidly and at a low cost. In recent years, the number of studies assessing pharyngeal airway size has risen, with the increased availability of three-dimensional (3D) data obtained with CBCT. CBCT scanning accurately determines the cross-sectional area of the pharyngeal airway; images are obtained only in the axial plane but can be reconstructed for volumetric analysis. In addition, most previous CBCT studies have documented assessment of pharyngeal airway morphology with subjects in the upright position.[18-20] Nevertheless, OSAS is characterized by recurrent upper pharyngeal airway obstruction during sleep, in the supine position. Therefore, it is important to clarify the relationship between the morphological changes in the pharyngeal area of individuals in the supine position and symptoms of SBD in the surgical orthodontic treatment of skeletal mandibular prognathism.
The purpose of this study was to perform a 3D analysis on the pharyngeal airway of patients in the supine position who have undergone mandibular setback surgery, using multi-slice computed tomography (MSCT). Considering this, we hypothesized that the reduction in the airway dimensions, with SBD symptoms, immediately after mandibular setback surgery could recover gradually after 1 year.
MATERIALS AND METHODS
Subjects for this study included two males and nine females (mean age, 24.1 ± 7.2 years, and mean body mass index, 20.1 ± 1.9 kg/m2), inclusion criteria for this study included patients who were diagnosed with mandibular prognathism at Hiroshima University Hospital and were scheduled to undergo bilateral sagittal split osteotomy (average amount of mandibular setback 7.6mm ± 1.8 mm), no previous history of SBD, general good health including no systemic diseases. Patients who were scheduled for (1) two-jaw surgery, (2) tongue reduction surgery, (3) had been diagnosed with OSAS, or (4) had complications from serious systemic disease were excluded from the study. The Ethics Committee of Hiroshima University Hospital approved this prospective study’s protocol (E-56), and informed consent was obtained from each subject before treatment. This study has followed the guidelines stated in the Helsinki Declaration for clinical investigations.
Dentoskeletal analysis
To assess the success of the orthognathic surgery, several cephalometric measurements were evaluated and compared before and after surgery as stated below [Figure 1]:

- Dentoskeletal analysis. S: Center of Sella, N: Most anterior point of the frontonasal suture, also referred to as Nasion. A: Most posterior point on the anterior contour of the upper alveolar process, B: Most posterior point on the anterior contour of the lower alveolar process.
∠ SNA: Anteroposterior position of the maxilla, ∠ SNB: Anteroposterior position of the mandible, ∠ ANB: Anteroposterior relationship between the maxilla and the mandible, Overjet: The horizontal overlap of maxillary incisors over the mandibular incisors, Overbite: The vertical overlap of maxillary incisors over mandibular incisors.
Radiographic examination
Using an Aquilion ONE™ computed tomography (CT) scanner (Toshiba Medical Systems, Tochigi, Japan), baseline MSCT data were obtained from the subjects before surgery for morphological analysis (T0; pre-surgery, with a mean average time of 2.2 ± 1.3 months before surgery), and then the two additional scans were obtained after mandibular setback surgery (T1; immediately after surgery, with a mean average time of 2.5 ± 2.1 days and T2; the final scan obtained during post-surgical orthodontic treatment, with a mean average time of 11.1 ± 4.0 months). All patients were positioned with the Frankfurt horizontal (FH) plane perpendicular to the floor, with the facial midline parallel to the floor, and were asked to maintain this resting body position. The subjects were instructed to take a deep breath twice and to swallow once, and 5 s after this, the MSCT scanning was performed.
OsiriX ver 3.9 (Pixmeo SARL, Geneva, Switzerland) was used to analyze the digital imaging and communications in medicine (DICOM) files that were extracted from the MSCT data. The individual DICOM files were opened in OsiriX, and multiplanar reconstruction (MPR) was used to obtain cross-sectional slices, which were verified for landmark location and anatomic contours by the first author (K. I.).
Measurements
To measure the anteroposterior diameter, width, and cross-sectional area of the oropharyngeal region of interest (ROI), 5 distance variables (cm/cm2) were first defined on each MPR image using OsiriX [Figure 2a]. These measurement variables were chosen in accordance with those defined by Uozumi et al.:[21]

- The measurement variables. (a) Midline and median sagittal cross-sectional images. (b) The five measurement sites of the upper airway on a multiplanar reconstruction (MPR) image. The multislice computed tomography (CT) data were imported into OsiriX ver. 3.9, with the window level/window width (WL/WW) set to the CT-bone value of 500/2000 HU. Slice datasets were coordinated as follows. (1) The midline of a midpoint of two straight lines, connecting the uppermost and lower most ends of the bilateral zygomatic process observed in the coronal section, and a straight vertical line parallel to that midpoint, were drawn. (2) The median sagittal cross-sectional image was a sagittal section sliced by the midline, and the median sagittal and axial cross-sections were set to the posterior edge of the maxillary bone (posterior nasal spine). (3) Five distance points were established on the MPR image by verification on the median sagittal, axial, and coronal cross-sectional images. (4) The WL/WW was set to the airway component value of –662/724 HU, and the anteroposterior diameter, width, and cross-sectional area at the 5 distance points were measured on the axial cross-sectional images. Abbreviations: EPS: Epiglottis laryngeal space, IPS: Inferior pharyngeal space, MPS: Middle pharyngeal space, PPS: Palatal pharyngeal space, SPPS: Superior posterior pharyngeal space.
Palatal pharyngeal space (PPS): The anteroposterior depth of the pharynx measured between the posterior pharyngeal wall and the posterior nasal spine (PNS), on a line parallel to the FH plane that runs through the PNS.
Superior posterior pharyngeal space (SPPS): The anteroposterior depth of the pharynx measured between the posterior pharyngeal wall and the dorsum of the soft palate, on a line parallel to the FH plane that runs through the middle of the line from the PNS to the tip of the soft palate.
Middle pharyngeal space (MPS): The anteroposterior depth of the pharynx measured between the posterior pharyngeal wall and the dorsum of the tongue, on a line parallel to the FH plane that runs through the tip of the soft palate.
Inferior pharyngeal space (IPS): The anteroposterior depth of the pharynx measured between the posterior pharyngeal wall and the surface of the tongue, on a line parallel to the FH plane that runs through the most anterior point of the second cervical vertebra.
Epiglottis pharyngeal space (EPS): The anteroposterior depth of the pharynx measured between the posterior pharyngeal wall and the surface of the tongue, on a line parallel to the FH plane that runs through the tip of the epiglottis.
With respect to PPS, the minimum width was measured to clarify the boundary with the nasal cavity, and the cross-sectional area was defined as the area surrounded by the minimum width and the anteroposterior diameter, specifically. For the other four sites, the maximum anteroposterior diameter, width, and cross-sectional area were measured [Figure 2b]. An additional measurement variable, the minimum area (MA), corresponding to the narrowest part of the airway size, was determined; the anteroposterior diameter, width, and cross-sectional area of the MA were also measured cm/cm2; [Figure 3].
![The minimum area (MA) on multiplanar reconstruction (MPR) image. The slice datasets were coordinated as follows. (1) The median sagittal cross-sectional image was set using the T0 data (window level/window width [WL/WW] was set to the computed tomography-bone value of 500/2000 HU). (2) The craniocaudal direction M was set with the upper end as the palatal pharyngeal space and the lower end as the lowermost anterior point of the 4th cervical vertebrae (C4) on the MPR image by verification on the median sagittal, axial, and coronal cross-sectional images. (3) The WL/WW was set to the airway component value of –662/724 HU, the site where the cross-sectional area within that range was the narrowest, by verification on the axial crosssectional image, was set as the MA, and the anteroposterior diameter, width, and cross-sectional area were measured. (4) The median sagittal cross-sectional image was set using data obtained after the mandibular setback surgery (T1 and T2). The WL/WW was set to the airway component value of –662/724 HU,and the anteroposterior diameter, width, and cross-sectional area were measured again by verifying on the axial cross-sectional image.](/content/9/2021/11/2/img/APOS-11-106-g003.png)
- The minimum area (MA) on multiplanar reconstruction (MPR) image. The slice datasets were coordinated as follows. (1) The median sagittal cross-sectional image was set using the T0 data (window level/window width [WL/WW] was set to the computed tomography-bone value of 500/2000 HU). (2) The craniocaudal direction M was set with the upper end as the palatal pharyngeal space and the lower end as the lowermost anterior point of the 4th cervical vertebrae (C4) on the MPR image by verification on the median sagittal, axial, and coronal cross-sectional images. (3) The WL/WW was set to the airway component value of –662/724 HU, the site where the cross-sectional area within that range was the narrowest, by verification on the axial crosssectional image, was set as the MA, and the anteroposterior diameter, width, and cross-sectional area were measured. (4) The median sagittal cross-sectional image was set using data obtained after the mandibular setback surgery (T1 and T2). The WL/WW was set to the airway component value of –662/724 HU,and the anteroposterior diameter, width, and cross-sectional area were measured again by verifying on the axial cross-sectional image.
In the MPR images, the tongue cross-sectional area (TCA) was measured, in addition to the anteroposterior diameter, width, and cross-sectional area (cm2) of the five previously mentioned sites. The tongue area, outlined by the dorsum of the tongue surface and lines that connect the tongue tip, spina mentalis, hyoid, and base of the epiglottis, was divided by the mandibular plane into the anterior TCA (aTCA) and posterior TCA (pTCA) [Figure 4].
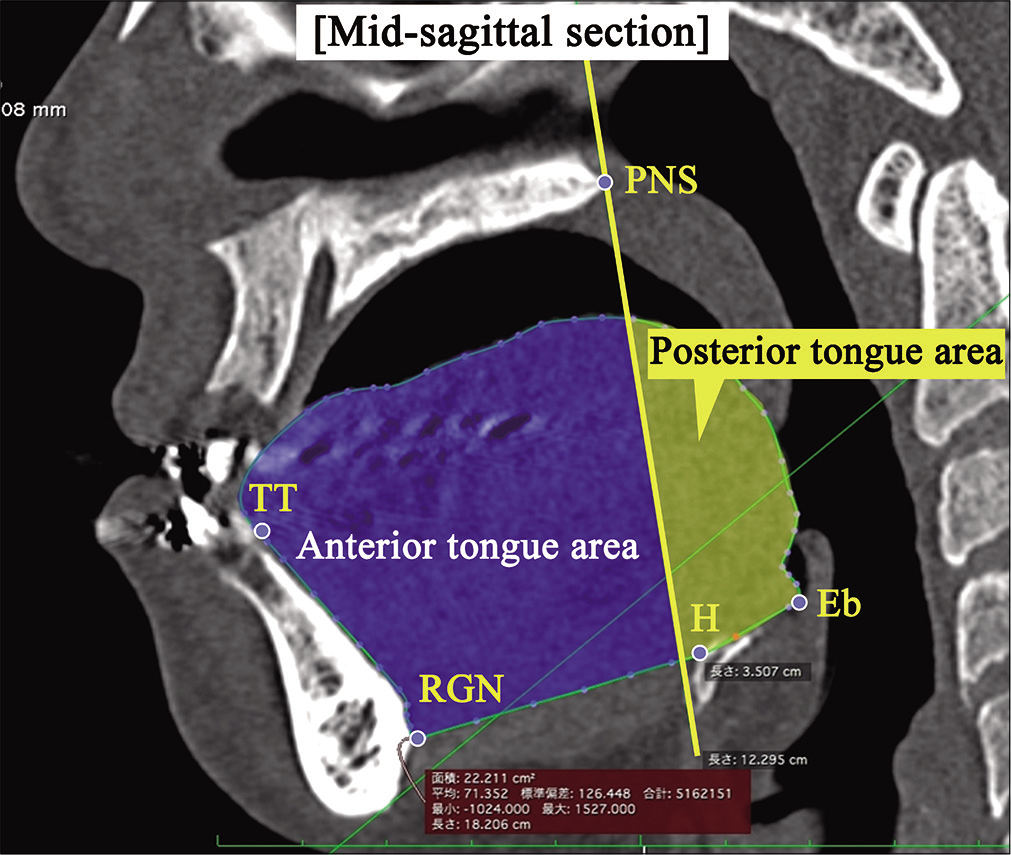
- Measurements of tongue cross-sectional area. TT: Tongue tip, RGN: A perpendicular line from the FH plane and symphysis where the mandibular symphysis intersects the most posterior point, H: The front most point of the hyoid bone, Eb: Epiglottis base; the lowest point in the epiglottis.
In addition, the volumes of aTCA and pTCA were divided by the total TCA to obtain their respective ratios. Further steps were performed to reconstruct 3D upper pharyngeal airway images for volumetric analysis. [Figure 5] depicts the method used to set the oro-hypopharyngeal region on the MPR image. Two points were defined to set this region: The reference points of the upper end were set as the PNS, and the lower end was set as C4 on the MPR image by verification on the median sagittal images. The area surrounded by the reference points was set as the oro-hypopharyngeal region (Window level/ Window width was set to the CT-bone value of 500/2000 HU). [Figure 6] depicts the airway volume ROI. The ROI of the airway was set by manually tracing all axial cross-sectional images of the oro-hypopharyngeal region. To establish the ROI, the movable region of the soft palate was positioned on the oral cavity side and was excluded from the range setting to clarify the boundary with the pharyngeal side. Finally, a 3D surface rendering was constructed using all the airway ROIs in the oro-hypopharyngeal region using MSCT data obtained before and after mandibular setback surgery. This was then used to measure the volumes of the upper airway in the oropharyngeal and hypopharyngeal regions in cm3 [Figure 7].
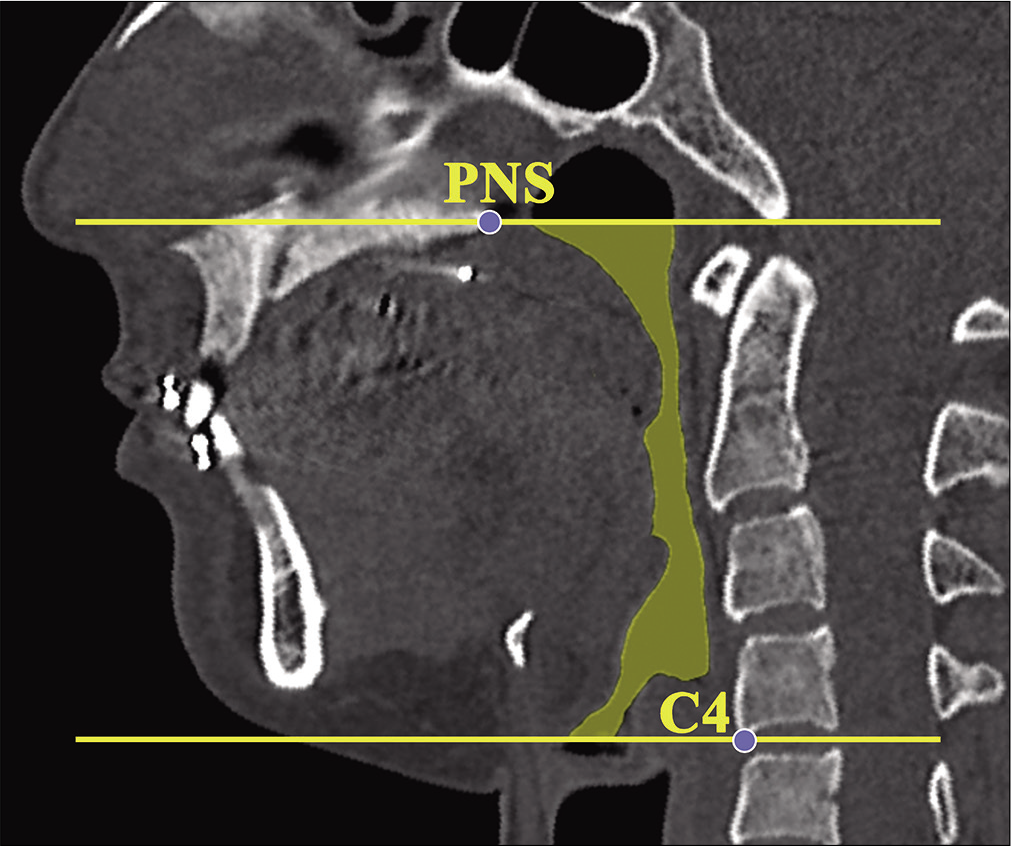
- The oro-hypopharyngeal region on the multiplanar reconstruction image. Abbreviation: WL/WW, window level/ window width.

- The region of interest for calculating the airway volume. Abbreviations: ROI: Region of interest, WL/WW, windowlevel/window width.
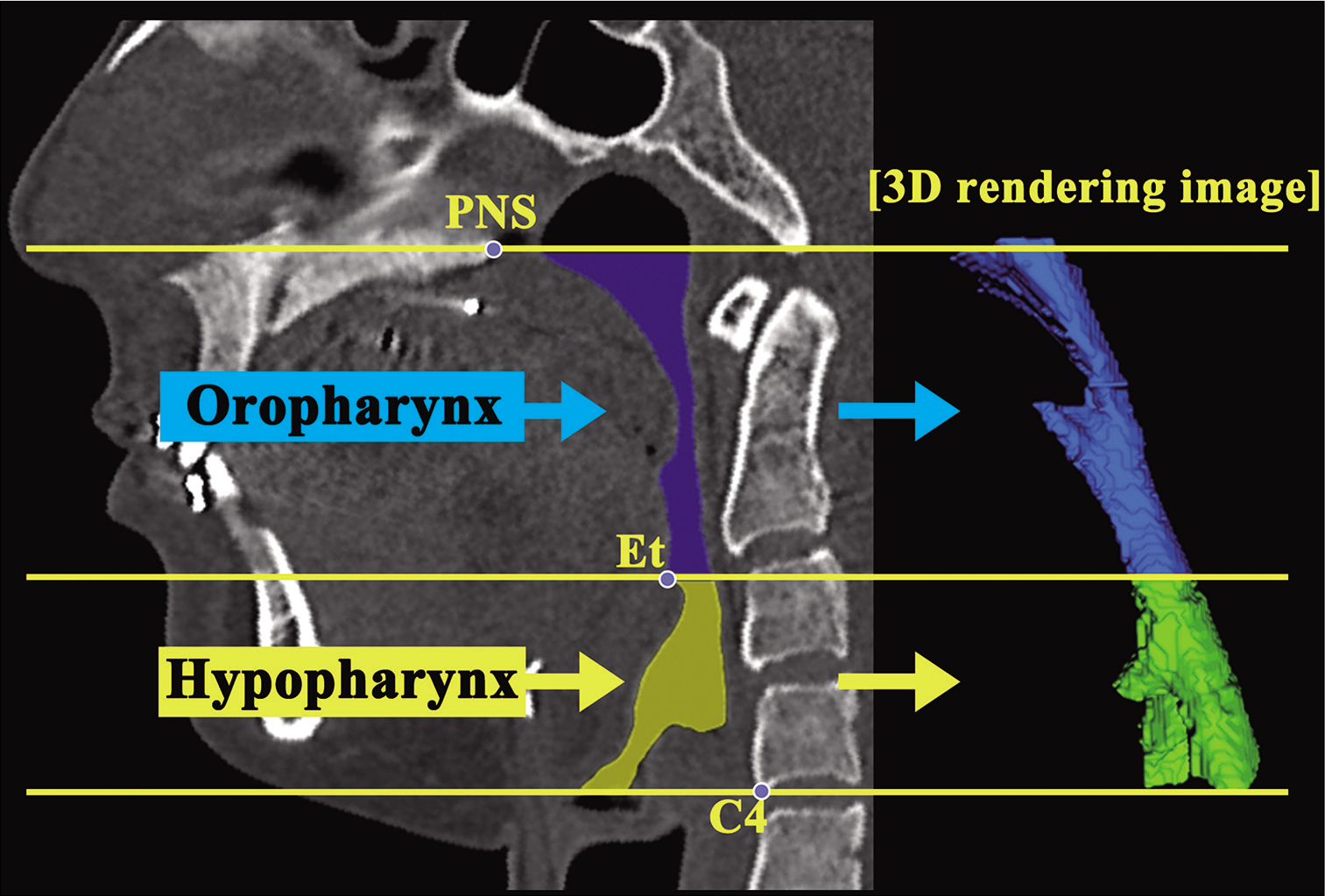
- An example of a three-dimensional image of the upper airway, oropharynx, and hypopharynx.
Sleep monitoring
All patients were provided with a type 3 at-home sleep monitor (Smart Watch PMP-300E, Pacific-Medico,® Tokyo, Japan) with instructions to use it both at baseline (T0; a mean average time of 1.7 ± 0.9 months before surgery), and approximately 1 year after surgery (T2; a mean average time of 9.1 ± 3.9 months after surgery). The sleep monitoring test, conducted on two consecutive nights, was performed at both T0 and T2. The average values of the test results were compared and analyzed. Patients were instructed to avoid testing on days in which they had consumed alcohol, felt physically weak, or had a lack of sleep. The following variables were used as indicators of SBD severity: The respiratory disturbance index (RDI), the apnea index (AI), hypopnea index (HI), oxygen desaturation index (ODI), and lowest arterial oxygen saturation (SpO2). The RDI, AI, HI, and ODI scores represented the number of events per hour of recording time. The number of total obstructive apnea, apnea, and hypopnea events per hour of sleep was detected; the number of times where blood oxygen levels decreased below a delimited threshold was recorded and statistically compared between T0 and T2.
Statistical analysis
Statistical analyses were performed using MedCalc Statistical Software version 18.11.6 (MedCalc Software bvba, Ostend, Belgium), unless otherwise specified. Descriptive statistics consisted of analyzing the average and standard deviation of parameter values. Differences in pharyngeal airway measurements among 3 MPR images were first tested with analyses of variance followed by post hoc Bonferroni tests. For SBD data, a paired t-test was used to compare the differences between T0 and T2. P = 0.05 was considered to be statistically significant.
RESULTS
Dentoskeletal changes
[Table 1] presents the changes in the skeletal and dental relationship of the subjects after mandibular setback surgery. ∠ SNB and ∠ ANB were significantly decreased and increased following mandibular setback, respectively. Moreover, normal overjet (2.8 mm ± 2.4 mm) and overbite (1.8 mm ± 0.9 mm) were obtained. At approximately 1 year following mandibular setback surgery, the skeletal relationship and craniofacial balance were observed to have improved markedly.
| T0 | T1 | T2 | P(T0–T1) | P(T1–T2) | P(T0–T2) | |
|---|---|---|---|---|---|---|
| SNA (°) | 81.2±3.6 | 81.3±3.5 | 81.2±3.4 | NS | NS | NS |
| SNB (°) | 83.4±4.3 | 80.0±4.3 | 80.1±4.2 | ** | NS | ** |
| ANB (°) | –2.3±2.5 | 1.3±2.4 | 1.1±2.3 | ** | NS | ** |
| overjet (mm) | –5.1±2.5 | 2.5±1.3 | 2.8±2.4 | ** | NS | ** |
| overbite (mm) | 0.9±1.3 | 1.7±1.1 | 1.8±0.9 | NS | NS | NS |
Mean±SD, ANOVA test, NS: Not significant, **P<0.01. SNA: Angle measurement from sella, to nasion, to point A, SNB: Angle measurement from sella, to nasion, to point B, ANB: Angle measurement from point A, to nasion, to point B.
Pharyngeal airway changes
The evaluation of the anteroposterior diameter, as obtained from MPR image data, demonstrated that MPS and EPS had significantly decreased between T0 and T1 (i.e., after surgery) [Table 2]. On the other hand, decreases in SPPS and MA did not reach statistical significance until T2. No significant changes in PPS or IPS were observed at either of the assessed time points [Table 2].
| Measurements | T0 | T1 | T2 | P (T0–T1) | P(T1–T2) | P(T0–T2) | |
|---|---|---|---|---|---|---|---|
| Anteroposterior diameter (cm) | PPS | 1.6±0.3 | 1.6±0.3 | 1.4±0.6 | NS | NS | NS |
| SPPS | 1.1±0.4 | 1.57±0.4 | 0.8±0.4 | NS | NS | * | |
| MPS | 1.4±0.4 | 1.6±0.3 | 1.1±0.4 | * | NS | NS | |
| IPS | 1.4±0.3 | 1.6±0.3 | 1.2±0.4 | NS | NS | NS | |
| EPS | 1.5±0.2 | 1.6±0.3 | 1.4±0.4 | * | NS | NS | |
| MA | 1.1±0.5 | 1.6±0.4 | 0.8±0.4 | * | NS | NS | |
| Width (cm) | PPS | 2.1±0.5 | 1.9±0.4 | 1.8±0.7 | NS | NS | NS |
| SPPS | 2.4±0.6 | 2.2±0.5 | 1.9±0.8 | NS | NS | NS | |
| MPS | 2.5±0.7 | 2.1±0.5 | 1.9±0.7 | NS | NS | NS | |
| IPS | 3.0±0.5 | 2.7±0.4 | 2.7±0.5 | NS | NS | NS | |
| EPS | 3.1±0.3 | 2.7±0.5 | 2.9±0.5 | * | NS | NS | |
| MA | 2.1±0.7 | 2.0±0.6 | 1.9±0.9 | NS | NS | NS | |
| Cross-sectional area (cm2) | PPS | 3.3±1.3 | 3.0±0.9 | 3.1±1.7 | NS | NS | NS |
| SPPS | 2.1±1.2 | 1.7±1.1 | 1.4±0.9 | * | NS | NS | |
| MPS | 2.3±1.2 | 1.8±1.0 | 1.6±0.8 | * | NS | NS | |
| IPS | 2.9±1.0 | 2.1±0.8 | 2.1±0.9 | * | NS | NS | |
| EPS | 2.8±0.9 | 2.1±0.7 | 2.4±0.7 | * | NS | NS | |
| MA | 1.6±1.0 | 1.1±0.8 | 1.0±0.7 | * | NS | NS | |
| Oro-hypopharyngeal airway (cm3) | 17.4±6.9 | 13.5±5.3 | 14.2±6.2 | * | NS | NS | |
| Oropharyngeal airway (cm3) | 10.1±4.6 | 7.8±4.0 | 7.3±4.3 | * | NS | NS | |
| Hypopharyngeal airway (cm3) | 7.3±2.7 | 5.7±1.6 | 6.9±4.7 | NS | NS | NS |
Mean±SD, ANOVA test, NS: Not significant, *P<0.05. PPS: Palatal pharyngeal space, SPPS: Superior posterior pharyngeal space, MPS: Middle pharyngeal space, IPS: Inferior pharyngeal space, EPS: Epiglottis laryngeal space, MA: Minimum area.
When comparing the widths of the six analyzed pharyngeal sites across the assessment time points, the only significant change was observed with EPS which decreased from T0 to T1. This difference was no longer statistically significant by T2 [Table 2].
With regards to the pharyngeal axial cross-sectional area, all sites, except PPS, exhibited a significant decrease from T0 to T1.
The ratio of aTCA to total TCA was significantly lower at both T1 and T2, compared to T0. In contrast, the ratio of pTCA to total TCA was significantly higher at both T1 and T2, compared to T0 [Table 3].
| T0 | T1 | T2 | P (T0–T1) | P(T1–T2) | P(T0–T2) | |
|---|---|---|---|---|---|---|
| aTCA/TCA (%) | 79.0±9.9 | 73.7±9.3 | 74.3±8.0 | * | NS | * |
| pTCA/TCA (%) | 21.0±9.9 | 26.3±0.9.3 | 25.7±8.0 | * | NS | * |
aTCA/TCA: Anterior tongue cross-sectional area/tongue cross-sectional area, pTCA/TCA: Posterior tongue cross-sectional area/tongue cross-sectional area. Mean±SD, ANOVA test, NS: Not significant, *P<0.05.
In the volumetric analysis, significant decreases were observed in both the oro-hypopharyngeal and oropharyngeal region volumes between T0 and T1, whereas their volumes at T2 were nearly the same as at T1 [Table 2]. The hypopharyngeal region volumes were not significantly different across the assessed time points.
Sleep monitoring
[Table 4] presents the evaluation of the sleep-breathing data obtained with the portable sleep monitor. Mean RDI, AI, HI, ODI, and lowest SpO2 were in the normal range for all patients and did not change significantly after mandibular setback surgery.
| T0 | T2 | P | |
|---|---|---|---|
| RDI | 3.3±2.1 | 3.5±0.9 | NS |
| AI | 1.4±1.5 | 1.1±0.4 | NS |
| HI | 2.0±2.0 | 2.4±0.8 | NS |
| ODI | 4.3±2.5 | 5.3±1.6 | NS |
| Lowest SpO2(%) | 89.2±4.1 | 85.7±3.9 | NS |
Mean±SD, Paired t-test, NS: Not significant, *P<0.05. RDI: Respiratory disturbance index, AI: Apnea index, HI: Hypopnea index, ODI: Oxygen desaturation index, Lowest SpO2: Lowest arterial oxygen saturation.
DISCUSSION
This prospective clinical study used MPR images obtained by MSCT with patients in the supine position, to assess the morphological changes of the pharyngeal airway following mandibular set-back surgery for correcting excessive mandibular prognathism. It also determined the influence of these changes on the development of SBD. In this study, the pharyngeal airway size reduction immediately after mandibular setback surgery did not recover significantly during the follow-up period. In addition, mandibular setback was not associated with the development of SBD during the 1-year follow-up period.
Many studies have evaluated the changes that occur in the upper airway after orthognathic surgery using lateral cephalometric radiographical analysis mainly because of its low exposure dose, simplicity, and low cost.[4-6,9-12] However, two-dimensional (2D) measurements have limitations, including difficulties with the differentiation of anatomical structures, as well as the inability to make volumetric determinations. Conversely, CBCT has significant advantages over conventional radiography. 3D records provide a considerable advantage of allowing viewing of objects at their actual (100%) size, without concerns about distortion, magnification, or superimposed anatomical objects, which are typical drawbacks of 2D film images.[22] CBCT allows not only linear measurements but also the measurement of the cross-sectional area of the airway, including the airway, tongue, and soft palate, in three planes of space.[7,15,16] Besides this, analysis of 3D models reconstructed from CBCT images allows for a more precise evaluation of the post-operative changes in the pharyngeal airway space.[23] However, most previous CBCT studies have evaluated airway caliber with the subjects in the upright position.[7,15-20] Yet, Martin et al.[24] have reported that body positions affect upper airway size. Patients with OSAS exhibited smaller decreases in the upper airway cross-sectional area when their body position changed from the upright to the supine position. The upper airway and surrounding soft-tissue structures may be influenced by gravitational forces in the supine position during sleep; therefore, it is of significant importance that MSCT data of patients who have undergone mandibular setback are obtained with the patients in the supine position.
In the present study, MPR images showed a significantly decreased anteroposterior diameter of the airway due to the significant decrease in MPS, EPS, and MA when comparing pre-operative with 1-week post-operative values (T0–T1). For most of the assessed airway size parameters in the cross-sectional area, significant decreases were observed, except for PPS, at T1. In the volumetric analysis, the total airway size and oropharyngeal region presented a significant decrease at T1. This is thought to explain why posterior movement of the mandible decreased the intraoral volume and significantly increased the posterior tongue area; with dorsiflexion, the tongue lifted upwards, and most sites below PPS mainly narrowed.
The previous studies on mandibular setback surgery and airway changes in skeletal Class III patients have yielded similar results to our study. In CBCT evaluation studies, Canellas et al.[15] demonstrated a reduction in the pharyngeal airway and a decrease in MA in patients who underwent mandibular setback surgery. In contrast, two previous cephalometric studies[11,12] demonstrated that the pharyngeal airway morphology that had changed after mandibular setback surgery can gradually relapse and adapt in the long-term, although a full recovery was not achieved within 1 year. Jeon et al.[12] reported that the pharyngeal airway recovered shortly after surgical setback repositioning of the mandible and continued to adapt, achieving 80–90% of baseline measurements by 12 months after surgery. We did not find significant recovery of the pharyngeal airway after 1 year (T2), although some patients showed an increased upper airway size between T1 and T2. Therefore, the hypothesis about changes in pharyngeal airway morphology was rejected.
It might be speculated that this study compared the data of about 1-week pre- and post-surgery, and at that time, swelling of soft tissues occurred due to the invasiveness of the procedure, and stenosis of the pharyngeal airway was likely to occur. In other words, the increase in airway size may partly be explained by disappearance of the effect of inflammation on airway size by T2. Therefore, we performed a continuous assessment in this prospective study. During the 1-year follow-up period, no measurements of the airway size showed any significant increase between T1 and T2, and few variables, such as SPPS and MA in the anteroposterior diameter, showed a significant decrease from T1 to T2.
Although there are not many reports of clinical respiratory disturbance caused by a decrease in airway size, Riley et al.[25] reported that, in two cases of patients with mandibular prognathism who underwent mandibular retrusion surgery, OSAS might have developed due to the airway size decrease. However, in the present study, no significant increases were observed in SBD parameter values after 1-year of follow-up. These results were similar to those of other studies. Wenzel et al.[3] reported that a decrease in pharyngeal airway size after mandibular setback surgery did not necessarily increase respiratory resistance. Canellas et al.[18] concluded that reduction in pharyngeal airway space was not accompanied by signs or symptoms of OSAS after orthognathic surgery in skeletal Class III patients. In the present study, patients also showed no SBD symptoms, despite a narrowing of the pharyngeal airway. This may be because patients with mandibular prognathism essentially have a wide pharyngeal airway. Samman et al.[26] and Hochban et al.[27] reported that, since skeletal Class III dysplasia patients have a wider upper airway than the normal population, the decrease caused by surgery would still place them in the normal range. Therefore, the occurrence of SBD after corrective surgery for skeletal Class III dysplasia patients may be rare. In addition, in our study, the mean mandibular setback was 7.6 mm (range 4.3–10.3 mm). Tselnik and Pogrel[5] showed a strong correlation between the amount of mandibular setback and the decrease in the pharyngeal airway space. The average mandibular setback in their study was 9.7 mm. Therefore, patients with potential OSAS symptoms and undergo a large mandibular setback may be prone to developing SBD in the future.
This study had some limitations, including its small sample size and the fact that the patients were awake during the MSCT examination. Techniques for obtaining MSCT data during sleep could provide additional information about the morphological changes in pharyngeal airway volume. However, such techniques are limited to research conditions and might be impractical in a large group of patients. To understand the pathogenesis of SBD and the clinical influence of mandibular setback surgery on airway pharyngeal morphology more in depth, further investigations that focus on 3D airway configuration analysis at various sites that are affected by mandibular setback surgery are required, with a larger number of patients, and careful long-term monitoring.
CONCLUSION
In this study, the pharyngeal space in patients in the supine position was significantly decreased immediately after mandibular setback surgery. No evidence was found for significant recovery during the follow-up period. Furthermore, mandibular setback surgery was not associated with the development of SBD during the 1-year follow-up period. Further longer-term studies with careful monitoring of changes in pharyngeal airway size after mandibular setback surgery should be performed to verify these findings.
Statement of clinical relevance
Reduction in pharyngeal airway size immediately after mandibular setback surgery, based on MSCT in supine patients, did not recover significantly by 1-year postoperatively, and was not associated with the development of sleep breathing disorder during this follow-up period.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Satisfaction with orthognathic surgery of skeletal Class III patients. Am J Orthod Dentfacial Orthop. 2015;148:827-37.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in stomatognathic function induced by orthognathic surgery in patients with mandibular prognathism. J Oral Maxillofac Surg. 2007;65:444-51.
- [CrossRef] [PubMed] [Google Scholar]
- Relationships of changes in craniofacial morphology, head posture, and nasopharyngeal airway size following mandibular osteotomy. Am J Orthod Dentofacial Orthop. 1989;96:138-43.
- [CrossRef] [Google Scholar]
- Effects of mandibular retropositioning, with or without maxillary advancement, on the oro-naso-pharyngeal airway and development of sleep-related breathing disorders. J Oral Maxillofac Surg. 2010;68:2431-6.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282-5.
- [CrossRef] [Google Scholar]
- Predicting the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2005;63:1509-14.
- [CrossRef] [PubMed] [Google Scholar]
- The structural changes of pharyngeal airway contributing to snoring after orthognathic surgery in skeletal Class III patients. Maxillofac Plast Reconstr Surg. 2017;39:22.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of orthognathic surgery on oropharyngeal airway: A meta-analysis. Int J Oral Maxillofac Surg. 2011;40:1347-56.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of orthognathic surgery on ventilation during sleep. Int J Oral Maxillofac Surg. 2011;40:146-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of pharyngeal airway space changes after bimaxillary orthognathic surgery with a 3-dimensional simulation and modeling program. Am J Orthod Dentofacial Orthop. 2014;146:477-92.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term changes in pharyngeal airway morphology after mandibular setback surgery. Am J Orthod Dentofacial Orthop. 2004;125:556-61.
- [CrossRef] [PubMed] [Google Scholar]
- Does the pharyngeal airway recover after sagittal split ramus osteotomy for mandibular prognathism? J Oral Maxillofac Surg. 2016;74:162-9.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1994;9:285-90.
- [Google Scholar]
- Alterations of hyoid bone position and pharyngeal depth and their relationship after surgical correction of mandibular prognathism. Am J Orthod Dentofacial Orthop. 1991;100:259-65.
- [CrossRef] [Google Scholar]
- Sleep-disordered breathing following mandibular setback: A systematic review of the literature. Sleep Breath. 2016;20:387-94.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional upper-airway changes with maxillomandibular advancement for obstructive sleep apnea treatment. Am J Orthod Dentofacial Orthop. 2014;146:385-93.
- [CrossRef] [PubMed] [Google Scholar]
- Cephalometric comparison of obstructive sleep apnea patients and healthy controls. Eur J Dent. 2013;71:48-54.
- [CrossRef] [Google Scholar]
- Oropharyngeal airway in children with Class III malocclusion evaluated by cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;136:318.e1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional analysis of the pharyngeal airway morphology in growing Japanese girls with and without cleft lip and palate. Am J Orthod Dentofacial Orthop. 2012;141:S92-101.
- [CrossRef] [PubMed] [Google Scholar]
- Upper airway obstuction in Class II patients. Effects of Andresen activator on the anatomy of pharingeal airway passage, Cone beam evalution. Stomatologija. 2015;17:124-30.
- [Google Scholar]
- A comparative study on the morphological changes in the pharyngeal airway space before and after sagittal split ramus osteotomy. J Hard Tissue Biol. 2012;21:35-42.
- [CrossRef] [Google Scholar]
- Cone beam computed tomography evaluation after palatal expansion and orthodontics. J World Fed Orthod. 2013;2:e9-13.
- [CrossRef] [Google Scholar]
- Changes in position of the hyoid bone and volume of the pharyngeal airway after mandibular setback: Three-dimensional analysis. Br J Oral Maxillofac Surg. 2019;57:29-35.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of posture on airway caliber with the sleep-apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1995;152:721-4.
- [CrossRef] [PubMed] [Google Scholar]
- Obstructive sleep apnea syndrome following surgery for mandibular prognathism. J Oral Maxillofac Surg. 1987;45:450-2.
- [CrossRef] [Google Scholar]
- Cephalometric study of the upper airway in surgically corrected Class III skeletal deformity. Int J Adult Orthodon Orthognath Surg. 2002;17:180-90.
- [Google Scholar]
- Mandibular setback for surgical correction of mandibular hyperplasia-does it provoke sleep-related breathing disorders? Int J Oral Maxillofac Surg. 1996;25:333-8.
- [CrossRef] [Google Scholar]






