Translate this page into:
Time-saving scoring chart for the American Board of Orthodontics’ objective grading system
First Author: Dr. Pratap Saini

*Corresponding author: Dr. Harpreet Singh, Department of Orthodontics and Dentofacial Orthopedics, ESIC Dental College and Hospital, Sector 15, Rohini, New Delhi, India. drhpreet_mamc04@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Saini P, Maurya RK, Singh H. Time-saving scoring chart for the American Board of Orthodontics’ objective grading system. APOS Trends Orthod 2020;10(4):262-5.
Abstract
Objective grading system is indispensable in contemporary orthodontic scenario to help elevate clinical proficiency and quality of care. Simplification of the format of grading system is necessary not only for easy chair side documentation but also for comparative pre- and post treatment assessment. The aim of this article is to propose a simple, practical, and time-saving scoring chart for scoring each criterion of the objective grading system.
Keywords
Objective grading
Orthodontic
Scoring chart
Time saving
INTRODUCTION
With the mission of establishing the highest standards of clinical excellence in orthodontics,[1] the American Board of Orthodontics (ABO) introduced “Objective Grading System” (OGS) to the orthodontic fraternity in 1999 to evaluate cases submitted by candidates as part of the Phase III examination for board certification. The ABO recommends that clinicians use their scoring index to evaluate their cases before submitting them to the board. ABO-OGS is a valuable tool for standardized assessment and reporting of cases treated by orthodontists from different sociodemographic backgrounds.[2] Moreover, participation in the certification process encourages every orthodontist to achieve his or her highest level of clinical proficiency and strive to elevate the quality of orthodontic care in the future.[2] The validity, reliability, and precision of ABO-OGS index in evaluation of the post-treatment occlusal outcome have been well documented in literature.[3]
ABO-OGS is a great tool to integrate into clinical practice, allowing orthodontic graduate students and clinicians to evaluate their cases at different stages of treatment like at finishing stage, assessing any necessary corrections required before debonding, or evaluating quality of post-treatment outcome and long-term post-treatment changes.[4-8]
ABO-OGS consists of seven distinct study model-scoring criteria, namely alignment, buccolingual inclination, overjet, occlusal contacts, occlusal relationships, marginal ridges, and interproximal contacts and one panoramic radiographic criterion – root angulation.[2] Each criterion is scored for specific teeth in upper and lower dentition; like all teeth in upper and lower arches are scored for alignment, while buccolingual inclination and occlusal contacts are scored for 1st premolar to 2nd molar bilaterally in maxillary arch and 2nd premolar to 2nd molar in mandibular arch (1st premolars are not scored in lower arch). Occlusal relationships are scored for canine to 2nd molar bilaterally in maxillary arch but not scored in mandibular arch. Only maxillary dentition is scored for overjet while mandibular dentition is not scored.
In 2006, Owens et al.[9] described a “Case management form” (CMF) instrument for enhancing the objectivity of the ABO clinical examination. They further stated that continuous refinements of the testing instruments and examination systems are deemed indispensable to achieve an impartial and effective examination process. More recently, Chung et al.[10] stressed the need for shifting to a scenario-based clinical examination which will offer an improved, valid, reliable, and fair testing method while increasing accessibility and complementing residency curricula.
Very often, it is very difficult to remember and score for eight criteria to evaluate a case for ABO’ OGS. With increased patient load and pressure, many busy clinicians also find the format of OGS too cumbersome and complex and consider the grading system a straining herculean task. There is no handy chart or table available for noting the scores for different criteria.
We, hereby, propose a new, easy to fill, and time-saving scoring chart to note down the scores for each criterion of ABO’ OGS.
METHODOLOGY
Explanation of the new scoring chart for ABO’ OGS
This chart in a one-page landscape format provides a checklist for clinicians while evaluating their cases [Figure 1].
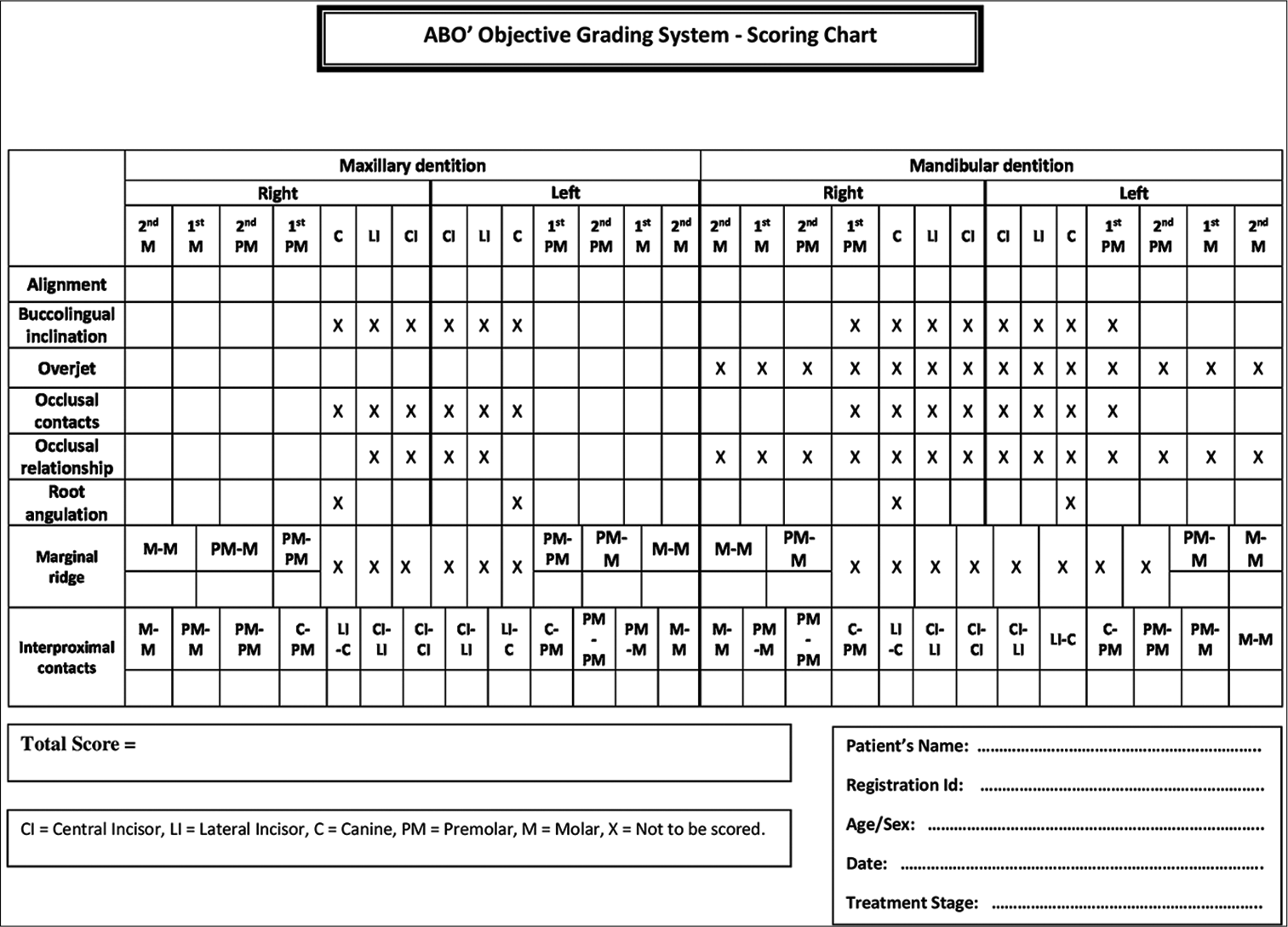
- Scoring chart for the American Board of Orthodontics’ Objective Grading System.
The empty boxes are provided for the teeth to be scored, whereas the boxes for the teeth which are not to be scored are marked with cross “X”. The total score is then recorded in a separate block to complete the candidate’s responsibility in completing the chart. Example of a filled-in scoring chart is illustrated in [Figure 2].
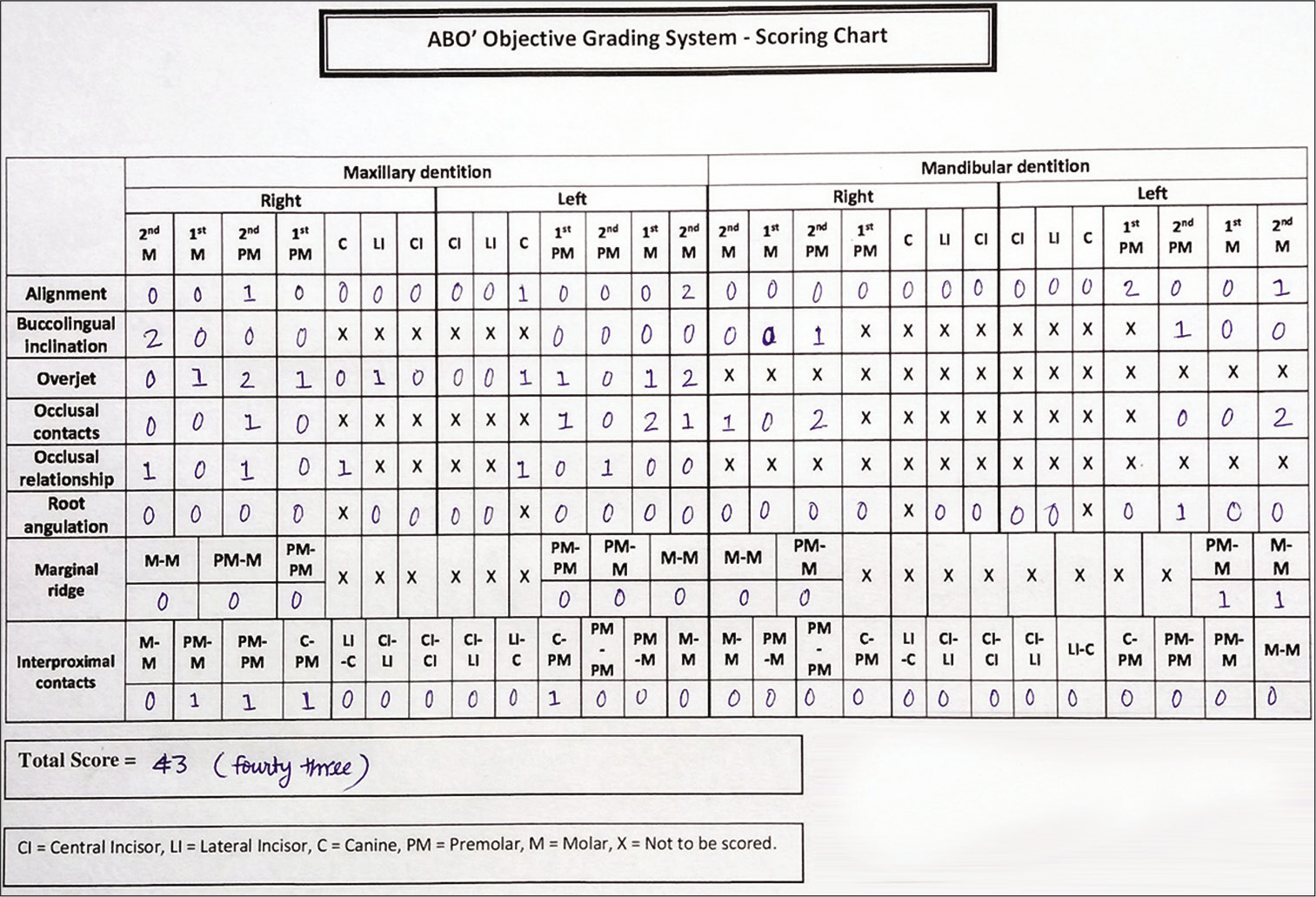
- Example of a filled-in scoring chart of a patient.
To check and ensure validity of our newly created time-saving chart for scoring ABO-OGS index, a panel comprising 50 experienced orthodontists (having at least 5 years of clinical experience in orthodontics) was constituted, who already knew and used this index for evaluating their cases. We distributed our scoring chart to them and requested them to score any two post-treatment case models using two different approaches and also to note time taken by these two approaches:
Scoring using conventional approach (Approach 1) as described by ABO.
Scoring using our newly designed scoring chart (Approach 2).
Statistical analysis
Processing of the data was done using SPSS version 21.0 software for Windows (IBM Corporation, Armonk, NY). Application of Shapiro–Wilk t-test showed normal distributions of data variables. The data regarding the two approaches were evaluated using the unpaired t-test. Tests of significance were 2 tailed, and the minimum level of significance was set at P < 0.05.
RESULTS
After getting the results by 50 orthodontists, we calculated average time taken for ABO-OGS index by these two approaches. Average time taken by conventional approach was 16 min 30 sec, and average time taken by filling our scoring chart was 8 min 15 sec. Significant reduction in scoring time was observed with the newly designed scoring chart, i.e., approach 2 (approximately half the time) when compared with scoring using conventional approach [Table 1].
| Variable | Approach 1 (using conventional ABO method) |
Approach 2 (using new scoring chart) |
|---|---|---|
| n | 50 | 50 |
| Mean difference | 16.2133 | 7.8167 |
| SD | 0.9884 | 0.5824 |
| SE | 0.2552 | 0.1504 |
| P value | 0.0001* | |
SD: Standard deviation; SE: Standard error; P < 0.05 is significant
DISCUSSION
Orthodontic graduate students and clinicians can conveniently assess their cases using this chart to get scores for ABO’ OGS at any stages of treatment. We also observed that orthodontists found this scoring chart very convenient to use, and they were also able to easily pinpoint the tooth at a glance which was at fault for a particular ABO’ OGS criteria. In addition to objectivity, the validity and reliability of the measurements contribute to the usefulness of this scoring chart.
Advantages of the tabulated scoring chart for OGS:
The novel scoring chart is reasonably time-saving (can be completed by the candidate in approximately 8–10 min) and eases the strain of frequent documentation required for continued self-reflection and evaluation, thus fostering increased confidence for the candidate’s self-assessment and presentation at the clinical examination.
It facilitates easy comparison and interpretation of different components of scoring criteria.
It aids in more objective analysis of the adequacy and quality of orthodontic treatment.
It pinpoints unique characteristics of different criteria at a glance.
Future large-scale studies involving orthodontists from different social and demographic backgrounds and allowing for assessment of the reliability and validity of the measurements of the ABO-OGS using the novel time-saving scoring chart will help make it a promising tool for integration into contemporary orthodontic practice.
CONCLUSION
This simple and practical tabulated scoring chart can prove to be a promising time-saving tool for scoring each criterion of the objective grading system.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- American Board of Orthodontics Information for the Candidates. (4th ed). St Louis, MO: American Board of Orthodontics; 1997.
- [Google Scholar]
- Objective grading system for dental casts and panoramic radiographs. Am J Orthod Dentofacial Orthop. 1998;114:589-99.
- [CrossRef] [Google Scholar]
- Validation of the American board of orthodontics objective grading system for assessing the treatment outcomes of Chinese patients. Am J Orthod Dentofacial Orthop. 2013;144:391-7.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of orthodontic treatment performed by orthodontists and general dentists. Angle Orthod. 2012;82:102-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of 0.018-inch and 0.022-inch bracket slot using the ABO objective grading system. Angle Orthod. 2010;80:528-32.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term occlusal changes assessed by the American board of orthodontics' model grading system. Am J Orthod Dentofacial Orthop. 2014;145:173-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term posttreatment changes measured by the American board of orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2005;127:444-50.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcome in a graduate orthodontic clinic using the American board of orthodontics grading system. Am J Orthod Dentofacial Orthop. 2002;122:451-5.
- [CrossRef] [PubMed] [Google Scholar]
- The case management form of the American board of orthodontics. Am J Orthod Dentofacial Orthop. 2006;129:325-9.
- [CrossRef] [PubMed] [Google Scholar]
- American board of orthodontics: Time for change. Am J Orthod Dentofacial Orthop. 2018;153:321-3.
- [CrossRef] [PubMed] [Google Scholar]






