Translate this page into:
Treatment effects of myofunctional appliances in different jaw rotations in Class II division 1 malocclusion
Address for Correspondence: Prof. Gauri S. Vichare, Department of Orthodontics and Dentofacial Orthopedics, Bharati Vidyapeeth Dental College and Hospital, Bharati Vidyapeeth Deemed University, Pune, Maharashtra, India. E-mail: drgauriv@gmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim
This retrospective study was conducted to determine skeletal, dentoalveolar changes in children treated with Twin Block or activator for the treatment of Class II Division 1 malocclusion with different jaw rotations.
Materials and Methods
Standardized lateral cephalograms of 32 patients (18 boys, 14 girls) between the ages of 11 and 14 years were chosen and divided into two groups, high angle (FMA >27) and low angle (FMA <20). Cephalograms were taken at T1 (pre-treatment) and T2 (after one year of myofunctional therapy).These were manually traced and analysed.
Results
The results showed statistically significant increase in SNB angle, VRP-Pog due to forward movement of the mandible. The overjet reduced significantly due to retroclination of upper incisors and proclination of lower incisors in both groups.
Conclusion
It was concluded that both high angle and low angle groups responded equally well to myofunctional therapy showing significant skeletal and dentoalveolar changes.
Keywords
Cephalometrics
Class II treatment
functional appliances
jaw rotations
INTRODUCTION
Class II malocclusions can manifest in various skeletal and dental configurations.[1-5] Most Class II patients have a deficiency in the anteroposterior position of the mandible.[6] Several treatment options are available for managing Class II problems, and functional appliances have been used for many years in the treatment of Class II Division 1 malocclusions. Several varieties of functional appliances are currently in use that aim to improve skeletal imbalances.[7-9] The term functional appliance refers to a variety of orthodontic appliances designed to induce a change in activity of the various muscle groups that influence the function and position of the mandible in order to transmit forces to the dentition and the basal bone. Alteration of maxillary growth, possible improvement in mandibular growth and position, and change in dental and muscular relationships are the expected effects of these functional appliances.[10]
It has been claimed that the forward growth of the maxilla can be inhibited,[3-16] redirected,[17] or unaffected[11-14] by functional appliances. The effect of functional appliances on mandibular growth is controversial. Some authors suggested that mandibular growth can be increased with functional appliance treatment,[15-17] but others believe the appliances have no real effect on mandibular length.[18,19] However, most researchers agree that the appliances produce retroclination of the maxillary incisors[10,14,16] and proclination of the mandibular incisors.[18] There is no consensus on how the molar correction occurs.
Two of the more popular functional appliances used today are the activator[18] and Clark’s Twinblock.[20] Few studies have compared the effects of these appliances.[21,22] Both are tooth-borne, but the twin-block is designed for full-time wear to take advantage of all functional forces applied to the dentition, including the forces of mastication.
According to Schudy,[23] the rotation of the mandible is the result of disharmony between vertical growth and antero-posteior or horizontal growth of the jaws. Accordingly, he describes two types of growth rotations of the mandible. If the condylar growth is greater than the vertical growth in the molar area, the mandible rotates counter-clockwise resulting in more horizontal change of the chin and less increase in anterior face height. Conversely, if vertical growth at the molar area is greater than at the condyles, the mandible rotates clockwise resulting in increased anterior face height and less horizontal change of the chin. Clockwise rotators are supposed to exhibit an unfavorable reaction to functional therapy due to a posterior mandibular rotation.[19]
The purpose of this study was to determine the skeletal, dentoalveolar and soft tissue changes in children with different jaw base rotations treated with either the twin block appliance or the activator for the treatment of Class II Division 1 malocclusion.
MATERIALS AND METHODS
The sample consisted of the patients who were already treated in the Department. Individual standardized lateral cephalograms of 32 patients (18 boys and 14 girls) taken from the X-Trophy Cephalostat manufactured by Kodak were selected. All the cephalometric radiographs were with the teeth in occlusion.
The inclusion criteria were as follows:
Age group was between 11 and 14 years
The subjects were treated with a mandibular protrusive appliance (twin block or activator) for the treatment of Class II Division 1 malocclusion.(8-10 h for the activator patient, 14-16 h for the twin block patients, per day)
The mean duration of the protrusive appliance treatment was 1 year
Inter-occlusal acrylic trimming was performed in a low angle patients to allow unhindered vertical development of the mandibular buccal segments
No adjunctive orthodontic treatment either prior to or during the period of functional treatment.
The subjects were divided into two groups:
A high angle group (n = 16) with frankfort mandibular plane angle (FMA) >27° and
A low angle group (n = 16) with FMA < 20°.
Cephalograms taken at T1 (pretreatment) and T2 (after 1 year of wearing myofunctional appliance) for all subjects in both the groups were collected. These cephalograms were traced manually and analyzed on the basis of various landmarks chosen to determine the skeletal, dentoalveolar and soft tissue changes in both the groups. The identification of these landmarks was based on the definition by Riolo et al.[24] A vertical reference plane (VRP) through the sella at 97° to the sella–nasion (SN) plane was constructed [Figure 1]. Forty-two angular, linear, and proportional measurements were recorded. The measurements were verified by two authors, and the mean was considered. The data collected were subjected to statistical analysis.
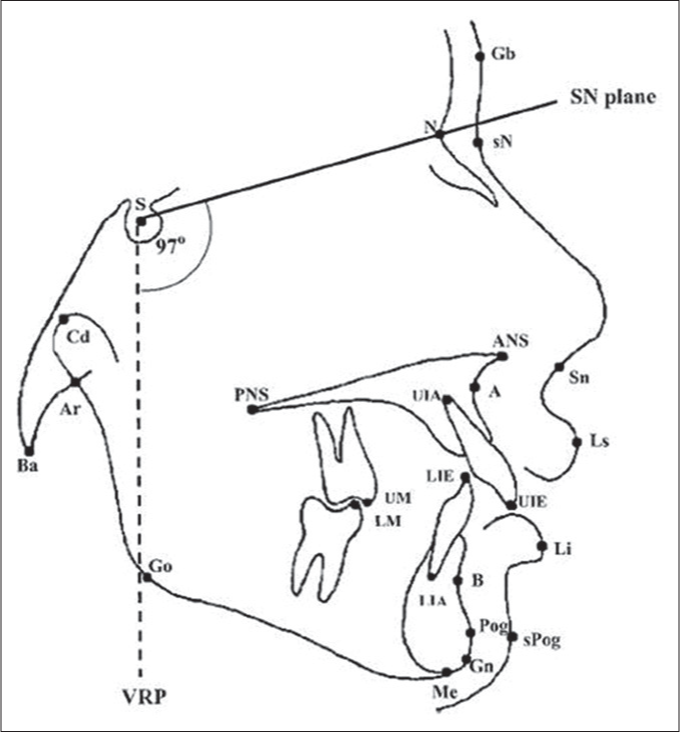
- A vertical reference plane through the sella at 97° to the sella–nasion plane
Statistical method
A master file was created, and the data were statistically analyzed on a computer using the Statistical Package for the Social Sciences software (Chicago, Ill, USA).The data were subjected to paired t-test. P <0.005 was considered as statistically significant.
RESULTS
The results are presented in tabular form. The mean ages and length of treatment for both groups were similar.
Cranial base variables
At the end of treatment, there was no increase in lateral cranial base length (S-Ar) and the anterior cranial base length (S-N) in both the high and low angle groups. The total cranial base length (Ba-N) was decreased in both the groups. The saddle angle (N-S-Ar) reduced in both the groups. None of these changes were statistically significant [Table 1].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At prereatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| S-Ar (mm) | 37.6 | 4.1 | 37.7 | 4.6 | 0.164 | 36.3 | 3.7 | 36.8 | 3.5 | 0.500 |
| S-N (mm) | 70.5 | 2.1 | 71.5 | 2.5 | 0.822 | 71.6 | 3.9 | 72.12 | 4.2 | 0.340 |
| Ba-N (mm) | 111.2 | 5.8 | 109.7 | 5.4 | 0.164 | 110.6 | 3.8 | 109.5 | 5.4 | 0.425 |
| N-S-Ar (°) | 125.8 | 7.2 | 125.3 | 5.6 | 0.698 | 126.3 | 5.1 | 123.8 | 5.4 | 0.028 |
SD - Standard deviation
Face height variables
The upper anterior face height increased only in the high angle group. The lower anterior face height (LAFH) increased in both groups but showed statistically significant increase in the low angle group only. The upper posterior face height and the lower posterior face height (LPFH) increased in both the groups. The LAFH % was increased in the low angle group but decreased in the high angle group. The LPFH % was decreased in both the groups. The articular angle (S-Ar-Go) decreased in the low angle group but increased in the high angle group [Table 2].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| UAFH (mm) | 51.4 | 3.6 | 51.3 | 3.2 | 0.873 | 50.7 | 3.1 | 51.8 | 3.1 | 0.107 |
| LAFH (mm) | 61 | 5.3 | 63.7 | 4.7 | 0.001* | 69 | 4.7 | 70.5 | 5.5 | 0.071 |
| UPFH (mm) | 47.5 | 2.6 | 49.3 | 3.3 | 0.014 | 49.6 | 3.1 | 50.3 | 3.6 | 0.312 |
| LPFH (mm) | 40.9 | 4.4 | 41.7 | 4.3 | 0.487 | 41.5 | 3.6 | 42.2 | 4.1 | 0.397 |
| %LAFH | 51.7 | 5.4 | 55.6 | 2.8 | 0.036 | 58 | 4.9 | 57.8 | 4.1 | 0.783 |
| %LPFH | 37.3 | 7.3 | 36.8 | 3.7 | 0.780 | 35.6 | 3.6 | 34.8 | 2.7 | 0.350 |
| S-Ar-Go (°) | 137.1 | 6.7 | 136.2 | 6.5 | 0.444 | 138.7 | 5.9 | 139.7 | 8.7 | 0.669 |
*P<0.005. SD - Standard deviation; UAFH - Upper anterior face height; LAFH - Lower anterior face height; UPFH - Upper posterior face height; LPFH - Lower posterior face height
Antero-posterior variables
The SNA angle remained the same in both groups. The SNB angle showed statistically significant increase in both the groups. The ANB angle reduced in both the groups but not significantly. The horizontal linear distance from the reference plane to condylion (VRP-Cd) decreased in the high angle group only. The horizontal linear distance from the reference plane to anterior nasal spine (VRP-ANS) and point A (VRP-A) remained the same in both the groups. The horizontal linear distance from the reference plane to point B (VRP-B) increased in both the groups but significantly only in the high angle group. The horizontal linear distance from the reference plane to pogonion (VRP-Pog) significantly increased in both the groups. The angle (S-N-Pog) increased in both groups but showed statistically significant increase in the high angle group [Table 3].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| SNA (°) | 82.2 | 3.9 | 82.6 | 3.5 | 0.643 | 82.9 | 3.5 | 82.6 | 3.7 | 0.732 |
| SNB (°) | 76.3 | 3.9 | 78.3 | 3.9 | 0.004* | 75.1 | 2.7 | 77.1 | 3.4 | 0.001* |
| ANB (°) | 6.4 | 10.3 | 5.9 | 1.7 | 0.643 | 9.1 | 15.7 | 7.7 | 2.8 | 0.745 |
| VRP-Cd (mm) | 15.8 | 3.8 | 15.2 | 3.6 | 0.542 | 15 | 3.8 | 14.1 | 3.3 | 0.456 |
| VRP-ANS (mm) | 76 | 4.8 | 76.1 | 4.5 | 0.947 | 77.6 | 6.1 | 77.8 | 5.5 | 0.744 |
| VRP-A (mm) | 68.8 | 4.5 | 68.9 | 7.1 | 0.968 | 71.5 | 5.2 | 71.1 | 5.9 | 0.548 |
| VRP-B (mm) | 60.5 | 6.4 | 63.2 | 7.6 | 0.024 | 58.1 | 6.8 | 61.6 | 7.2 | 0.004* |
| VRP-Pog (mm) | 61.6 | 6.2 | 64.9 | 8.2 | 0.004* | 58.1 | 6.8 | 61.6 | 7.2 | 0.000* |
| SN-Pog (°) | 78.2 | 3.6 | 79.1 | 3.8 | 0.140 | 75.6 | 2.6 | 77.6 | 3.4 | 0.001* |
*P<0.005. SD - Standard deviation; SN - Sella-nasion; VRP - Vertical reference plane; Cd - Condylion; ANS - Anterior nasal spine; Pog - Pogonion
Horizontal variables
The angles S-N-maxillary plane (S-N-MxP) and S-N-mandibular plane (S-N-MnP) increased in both the groups but were not significant. The basal plane angle (MxP-MnP) increased in the low angle group but decreased in the high angle group but the change was not significant [Table 4].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| SN-MxP (°) | 5.8 | 3.2 | 6.4 | 3.7 | 0.533 | 5 | 2.2 | 6.1 | 3.4 | 0.205 |
| SN-MnP (°) | 27.2 | 5.1 | 28.3 | 6.9 | 0.393 | 34.6 | 5.7 | 35.3 | 5.4 | 0.374 |
| MxP-MnP (°) | 21 | 4 | 23.4 | 5.9 | 0.035 | 29.5 | 3.1 | 28.8 | 4.8 | 0.651 |
SD - Standard deviation; SN - Sella-nasion; MxP - Maxillary plane; MnP - Mandibular plane
Mandibular variables
The ascending ramus length (Cd-Go) and the corpus length (Go-Gn) increased in both the groups but were not significant. The total mandibular length (Cd-Gn) reading was the same in the low angle group but increased in the high angle group. The linear distance from articulare to gnathion (Ar-Gn) and articulare to gonion (Ar-Go) decreased in both the groups. The gonial angle (Ar-Go-Me) showed an increase in both the groups [Table 5]. in the high angle group. The linear distance of the upper molar from the MxP (UM-MxP) and the lower molar from the MnP (LM-MnP) also showed statistically significant increase in both the groups. The linear distance of the upper molar (VRP-UM) from the vertical reference line also showed an increase but not significantly in both groups. The linear distance of the lower molar from the vertical reference plane (VRP-LM) also showed statistically significant increase in both the groups [Table 6].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| CD-Go (mm) | 54.3 | 4.3 | 56.1 | 5.7 | 0.169 | 52.6 | 7.3 | 54.6 | 3.3 | 0.290 |
| CD-Gn (mm) | 108.3 | 6.1 | 108.7 | 11.8 | 0.891 | 108.6 | 14.6 | 110.1 | 11.6 | 0.762 |
| Go-Gn (mm) | 66.6 | 5.6 | 71.3 | 12.8 | 0.172 | 70.68 | 10.5 | 73.4 | 12.1 | 0.468 |
| Ar-Gn (mm) | 166.5 | 2.5 | 105.2 | 6.1 | 0.345 | 106.2 | 8.2 | 105.3 | 5.8 | 0.599 |
| Ar-Go-Me (°) | 127 | 4.9 | 130 | 5.2 | 0.542 | 130 | 6.7 | 133.6 | 7.1 | 0.142 |
SD - Standard deviation
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| OJ | 10.7 | 2.6 | 5.7 | 1.9 | 0.0001* | 9.7 | 3.1 | 5.3 | 2.3 | 0.000* |
| UI-MxP (°) | 124.1 | 5.8 | 117.9 | 7.5 | 0.0004* | 120.5 | 6.7 | 113.9 | 5.9 | 0.000* |
| LI-MnP (°) | 104.3 | 6.1 | 102.4 | 6.4 | 0.369 | 101.8 | 6.4 | 102.3 | 8.3 | 0.006* |
| II (°) | 108.6 | 7.4 | 114 | 9.5 | 0.048 | 106.2 | 7.5 | 111.9 | 8.8 | 0.003* |
| UM-MxP (mm) | 19.4 | 2.1 | 20 | 1.5 | 0.326 | 20.3 | 1.9 | 21.9 | 2.5 | 0.000* |
| LM-MnP (mm) | 28.1 | 3 | 30.1 | 2.6 | 0.006* | 30.8 | 2.7 | 32.7 | 2.3 | 0.001* |
| VRP-UM (mm) | 40.1 | 5.5 | 41.1 | 5.6 | 0.101 | 41.8 | 5.6 | 42.4 | 5.7 | 0.333 |
| VRP-LM (mm) | 39.4 | 5.7 | 44.1 | 5.5 | 0.000* | 40.7 | 5.6 | 44.2 | 5.8 | 0.000* |
*P<0.005. SD - Standard deviation; VRP - Vertical reference plane; LM - Lower molar; UM - Upper molar; MxP - Maxillary plane; MnP - Mandibular plane; LI - Lower incisor; UI - Upper incisor; OJ - Overjet
Dentoalveolar variables
The overjet showed statistically significant decrease in both the groups. The upper incisor inclination (UI-MxP) showed statistically significant decrease in both the groups. The mandibular incisor inclination (LI-MnP) and inter-incisal angle showed statistically significant increase
Soft tissue variables
Perpendicular linear distances from the VRP to soft tissue nasion and VRP-labi-superioris increased in both the groups but were not significant. Perpendicular linear distances from the VRP to glabella remained the same in both the groups. Perpendicular linear distances from the VRP to subnasale increased in the high angle group but perpendicular linear distances from the VRP to labii-inferioris showed statistically significant increase in the low angle group. Perpendicular linear distances from the VRP-Pog significantly increased in both the groups [Table 7].
| Low angle group | High angle group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | At pretreatment (T1) | After 1-year of wearing appliance (T2) | P | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| VRP-Gb (mm) | 78.7 | 3.2 | 78.8 | 3.6 | 0.831 | 79.8 | 3.9 | 80.1 | 5.4 | 0.794 |
| VRP-SN (mm) | 76.6 | 2.8 | 77 | 3.2 | 0.573 | 76.7 | 5.6 | 77.6 | 5.3 | 0.425 |
| VRP-SN (mm) | 93.8 | 9.1 | 95.4 | 6.7 | 0.248 | 93.6 | 9.3 | 93.7 | 6.9 | 0.962 |
| VRP-Ls (mm) | 90.1 | 5.4 | 91.1 | 6.1 | 0.119 | 90.7 | 8 | 90.6 | 7.9 | 0.881 |
| VRP-Li (mm) | 82.3 | 5.7 | 86.1 | 7.8 | 0.003* | 83.1 | 8.7 | 85.5 | 8.1 | 0.054 |
| VRP-Pog (mm) | 72.2 | 8.5 | 76.1 | 8.5 | 0.007* | 70.6 | 7.9 | 74.1 | 7.6 | 0.004* |
*P<0.005. SD - Standard deviation; VRP - Vertical reference plane; SN - Sella-nasion; Pog - Pogonion
DISCUSSION
The discrepancy between the jaws in the development of the stomato-gnathic system plays an important role in the development of Angles Class II Division 1 malocclusions. After 3.8 years of study on a lot of 23 Class II untreated patients, Baccetti et al.[25] have reported that under the influence of normal growth, the length of the mandible is changing with 0-1.2 mm. A previous study, 14.5 months long, on Brazilian Class II untreated subjects of Gomes and Lima,[26] has reported an annual growth rate of 2.16 mm for the horizontal ramus, 3.16 mm for the vertical ramus and 4.31 mm for the total mandibular length.
McNamara (1981)[27] studied the components of Class II malocclusion in children and 8-10 years of age and revealed that the majority have a component of mandibular deficiency. Changing the function of the mandible by inducing the patient to function with the lower jaw placed forward could stimulate mandibular growth thereby correcting a Class II problem. It has been established that functional appliances play a significant role in the correction of sagittal and vertical malrelationship (Schmuth 1983).[6] The change in maxillo-mandibular relationship after forward alteration of the mandibular position results from an interrelated series of changes in several regions within the craniofacial complex (Elgoyhen et al. 1972).[28] Mamandras and Allen (1990)[29] suggested that the persons who have small mandibles may benefit from functional appliance therapy than patients with normal-sized mandibles. This study was conducted to determine the skeletal, dentoalveolar and soft tissue changes in children with different jaw rotations treated with either the twin block appliance or the activator for the treatment of Class II Division 1 malocclusion.
All 32 patients selected for this study had undergone functional appliance therapy for correction of a Class II Division I incisor relationship. The subjects were divided into two groups as high angle group (n = 16) with FMA >27° and a low angle group (n = 16) with FMA <20°. The statistically significant changes were seen with the SNB angle and the linear distance from the VRP-Pog in both the high and low angle groups suggesting favorable response to myofunctional appliances by posturing the mandible forward. There was an increase in the corpus length (Go-Gn) in both the groups but not significantly.
The SNA angle, the horizontal distance from VRP-A and VRP-ANS, remained the same for both the groups, suggesting that the functional appliances had a restraining effect on the maxilla. When the mandible was postured forward by the functional appliances, a reciprocal force acted distally on the maxilla, redirecting growth.[30]
Amongst the dentoalveolar changes, both the groups showed statistically significant reduction in the overjet by retroclination of the upper incisors and proclination of the lower incisors. Mandibular molars significantly moved ahead in relation to the VRP and also showed significant vertical eruption in both the groups. The forward movement of mandibular molars could be attributed to the repositioning of the mandible. The vertical eruption of the molars in the low angle group was because of interocclusal acrylic trimming which was carried out to allow unhindered vertical development of the mandibular buccal segments. As a protocol, all the high angle patients were treated with activator only to restrict further vertical growth. In the high angle group inter-oclussal trimming was not done of the activators, but there was vertical eruption of molars that may have been due to the part-time wear of the activator in the high angle patients. In the upward and forward rotators, that is, in low angle group, these changes are expected, and the literature also supports these findings. But significant findings were also found in the high angle group, which were unexpected. As our study was limited only to a 1 year duration, long-term follow-up of this group is required to further evaluate these findings.
In the low angle group, we found that there is a statistically significant increase in the gonial angle and the LAFH which could be attributed to the upward and mesial movement of the mandibular molars indicating that the horizontal growers showed a favorable response to mandibular advancement by enhancing eruption of posteriors.
In the high angle group, though there was a significant increase in the S-N-Pog and VRP-B, which indicates forward movement of the mandible. This forward movement did not cause a significant increase in the LAFH; that shows that in the high angle group there was a good control on the downward and backward rotation of mandible. In this group, we also found that the lower incisors are significantly proclined because of the forward positioning of the mandible.
Functional appliances have been shown to stimulate bone apposition at the posterior pole of the condyle,[31-34] this therapeutic effects coincides with the inherited condylar growth direction in vertical growers[35] and this could explain the unexpected favorable skeletal changes in high angle group.
CONCLUSION
In this study, it was found that both the high angle and low angle groups responded equally well to the myofunctional therapy, in fact, in the high angle group, we found significant changes in more number of variables including skeletal and dentoalveolar parameters.
LIMITATIONS
Duration of the study was short. This study evaluates the effects of myofunctional appliances after 1 year only, which may not be permanent. So a further study with an increased sample size and followed for a longer time period will greatly improve the authenticity of our results
The amount of sagittal and vertical advancement during bite registration for myofunctional appliances was not taken into consideration.
Acknowledgment
We would like to thank the Dr. Vinit Swami sincerely for his help in sample acquisition. We would also like to thank Mr. Suyog Joshi for the help with the statistical analysis.
References
- The skeletal patterns characteristic of Class I and Class II, Division I malocclusions in norma lateralis. Angle Orthod. 1951;21:44-56.
- [Google Scholar]
- A study of the facial patterns associated with Class I, Class II, Division 1, and Class II, Division 2 malocclusions. Angle Orthod. 1948;18:12-5.
- [Google Scholar]
- Facial morphology and growth from 10 to 14 years of age in children presenting Class II, Division 1 malocclusion: A comparative roentgenographic cephalometric study. Am J Orthod. 1971;60:619-20.
- [Google Scholar]
- Components of class II malocclusion in children 8-10 years of age. Angle Orthod. 1981;51:177-202.
- [Google Scholar]
- Milestones in the development and practical application of functional appliances. Am J Orthod. 1983;84:48-53.
- [Google Scholar]
- A growth-related concept for skeletal class II treatment. Am J Orthod. 1978;74:258-75.
- [Google Scholar]
- Cephalometric evaluation of treatment effect on Class II, Division I malocclusions. Am J Orthod. 1967;53:446-57.
- [Google Scholar]
- Morphological changes of the facial skeleton in Class II/1 patients treated with orthodontic functional appliances. APOS Trends Orthod. 2014;4:126-32.
- [Google Scholar]
- The principle of the Andresen method of orthodontic treatment a discussion based on cephalometric x-ray analysis of treated cases. Am J Orthod. 1951;37:437-58.
- [Google Scholar]
- The effect of activator treatment on class II malocclusions. Am J Orthod. 1979;75:20-6.
- [Google Scholar]
- An assessment of Andresen therapy on class II division 1 malocclusion. Br J Orthod. 1982;9:149-53.
- [Google Scholar]
- A laminographic study of alterations in the temporomandibular joint following activator treatment. Eur J Orthod. 1984;6:257-66.
- [Google Scholar]
- Skeletal profile changes related to two patterns of activator effects. Am J Orthod. 1982;81:390-6.
- [Google Scholar]
- The passive activator: Case selection, treatment response, and corrective mechanics. Am J Orthod. 1978;73:378-409.
- [Google Scholar]
- Response to activator treatment in Class II malocclusions. Am J Orthod. 1985;88:242-51.
- [Google Scholar]
- The bionator In: Graber TM, Newmann B, eds. Removable Orthodontic Appliances. Philadelphia: W. B. Saunders; 1977. p. :229-46.
- [Google Scholar]
- Cephalometric determinants of successful functional appliance therapy. Angle Orthod. 2002;72:410-7.
- [Google Scholar]
- Skeletal and dentoalveolar effects of Twin-block and bionator appliances in the treatment of Class II malocclusion: A comparative study. Am J Orthod Dentofacial Orthop. 2006;130:594-602.
- [Google Scholar]
- The rotation of the mandible resulting from growth: Its implications in orthodontic treatment. Angle Orthod. 1965;35:36-50.
- [Google Scholar]
- An Atlas of Craniofacial Growth. Monograph 2, Craniofacial Growth Series. Mich: University of Michigan Ann Arbor; 1974.
- Dentofacial growth changes in subjects with untreated Class II malocclusion from late puberty through young adulthood. Am J Orthod Dentofacial Orthop. 2009;135:148-54.
- [Google Scholar]
- Functional determinants of craniofacial size and shape. Eur J Orthod. 1980;2:131-59.
- [Google Scholar]
- Craniofacial adaptation of protrusive function in young rhesus monkeys. Am J Orthod. 1972;62:469-80.
- [Google Scholar]
- Mandibular response to orthodontic treatment with the Bionator appliance. Am J Orthod Dentofacial Orthop. 1990;97:113-20.
- [Google Scholar]
- Application and appliance manipulation of functional forces. Am J Orthod. 1970;58:459-78.
- [Google Scholar]
- Orthodontics: Current Principles and Techniques. Vol 81. C.V. Mosby Co.; 1985. p. :408.
- Neuromuscular and skeletal adaptations to altered function in the orofacial region. Am J Orthod. 1973;64:578-606.
- [Google Scholar]
- Long-term mandibular adaptations to protrusive function: An experimental study in Macaca mulatta. Am J Orthod Dentofacial Orthop. 1987;92:98-108.
- [Google Scholar]
- The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop. 1987;92:181-98.
- [Google Scholar]






