Translate this page into:
Orthodontic Finishing: Ten Steps to Success*
Address for correspondence: Prof. Jose Nelson Mucha, Rua Jornalista Henrique Cordeiro 400/1606, Barra da Tijuca, Rio de Janeiro 22631-450, Brazil. E-mail: muchanelson@yahoo.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
An excellent orthodontic finishing is essential and involves a series of procedures such as a good diagnosis, appropriate treatment plan, and implementing the treatment plan. However, the most critical phase corresponds to finish properly or closely to the appliance removal. It is not enough only to say that it was a good finish. Specifically why, or what details are needed to be observed and obtained, and in what order to conclude that a great orthodontic finishing was done. In this article, I intend to discuss and propose procedures considered indispensable for the excellence in orthodontic finish. The goals are results with excellent oral health; facial, dental and smile harmony; functional occlusion; and especially long-term stability. In this matter, it is important to follow a series of procedures that can be summarized in 10 steps: (1) define clearly your goals; (2) have a checklist; (3) improve bracket placement; (4) repositioning of brackets; (5) make adjustments in the archwires; (6) look at the face, teeth and smile, not the appliance; (7) improve the functional occlusion; (8) reshape teeth anatomically; (9) plan the retention; and (10) plan the appliance removal. The conclusions are that following this steps and keeping in mind that in clinical orthodontic practice is necessary to clearly define the objectives, to know the basic and have technical domain; the result will be inevitable: Success.
Keywords
Evaluation of the results
excellence in orthodontics
treatment finishing
Introduction
Near the time of orthodontic appliance removing or at the end of the orthodontic treatment, certain aspects need to be observed. It is not enough just to conclude that a great treatment has been performed; however, the most important question to ask at this moment is: Why an excellent treatment was carried out? Or not!
More precisely, at this crucial stage of treatment, it will be necessary to observe certain details to have the definition that a good treatment has really been performed. The question rise again: Which are the details that should be observed?
In other words, which characteristics should the case present or better yet, what should be the hierarchical order of details to observe to be able to state that the case was in deed well conducted and that we reached ours goals? And what should be ours goals in that specific case? [Figures 1-3].
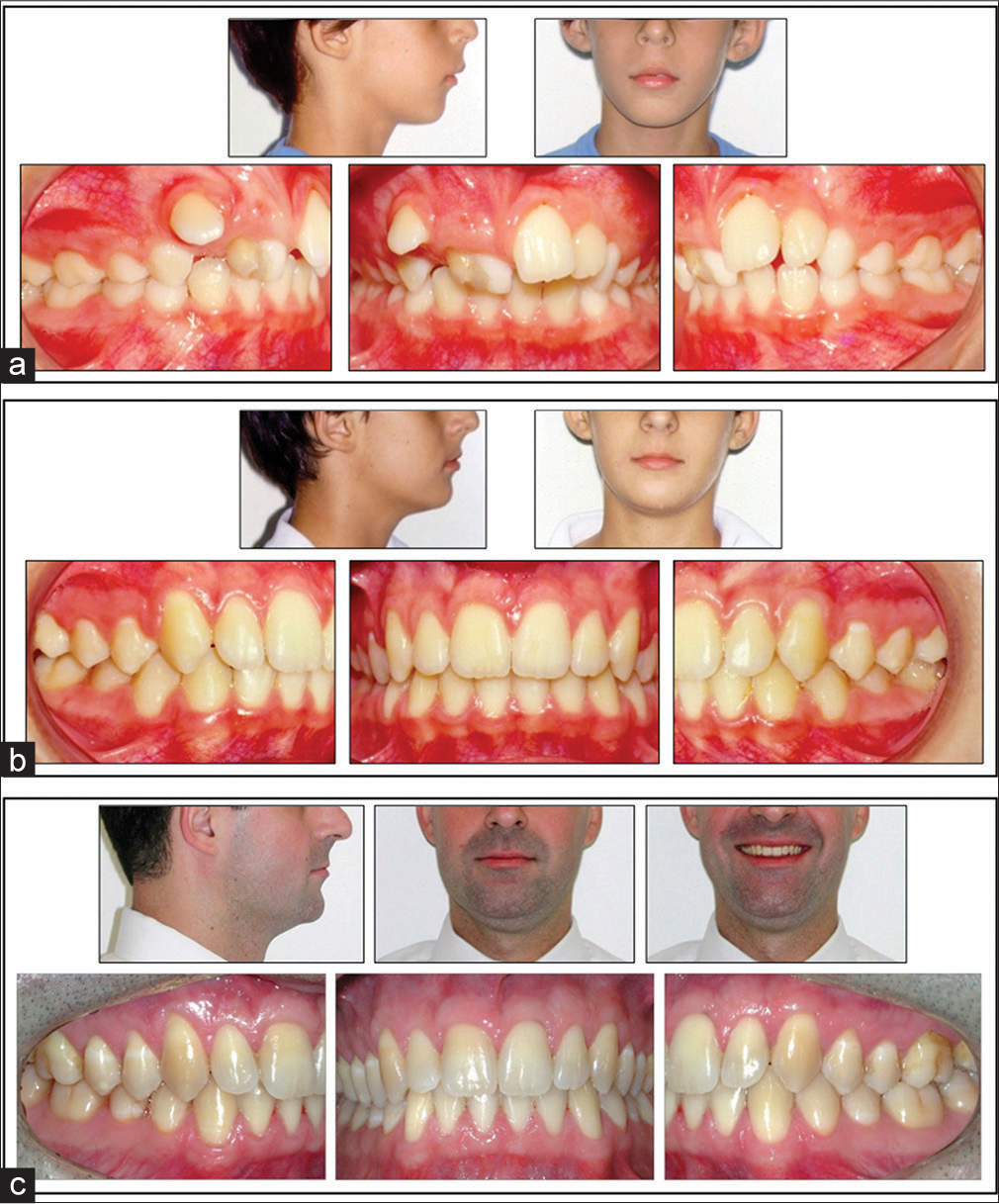
- (a) A Class II patient with a retrognathic profile and increased lower facial third that began treatment in 1987 at 9 years old. (b) Posttreatment at 12 years old in 1990. (c) The patient with 35 years old in 2013, and with 23 years of follow-up
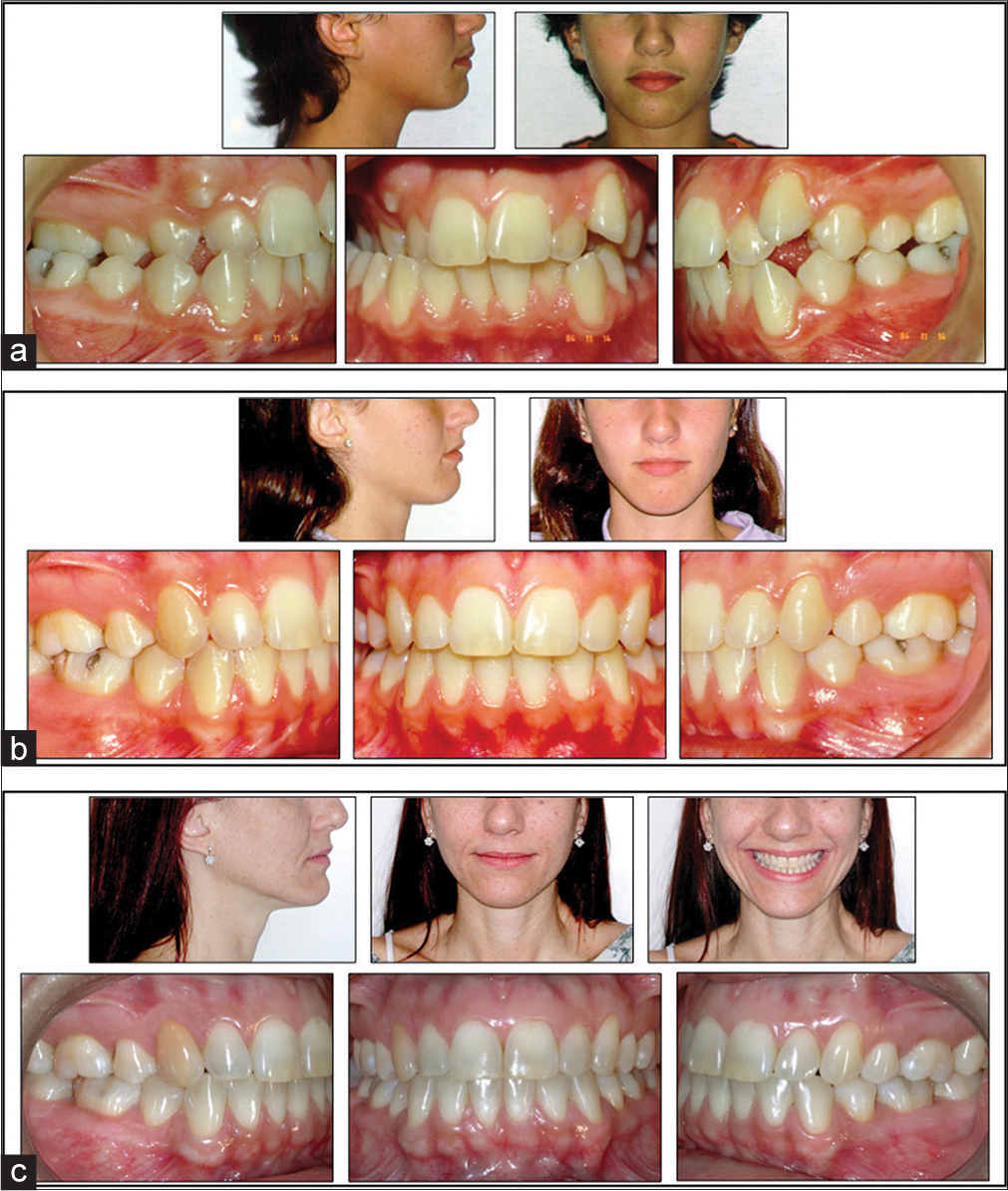
- (a) Patient started treatment at 12 years and 3 months old, in 1984. (b) At the end of orthodontic treatment, patient with 14 years and 9 months in 1987. (c) Patient at 41 years old in 2014, with 27-year follow-up and 23 years out of retention
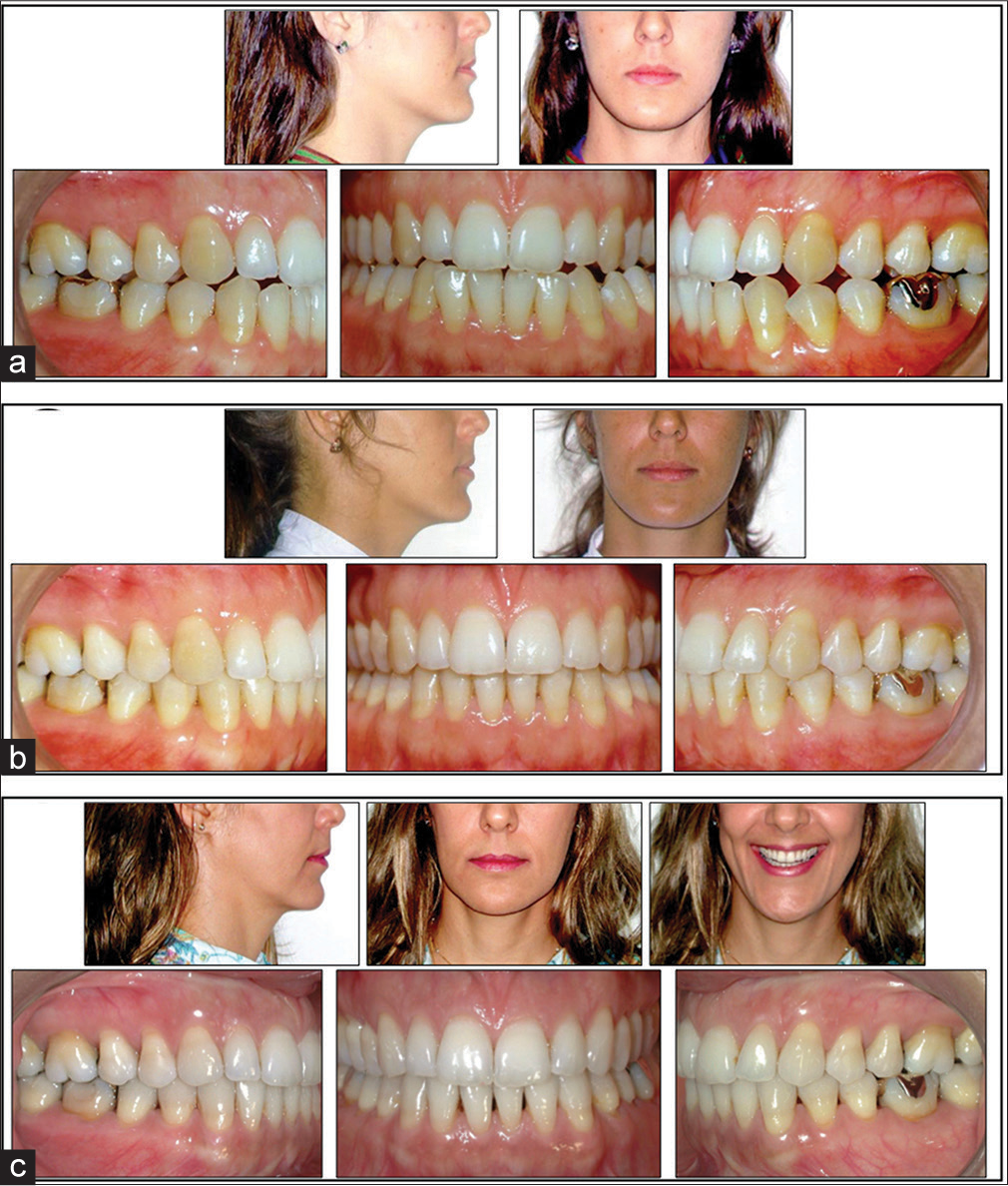
- (a) A Class III adult patient that started treatment at 23 years and 10 months old in 1991. (b) At the end of treatment with 25 years and 11 months in 1993. (c) Patient 46 years old in 2013 and 20-year follow-up
I intend, therefore, to present and to discuss a logical sequence of procedures to obtain an excellent orthodontic finishing treatment. I hope that it may benefit the clinical orthodontists, and especially, the young clinical orthodontists who desires excellent results.
Ten Steps
The ten steps are as follows:
Define your goals
Have a checklist
Improve bracket placement
Repositioning of brackets
Make adjustments in the archwires
Look at the face, teeth and smile, not the appliance
Improve the functional occlusion
Reshape teeth anatomically
Plan the retention
Plan the appliance removal.
Define your goals
In the article, “Common errors observed at the American Board of Orthodontics clinical examination”, Chung et al.[1] conclude that the ABO examiners continue to see problems in cases presentation including lack of attention to finishing details and inappropriate treatment objectives, among other details.
So let’s define our goals in orthodontic treatment:
Oral health
Esthetics
Occlusion
Function
Stability.
Oral health: This means maintainable health of the teeth, the supporting structures, and all the other components of the masticatory system [Figure 4][2]
 Figure 4
Figure 4- Excellent oral health is one of the objectives of the orthodontic treatment. (a) Spot on the buccal surface of the upper central incisor (yellow arrow). (b) During treatment. (c) At the removal of the appliance
Esthetics: Pleasing esthetics of the face, teeth, and especially the smile [Figure 5]
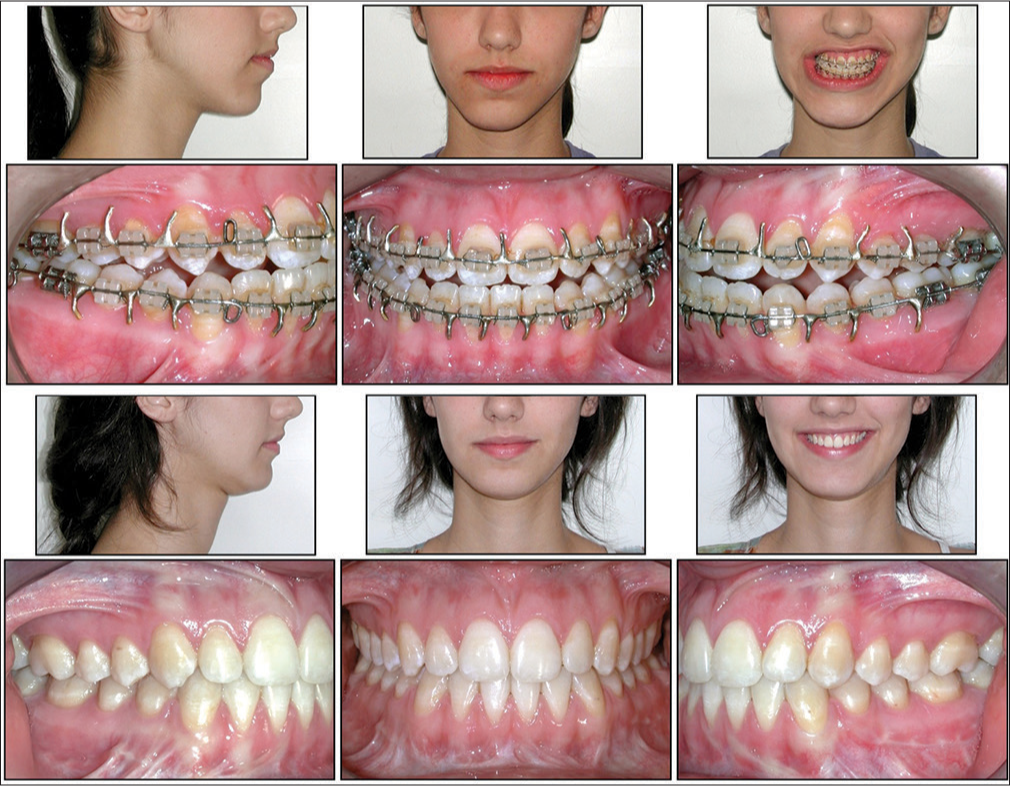 Figure 5
Figure 5- Patient with facial asymmetry being prepared for orthognathic surgery and the outcome of surgical and orthodontic treatment with significant improvement in facial esthetics, occlusion, and dental smile
-
Occlusion: The goal is an anatomic harmony. This means that all the interrelated parts of the masticatory system are in a structural equilibrium. This requires a harmony of form:
Between the teeth and the face-appropriate teeth positions providing an esthetically pleasing face, teeth, and smile
Between the lower teeth and the upper teeth
Between the posterior teeth, the cheeks, and the tongue
Between the anterior teeth, the lips, and the tongue
Between the condyle, the disc, the musculature, and the teeth.[2]
Function: The goal is to obtain a functional harmony. The preferred type of functional occlusion is named “mutually protected occlusion.” The posterior occlusal contacted teeth protect in centric occlusion relation and the anterior teeth protect the eccentric occlusion (anterior guidance), without interference of the posterior teeth in the mandibular movement. For this, it is necessary that this dentition is in a neutral zone between the tongue and the perioral muscles [Figure 6][3]
 Figure 6
Figure 6- (a) Class II malocclusion; (b) The result of treatment with stable contacts in CR. (c) Anterior guidance. Disocclusion of the posterior teeth in protrusive movements. (d and e) Canines guidance in lateral movements
Stability: If each tooth remains without mobility, it does not wear excessively and stays in its proper position, the occlusion can be considered stable. The signs of instability are clinically recognizable as follows: hypermobility; excessive wear; and migration or relapse [Figure 7].[2]
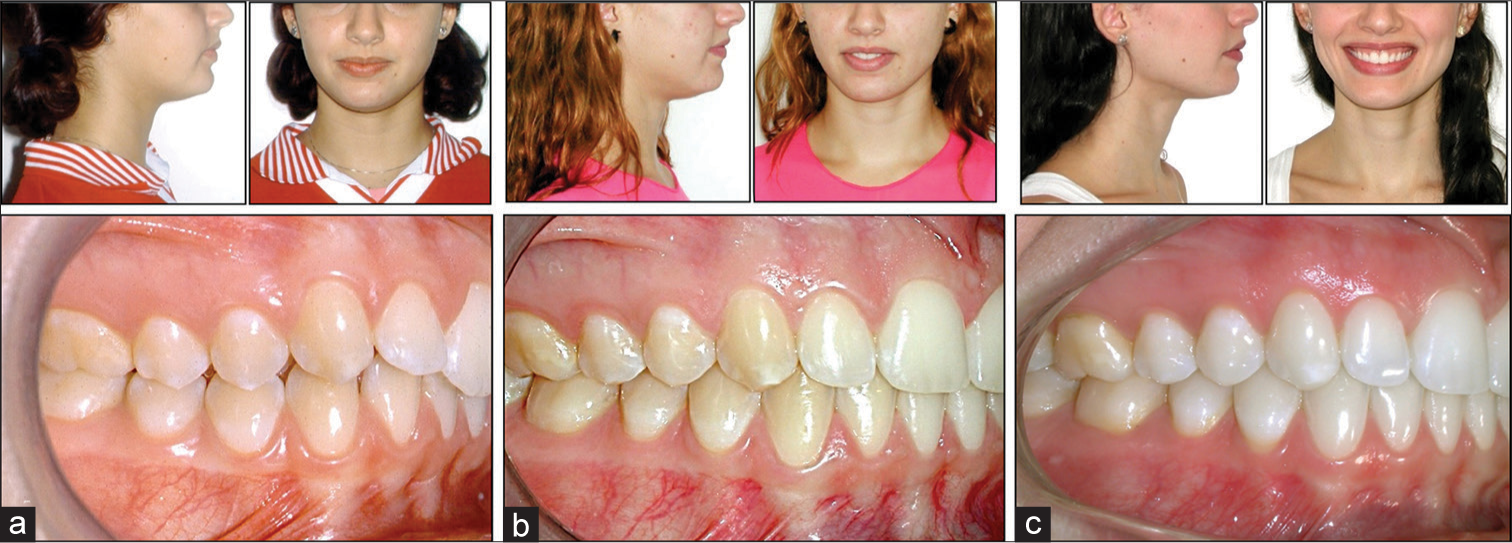 Figure 7
Figure 7- (a) Before treatment, patient age 15 years and 11 months. (b) At the end of treatment, at age 17 years and 11 months. (c) A patient with 28 years and 10 months and 11 years and 10 months follow-up with very stable results
Have a checklist
It is recommended to use a checklist, especially to all whom are starting in clinic orthodontics. This checklist [Figure 8] consists of a hierarchical sequence of seven major items:
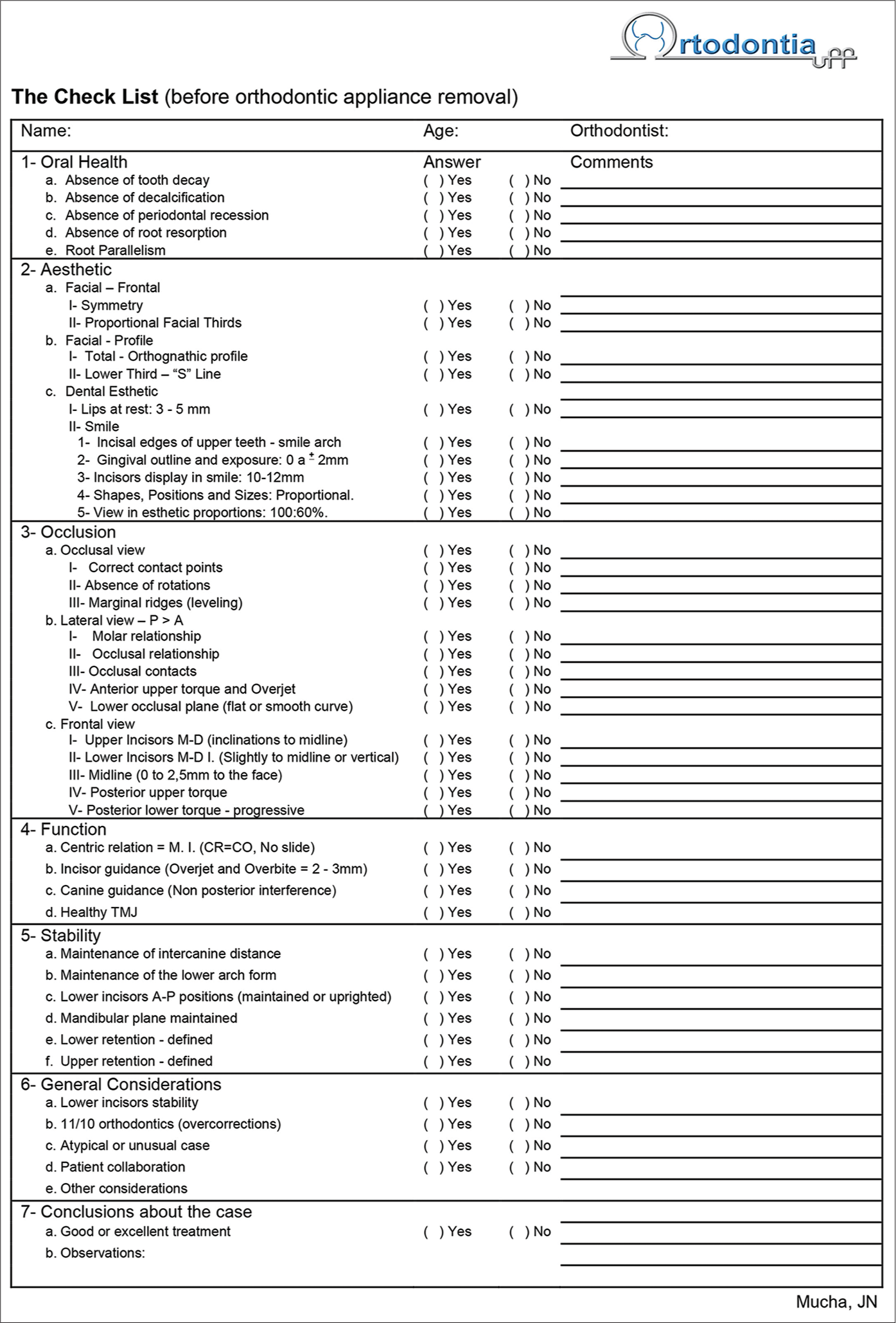
- A checklist
Oral health
Esthetics
Occlusion
Function
Stability
General considerations about the treatment and
Conclusions about the case.
-
Oral health: It is intended with the treatment to prevent or avoid: (a) Tooth decay; (b) decalcification; (c) periodontal resection; (d) root resorption and (e) good root parallelism.
Even though some items may be considered as being irreversible – such as those related to oral health-like decalcification and root resorption – observation and registration of them serve as a reminder of the specific situation in that case and work as a feedback to avoid future-related problems.
-
Esthetics:
-
Face-frontal
Symmetry: The assessment of the patient’s face at the end of the treatment should display an unnoticeable asymmetry. In reality, we are all somewhat slightly asymmetrical. Yet when this asymmetry becomes evident, it remains a great challenge, both for orthodontists and for maxillofacial surgeons, since only skilled surgeons will be able to adequately solve the problem
Vertical proportions: Like the symmetry, the vertical proportions of the face should deserve special attention both in the diagnosis, treatment, and in the evaluation at the end of the treatment. The vertical relationships are related to the middle third of the face, from the eyebrows (G) to the base of the nose (Sn), relative to the lower third of the face, and from the base of the nose (Sn) to the lower edge of the mandible (Me). Thisratio should be close to 1:1. While on women, it may be slightly decreased, giving them a younger appearance. When this lower third is excessively enlarged, the best solution is surgery [Figure 9]
 Figure 9
Figure 9- Lower third is excessively enlarged and the best solution was surgery
Face-Profile (This item will be discussed in step 6 of this article-Look at the face, teeth and smile, not the appliance)
Esthetic: Dental Esthetic (This item will be discussed in step 6 of this article).
-
Occlusion (This item will be discussed in step 6 of this article).
Function (This item will be discussed in step 7 of this article -7. Improve the functional occlusion).
-
Stability:
Maintain lower 3-3 distance [Figure 10a-c]
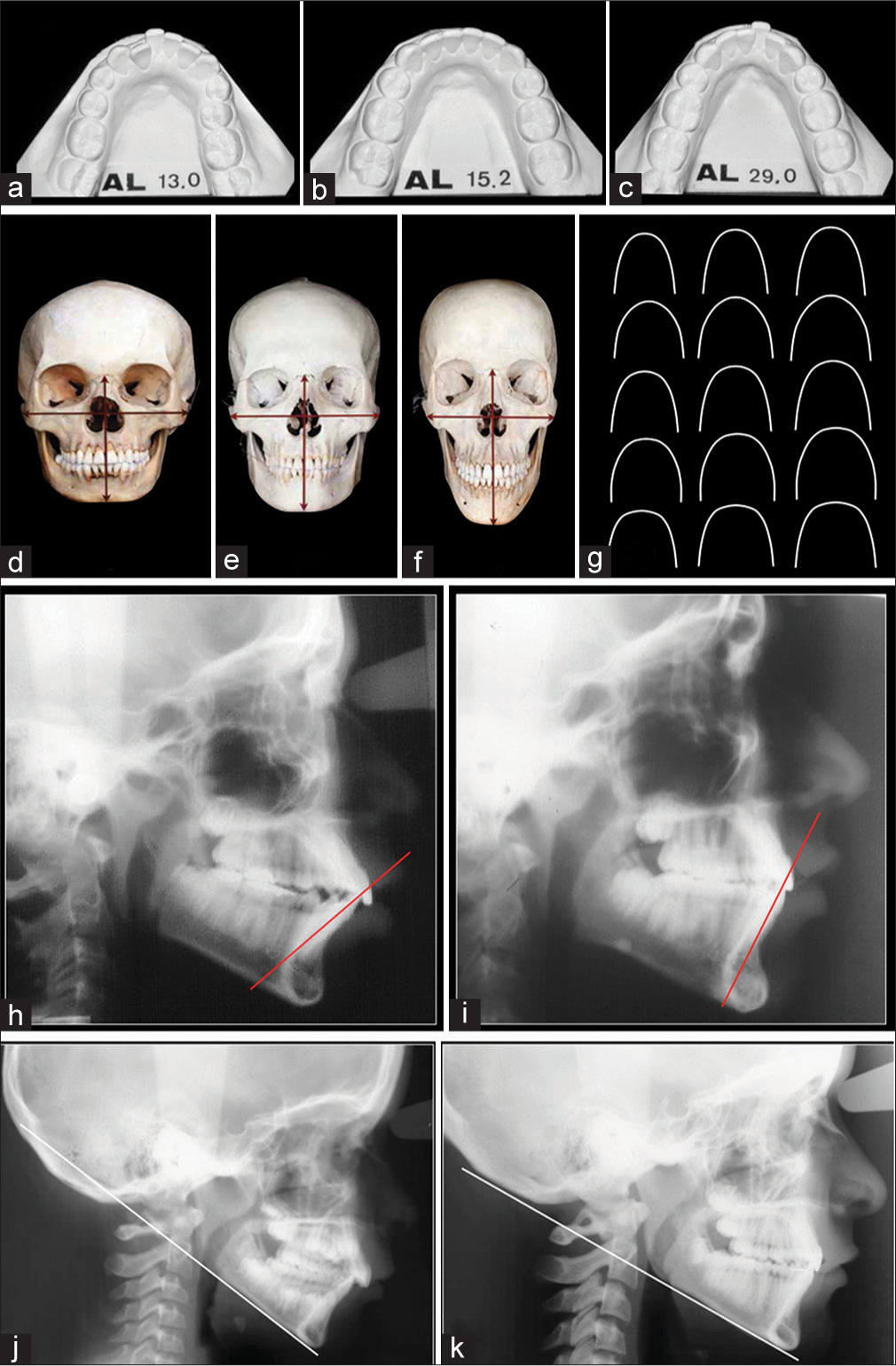 Figure 10
Figure 10- Increase in intercanine distance, even with extractions of premolars, resulted in relapse. (a) Before treatment. (b) At the end of treatment. (c) Relapses 14 years later. (d-g) Different individuals have different skull forms and consequently different shapes and sizes of dental arches. (h and i) The objectives are to maintain lower incisors positions or upright them. (j and k) Maintain mandibular plane angle – or even to reduce in Class II cases
Maintain lower arch form [Figures 10d-g]
Lower incisors-maintain or upright [Figure 10h and i]
Maintain mandibular plane angle– or even to reduce in Class II cases [Figure 10j and k]
Lower retention. Plan the lower retention (more details on step 9)
Upper retention. Plan the upper retention (more details on step 9).
-
General considerations about the treatment: Each case has its peculiarities and problems that can be found during the treatment; however, some details deserve special attention. Among them we have:
Lower incisors stability: In cases of poor patient collaboration, it may have been necessary to make some compromises to reach the end of treatment as the use of intermaxillary elastics and as a result the proclination of the lower incisors. These observations are then recorded in the form
11/10 Ortho: Overcorrections: The overcorrection of some problems are within the characteristics of an excellent orthodontic finalization, such as lower bicuspid giroversion in more 1/10 tenth, not reaching a result of 9/10, neither 10/10 but 11/10
Atypical or unusual case: These data will then be noted on the evaluation sheet
Patient cooperation: This information deserves registration so that in new cases these situations are weighted so that success can be more precisely predicted
Other considerations: These are information that was not contemplated during the all evaluation and due to their importance, deserve mention, and adequate registration.
-
Conclusions about the case. This conclusion can be:
Excellent treatment
Good treatment
Notes (register for when an excellent finishing was not obtained).
Improve bracket placement
There can be advantages in mounting the orthodontic-fixed appliance to assist in the correction of certain specific problems. Some areas are more critical and can be listed as: upper second molars; (b) lower first premolars; (c) upper second premolars and first molars; (d) third molars and; (e) according to malocclusion.
-
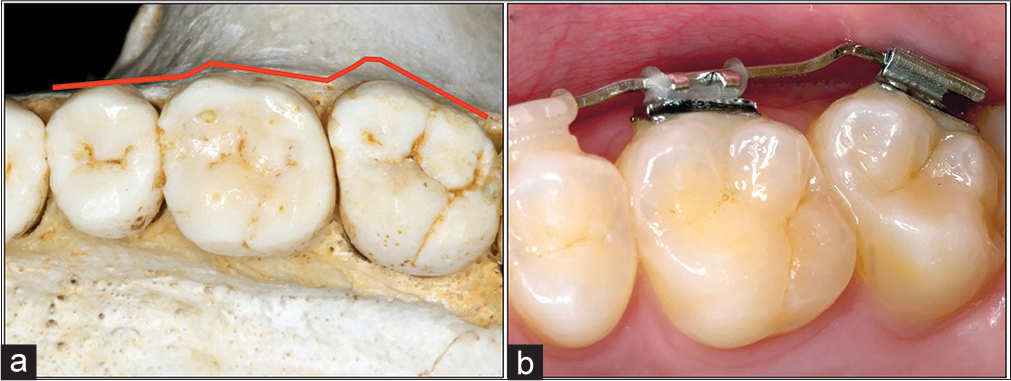
Upper second molars: Usually, a step between first and second molar occurs [Figure 11]. To avoid this step, it is important to understand how these teeth are in a normal situation. By analyzing the position and inclination of the second molars in a collection of skulls with normal occlusion, it is found that these teeth are in a more distocervical direction to the occlusal plane and at a slight angle to distal [Figure 12]
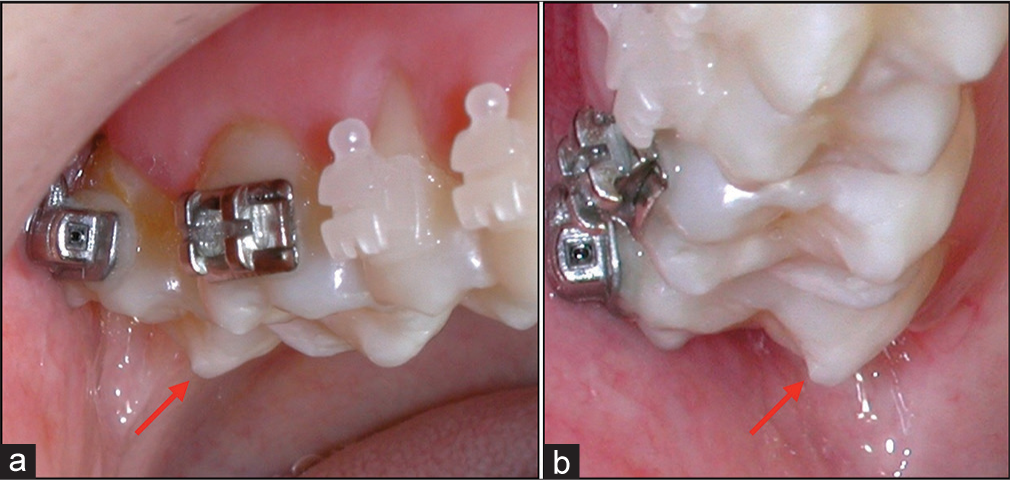 Figure 11
Figure 11- (a and b) An undesirable step between the first and second upper molar
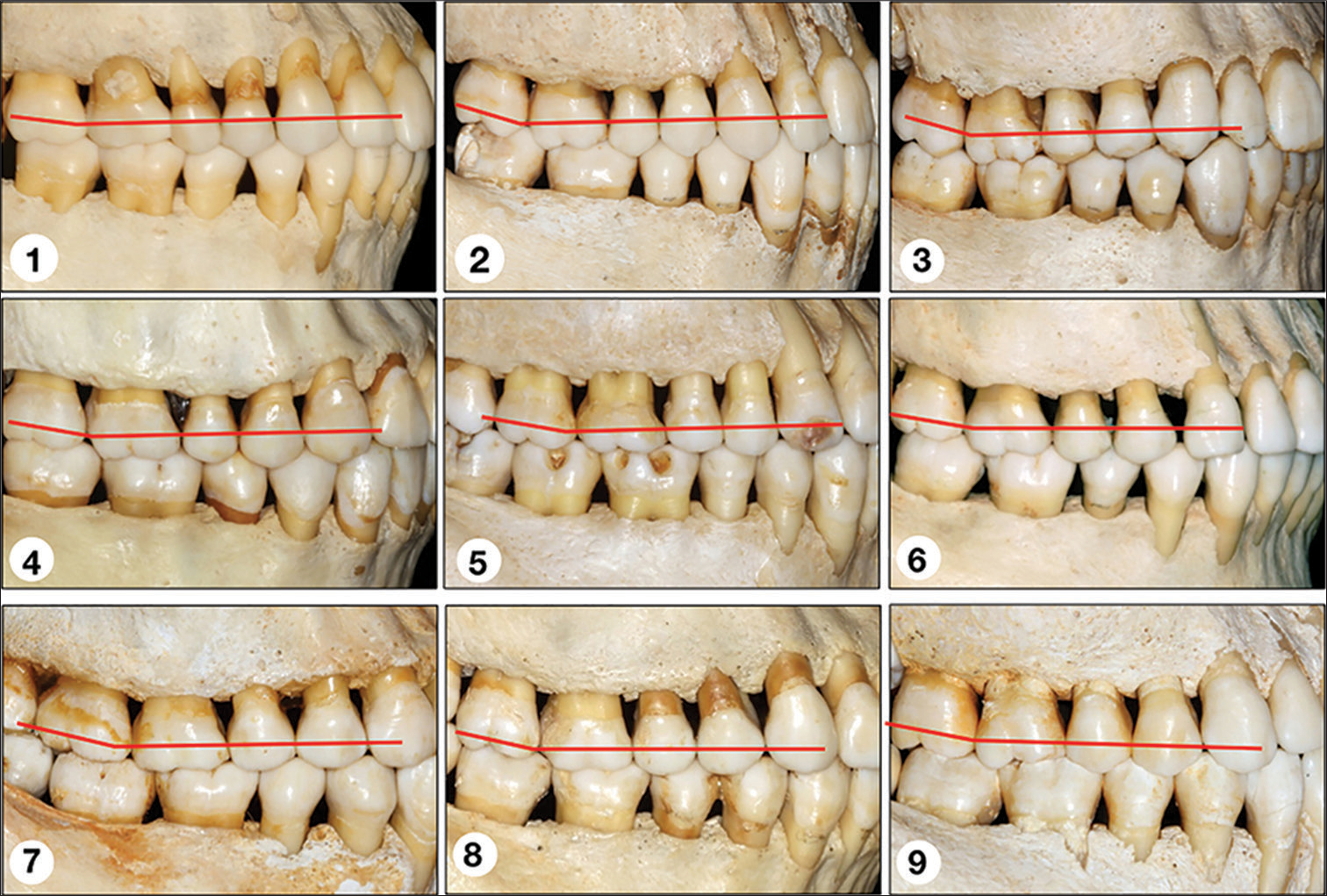 Figure 12
Figure 12- Observe the position of the second molars in a collection of skulls with normal occlusion. These teeth are in a more superior position to the occlusal plane and at a slight angle to the distal
It seems that the position of these teeth is a little different from what is common to mount orthodontic appliances. Therefore, the clinical crowns of the second molars are always angulated in distocervical direction[4] One can observe the same situation illustrated in Angle’s book, as a normal occlusion [Figure 13][5]
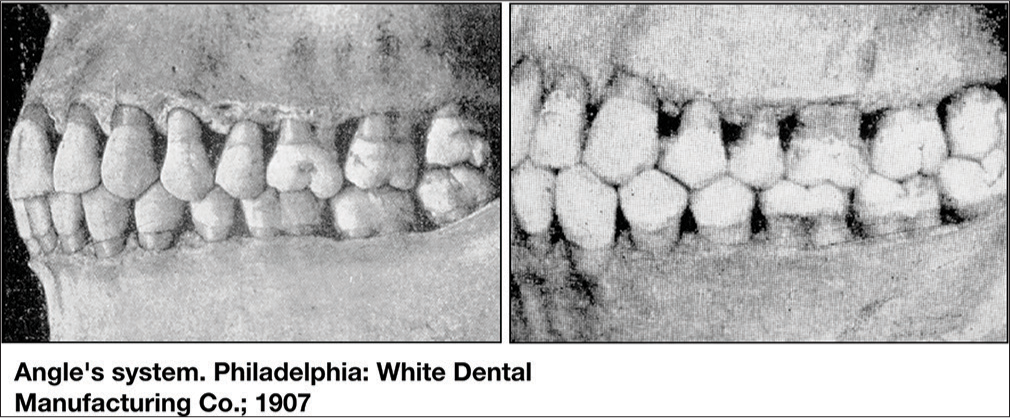 Figure 13
Figure 13- Normal occlusion illustrations from the Angle’s book (1907). The same characteristic position of second molars can be observed
Klontz[6] also emphasizes this condition in a very clear way in his article– “Readout.” Thus, to have no problems in positioning the brackets and tubes on upper second molars, it is necessary to follow the precepts: (1) hold tooth in its normal position, (2) position the bracket as occlusal as possible, and (3) control torque
Lower first premolar: A very common situation is found in Class II malocclusion with severe overbite cases. It is not simply a sharp Curve of Spee, but commonly, there is a step between canine and first premolar [Figure 14]. If the goal is an excellent intercuspidation between these teeth [Figure 15], the solution is to place the first premolar bracket slightly cervical in deep bite cases. This is a technical approach to improve the occlusal contacts in this area and avoid remakes or bending in the arches. In a clinical case where the first premolar was mounted, with the bracket most cervical than the canine, it was possible to get an excellent intercuspidation in this area [Figure 16]
 Figure 14
Figure 14- (a and b) Class II malocclusion with severe overbite. (c and d) It is not simply a sharp Curve of Spee, but commonly, there is a step between canine and first premolar
 Figure 15
Figure 15- (a and b) If the goal is an excellent intercuspidation between these teeth, (c) The solution is to place the first premolar bracket slightly cervical
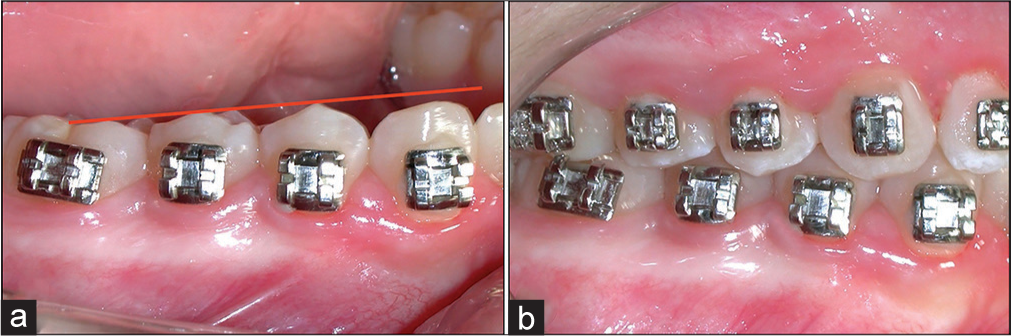 Figure 16
Figure 16- (a) A technical approach to improve the occlusal contacts in this area and avoid rebonding or bending archwires. (b) With bracket more cervical in the first premolar than the canine, it is possible to get an excellent intercuspidation in this area
Upper second premolars and first molars: The height of the mesial buccal cusp of the first molar is always lower than the buccal cusp of the second premolar, up to about 1 mm [Figures 17 and 18]. Thus, it can be stated that it is not possible to mount correctly from a higher of cusp; however, it is necessary taking into account the marginal ridges
 Figure 17
Figure 17- An undesirable step between second upper premolar and first molar
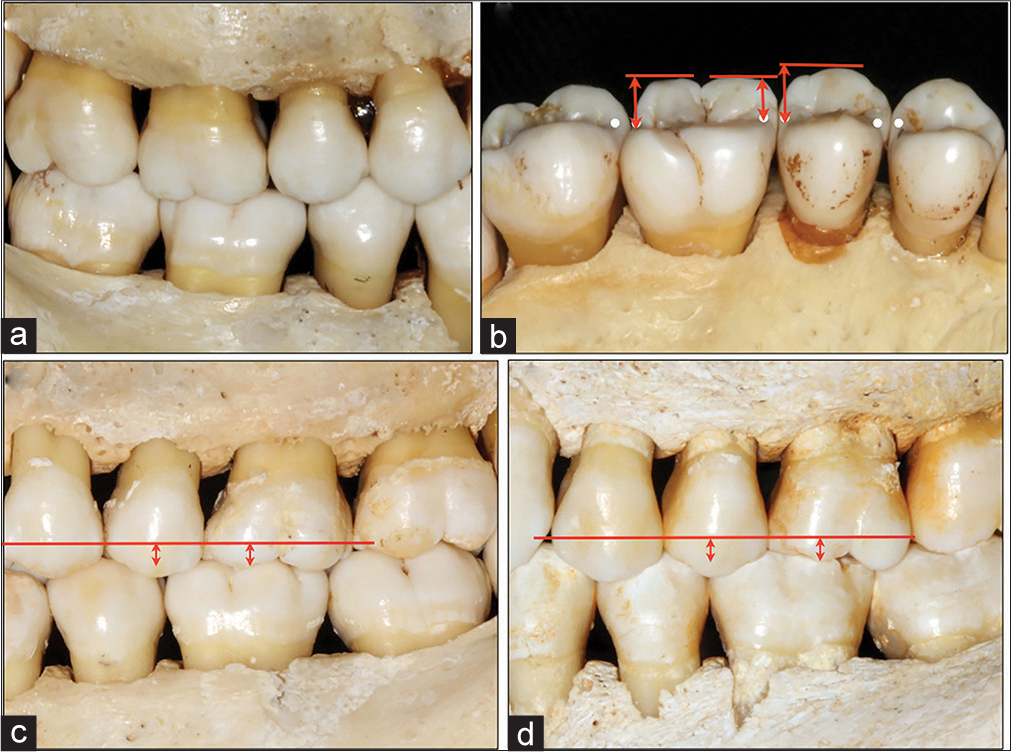 Figure 18
Figure 18- (a) Excellent intercuspation. (b) The height of the mesial buccal cusp of the first molar is always lower than the buccal cusp of the second premolar, up to about 1mm. (c and d) It is not possible to mount correctly from a height of cusp; however, it is necessary taking into account the marginal ridges
Third molars: Specifically in adult patients, it is necessary to mount the orthodontic appliance in all teeth to avoid occlusal interferences. This means that it is necessary to include the second molars and even the third molars if it they will be maintained-without third molars extractions [Figure 19]
 Figure 19
Figure 19- (a) It is necessary to mount the appliance in all teeth, mainly in adult patients. (b) This means that second molars should always be included. Similarly, if the third molars will be maintained, they also need to be included in the treatment
According to malocclusion. The cases of open bite and deep overbite are benefited from the treatment effectiveness when the brackets are mounted more incisal in the anterior teeth in deep overbite cases, and more cervical in open bite cases.[7]
In the same way, other malocclusion can benefit from this approach. Figures 20-22 illustrate a case with mild facial asymmetry, and asymmetric smile with great alteration of the occlusal cant and the smile line on one side compared with the opposite side, which was her main complaint. The solution was to bond the brackets in this anterior area according to the malocclusion, with the height of the canine bracket from one side different toward the other side. In this case, the leveling result presented a significant improvement.
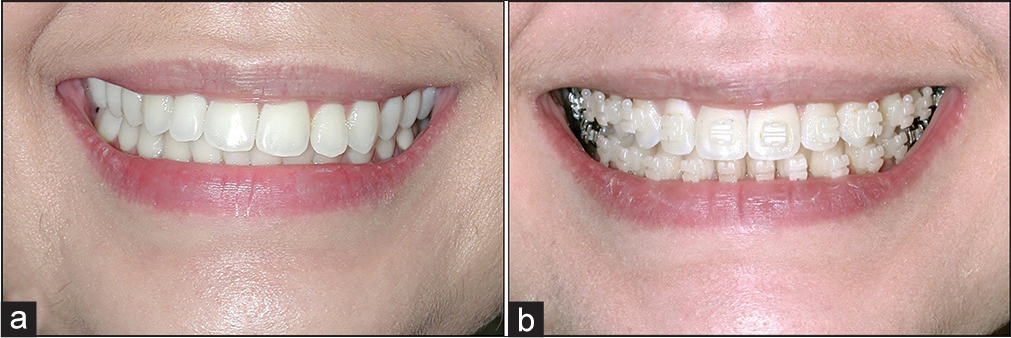
- (a) A case with asymmetric smile and alteration of the occlusal plane and the smile line. (b) The significant improvement of the occlusal plane and the smile line

- The appliance was mounted according to the malocclusion. The height of the canine bracket from one side is different to other side with the leveling resulting in a significant improvement
- (a) The case before treatment. (b) After treatment
Repositioning of brackets
The question that can be done regarding this item might be why it is necessary to reassemble the appliance. I must then review some articles related to this subject.
According to Polling: “The results generated by the preadjusted appliance (any fixed appliance-author comment) are limited by the ability of the orthodontist to adequately place the appliance and the adaptability of the selected appliance to individual patient variation. An orthodontist may have to reposition brackets or make adjustments to the orthodontic wires to obtain an excellent finished result.”[8]
Koo et al. comparing the accuracy of bracket placement between direct and indirect bonding techniques, concluded that neither technique yielded ideal bracket placement.[9]
Hodge et al., in a randomized clinical trial comparing the accuracy of direct versus indirect bracket placement, also concluded that there was no difference between mean bracket placement errors for direct or indirect methods.[10]
Redmond et al. evaluating the OrthoCAD bracket placement as a solution, verified as a result that it can help to reduce but not to eliminate the frequency and number of wire bending and repositioning appointments.[11]
Armstrong et al. performed a research to compare the accuracy in bracket positioning between two techniques: Localizing the center of the clinical crown and measuring the distance from the incisal edge. They concluded that the extent of error of bracket placement, regardless of which technique was used, demonstrates that archwire bending adjustments or repositioning of brackets will be necessary to achieve acceptable treatment results.[12]
Suárez and Vilar, evaluating the effect of constant height bracket placement on marginal ridge leveling using digitized models, verified that vertical placement bracket protocols, which ignore individual labial crown convexities and crown lengths, may introduce an initial bracket placement error which may lead to poor marginal ridge leveling at the end of treatment.[13]
Mota Júnior et al. aimed to evaluate the influence of clinical experience and the type of tooth (incisors, canines, and premolars) on the vertical accuracy of bracket placement with the Boone gauge. They concluded that operators are prone to fail in the placement of orthodontic attachments with the Boone gauge, despite their clinical experience in orthodontics.[14]
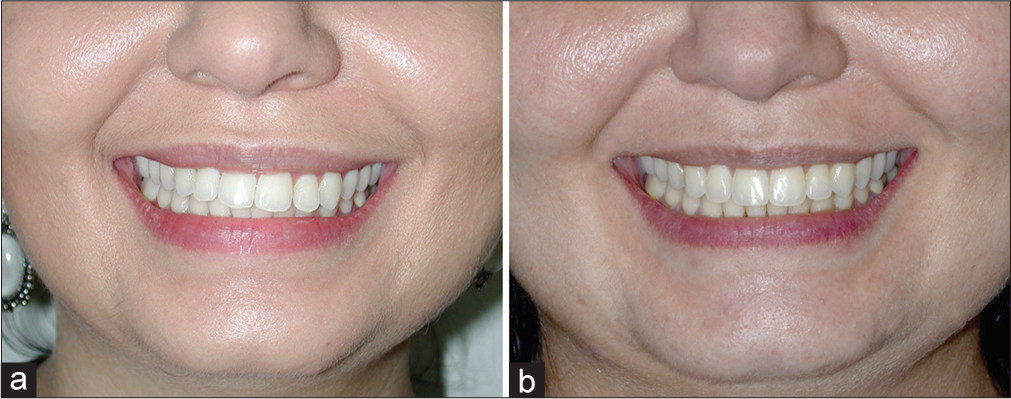
The question is: Bonding in optimum position is guarantee of perfect alignment and leveling? In unleveled teeth, the answer is NO. Why? There are many reasons why perfect bonding is not enough in unleveled and rotated teeth, as follows [Figure 23]:
- (a) The goals in leveling and alignments. There are many reasons why perfect bonding is not enough in unleveled and rotated teeth as follows: (b) Play between the archwire and slot. (c) Force diminution - reduction in force produced by an archwire, deflected within its elastic limits, as it returns to its original shape. (d) Brackets away from the center of resistance. (e) Action and reaction
The most frequent reason is inaccurate bracket placement. Since the surface of the tooth is curved, both mesiodistally and occluso-gingivally, misplaced brackets in the mesiodistal orientation result in rotational irregularities whereas those in the occlusogingival plane result in torque, as well as height errors. Brackets not aligned with the long axis of the tooth result in tip variations[15,16]
Play between the archwire and slot: Play between the archwire and slot are required to insert and remove archwires, but this compromise exact tooth control[15]
Force diminution: The force produced by an archwire deflected to engage a malpositioned tooth will diminish as the tooth moves until the minimum threshold of force is reached. At this point, tooth movement will stop before the archwire has completely returned to its original shape. In this case, the straight wire never becomes quite straight. Force diminution occurs in all directions of tooth movement. It is most evident in leveling an excessive Curve of Spee[15]
Brackets away from the center of resistance. Brackets cannot be placed at the center of resistance of a tooth. Consequently, the application of force to a tooth by an archwire also produces additional forces on the other adjacent teeth[15]
Action and reaction: On unleveled and out of alignment teeth to be exerted a force to extrude a tooth will also be a force to incline to the lingual side, and the other teeth will apply a force to intrude and tilt them to the labial side
Variations in tooth structure: Variations in tooth structure, such as irregular facial surfaces, crown-root angulations, and unusual crown shapes, require variations in tip, torque, rotation, and height parameters to achieve optimum results[15,16]
Variations in the maxillary/mandibular relationships: Differences in the vertical and anteroposterior jaw relationships require variations in the positions of maxillary and mandibular incisors[15]
Tissue rebound and need for overcorrection (giroversions).[17]
A typical case of bracket reposition advantage is seen in Figure 24, where spaces were closed in absence of upper laterals teeth by canines, and they were reshaped and brackets rebonded in better positions.
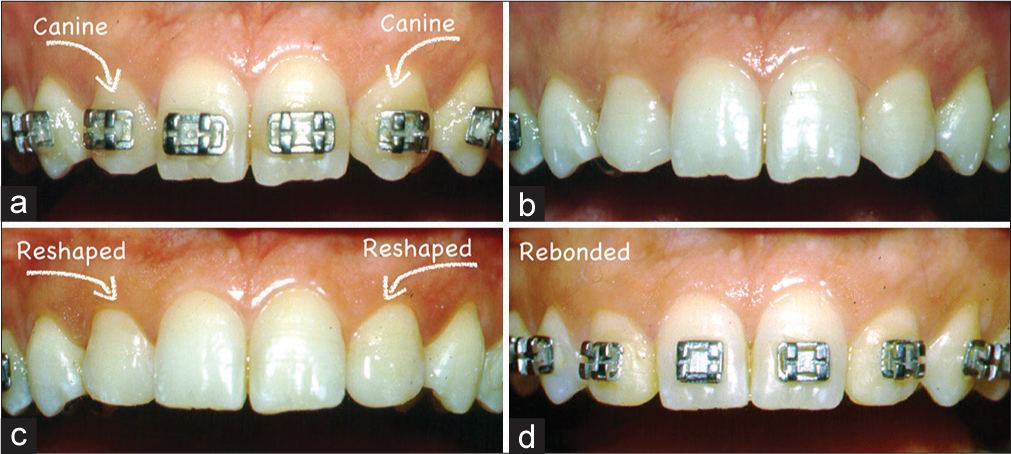
- A typical case of repositioning of brackets. Congenital absence of laterals teeth. (a) Spaces were closed. (b) Brackets removed. (c) Reshaped teeth. (d) Reposition of brackets
Make adjustments in the archwires
The question related to this item might be: Why make adjustments in the archwires? Let’s see what the literature states about “Returning to Polling.”[7] An orthodontist may have to reposition brackets or make adjustments to the orthodontic wires to obtain an excellent finished result. Hence, there’s a need to perform one or two procedures, replace brackets and/or make adjustments in the archwires.
Lossdörfer et al., in the analysis of the torque capacity of a completely customized lingual appliance of the next generation, found that it requires careful treatment planning to avoid undesired side effects when considering the periodontal architecture.[18]
Even with Scholz state Sachdeva[19] that it is necessary to bend archwires. In an interview, he affirms and illustrates that archwire modifications are required to achieve the desired alignment.[19]
Johnson proposes selecting custom torque prescriptions for the straight wire appliance, emphasizing that as a result, fewer time-consuming final torque adjustments are needed with stainless steel finishing wires.[20] It is important to note that he refers to less adjustments and not the elimination of these procedures.
Another important question concerns the gap between wire and slot. A bracket actually has the measurements provided by the manufacturers. Cash et al.,[21] in an evaluation of slot size in orthodontic brackets, ask this question: Are standards as expected? The results of this study indicate that orthodontic bracket slots are all larger than stated by the manufacturers.[21]
A dimensional evaluation of metallic slots bracket by Assad-Loss et al.[22] verify that the real dimension of the metallic brackets slot tested is larger.
Joch et al. verify that the accuracy of the manufacturers dimension slot is not to be taken for granted. A perfect finishing still requires correction bends put in by the orthodontist.[23]
Hence, to improve the occlusal contacts, an orthodontist has to reposition brackets or adjust the orthodontic wires, or even do both, in this order.
In some cases, it will be necessary, incorporate archwire bends to improve alignments like shown in Figure 25.
- (a and b) In some cases will be necessary increase or decrease bend in archwires to get better teeth alignments
To obtain appropriate points of contact between the lateral incisor and mandibular canine, it will often be necessary to incorporate or increase the offsets of the canines in the archwires [Figure 26]. A transferred case is seen in Figure 27, where bending was performed to improve occlusal contacts.

- (a and b) Incisor and canine will often be necessary to incorporate or increase the offsets of the canines in the archwires
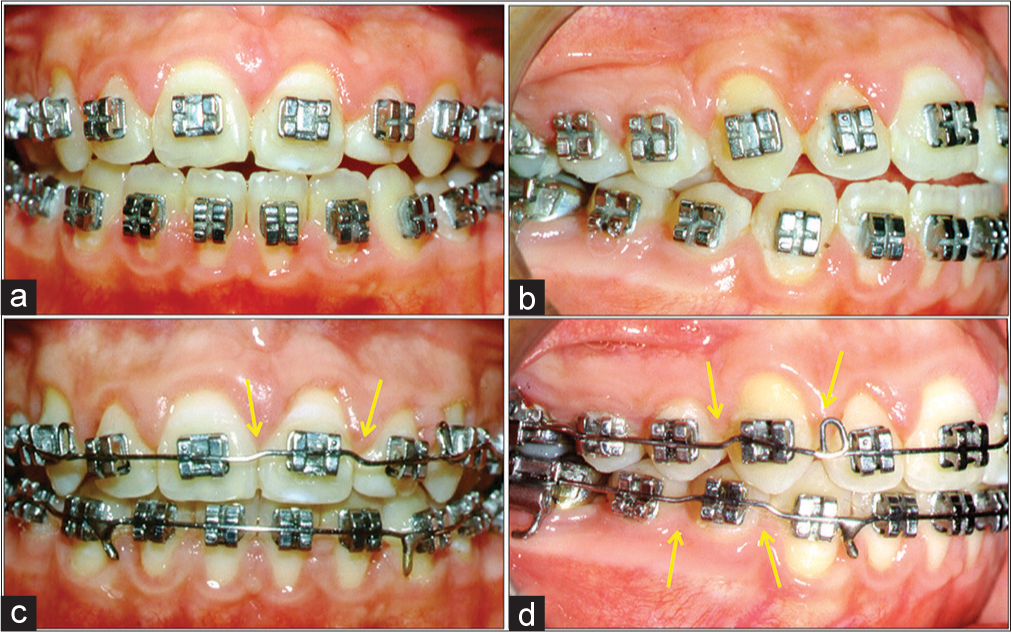
- (a and b) A transferred case. (c and d) In which the archwires were bended to improve intercuspidation (yellow arrows)
How can we make fewer mistakes in bracket placement and less wire bending? It is possible to take advantages from a traditional set-up [Figure 28], currently, from a virtual set-up and from orthodontic appliance mounting with this information. Still, some mistakes will remain.[24]
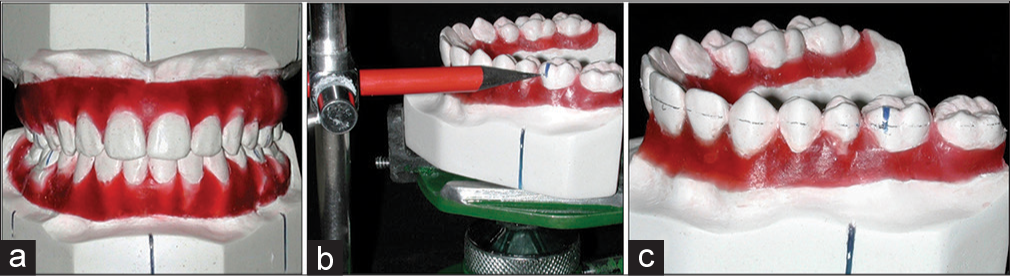
- To solve the problem of inaccurate bracket placement, (a) traditional or a virtual set-up can help. (b) Marking the standard height in molars and incisors. (c) A horizontal line is drawn by marking a central position of the orthodontic bracket slots
More than this, it will be necessary a good orthodontic training in basic arch bending. Dougherty[25] in a guest editorial mentioned: “Wendell Wylie, one of my great teachers, once said: A good orthodontist who knows the basis can treat well with barbed wire if need be; a poorly trained orthodontist will never treat well, even with the most sophisticated appliance.”[25]
Look at the face, teeth, and smile, not the appliance
At this moment, the most important thing is not to observe the appliance, but to concentrate the focus on the face, occlusion, and smile. Because the appliance will be removed, but these details will remain. For better understanding of this item, I must return to the checklist, which refers to esthetics and occlusion.
Face
Face in frontal view, with symmetry and balanced proportions
Face in profile view, with a total orthognathic profile. The lower face in profile with appropriate relationship and contour among nose, upper lip, lower lip, and chin. To this analysis, it is necessary to use some reference line. In this particular subject, the author prefers the “S” from Steiner [Figures 29-31].[26]
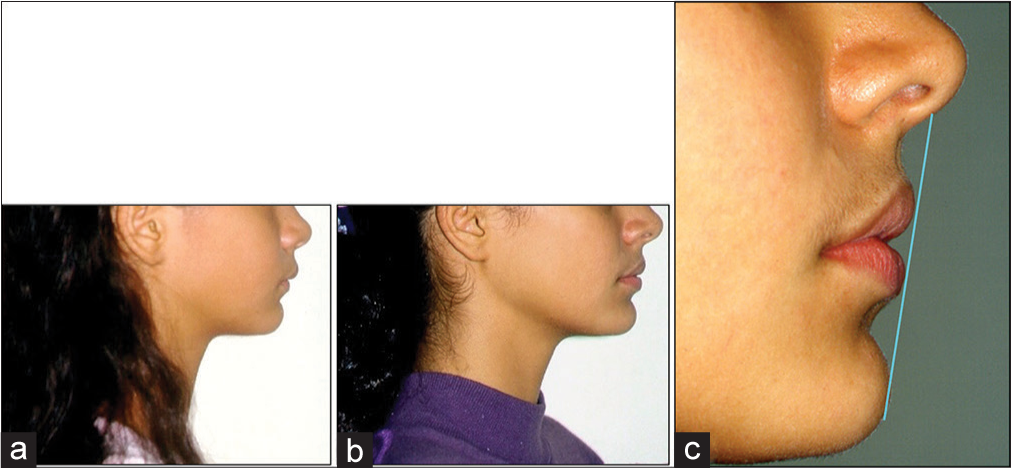 Figure 29
Figure 29- The goal in the lower face profile. (a) Before treatment. (b) After treatment. (c) “S” line with excellent relationship between nose, upper lip, lower lip, and chin, with agreeable curves
 Figure 30
Figure 30- Improvements in the lower face profile. (a) Before treatment. (b) After treatment. (c) Excellent relationship between nose, upper lip, lower lip, and chin, with agreeable curves
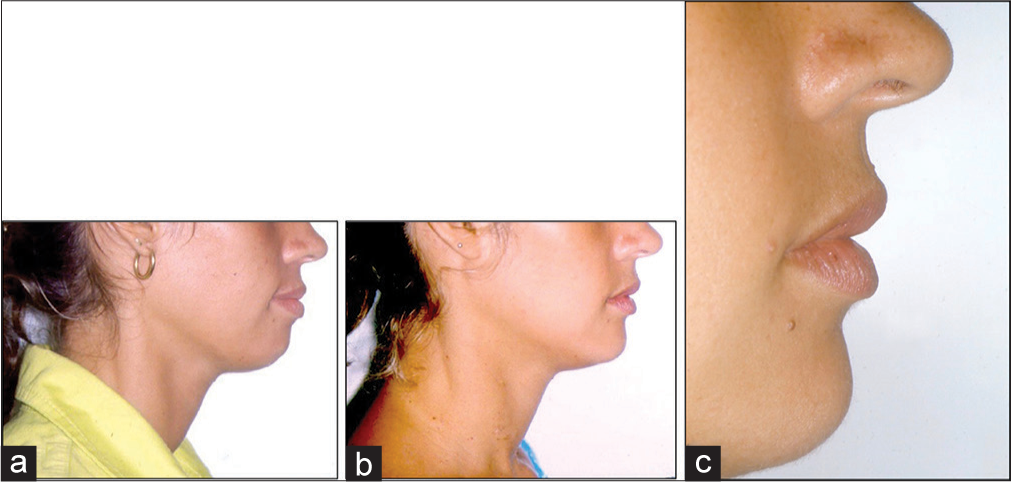 Figure 31
Figure 31- Premolar extractions can be beneficial to facial profile. (a) Before treatment. (b) After treatment and (c) close view of the face profile
Occlusion
This analysis should be done in three views:
-
I. Occlusal view:
Correct contact points: All spaces within dental arch have been closed
Absence of rotations
Leveling of marginal ridges: Even in cases with and without extractions. This mean, the correct alignment of the lingual surfaces of the maxillary anterior teeth and groves of posterior teeth; and the incisal edges of the mandibular anterior teeth and the buccal cuspid of the posterior teeth. The goal is to get the correct occlusion lines [Figures 32 and 33].[27]
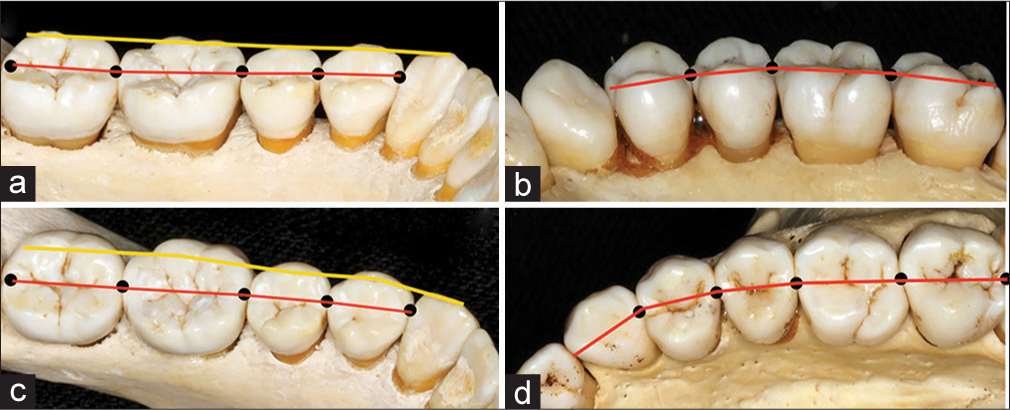 Figure 32
Figure 32- (a-d) Correct points of contact, absence of rotations, and leveling mandibular teeth. The occlusion lines of marginal ridges
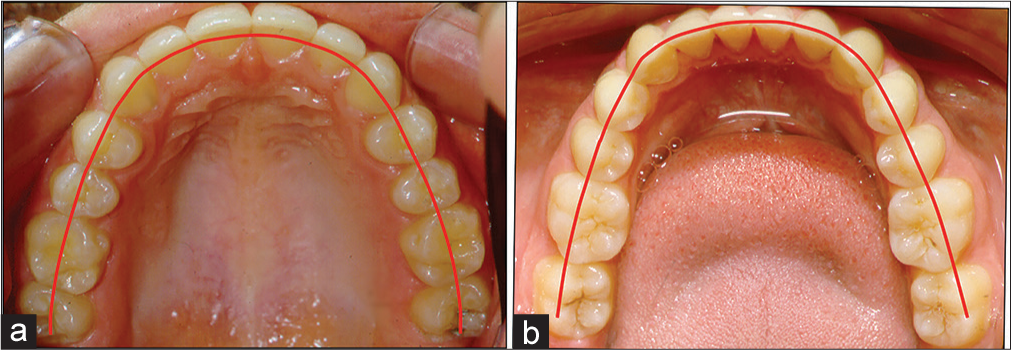 Figure 33
Figure 33- (a and b) Correct alignment of the maxillary teeth and the
-
Lateral view: From posterior to anterior:
Molar relationship: Upper first molar distal buccal cuspid must be located between first and second lower molars [Figure 34].[27] Even in extractions cases [Figure 35]
 Figure 34
Figure 34- (a and b) Molar relationship. Upper first molar distal buccal cuspid must be located between first and second lower molars
 Figure 35
Figure 35- (a-c) Molar relationship. Upper first molar distal buccal cuspid must be located between first and second lower molars even in extractions cases
Occlusal relationship: The buccal cusps of the maxillary molars, premolars, and canines must align within the interproximal embrasures of the mandibular posterior teeth
Occlusal contacts: A major objective of orthodontic treatment is to establish correct and maximum intercuspation of opposing teeth [Figure 36]
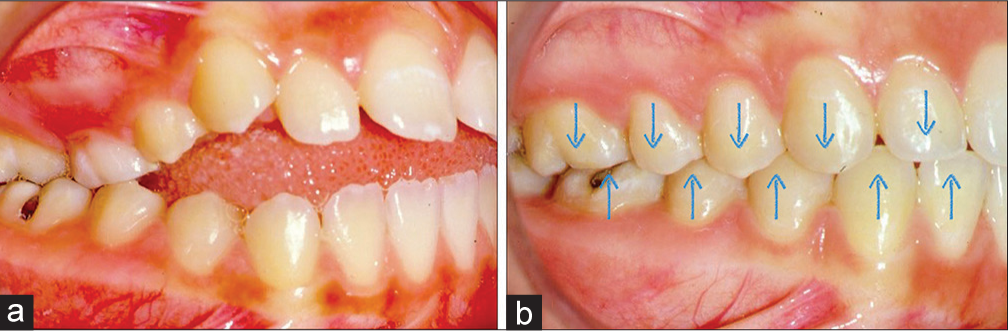 Figure 36
Figure 36- Occlusal contacts. (a) At the beginning of treatment and (b) after treatment the correct and maximum intercuspation of opposing teeth
Anterior torque [Figure 37]: In the anterior region, the mandibular incisal edges should be in contact with the lingual surfaces of the maxillary anterior teeth
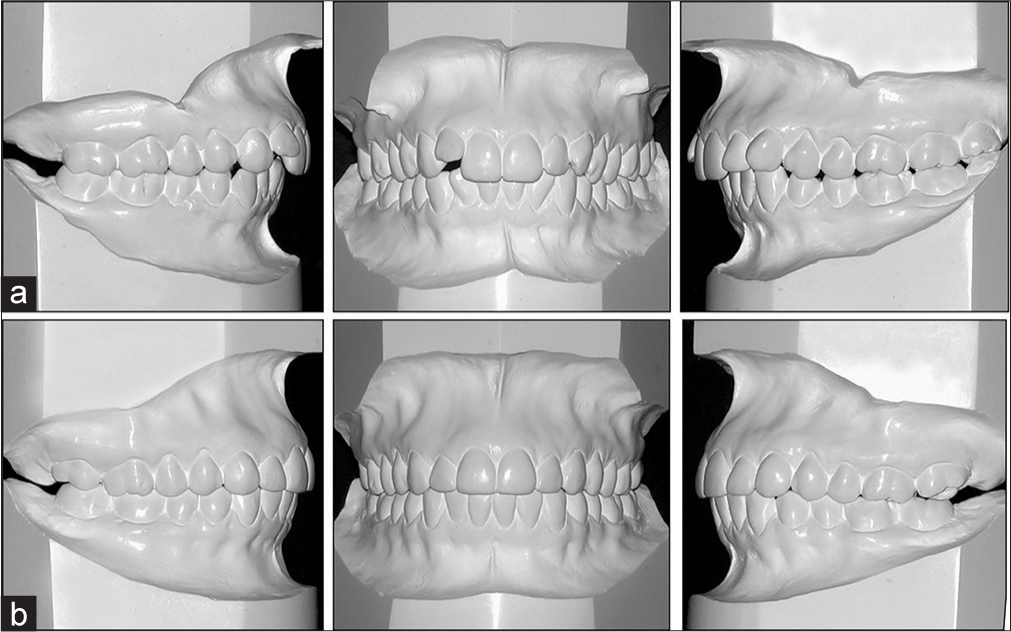 Figure 37
Figure 37- (a) Clinical case before and (b) After treatment where occlusal relationship of all teeth can be observed with its occlusal contacts, correct anterior torque, and a flat occlusal plane
Occlusal plane: Flat occlusal plan or slightly Curve of Spee [Figure 38].[28]
 Figure 38
Figure 38- (a) Occlusal plane before treatment. (b) After treatment. Flat occlusal plan or slightly Curve of Spee
-
Anterior view:
Upper anterior mesial-distal inclinations. Slightly to midline inclinations-artistic positions [Figure 39a]
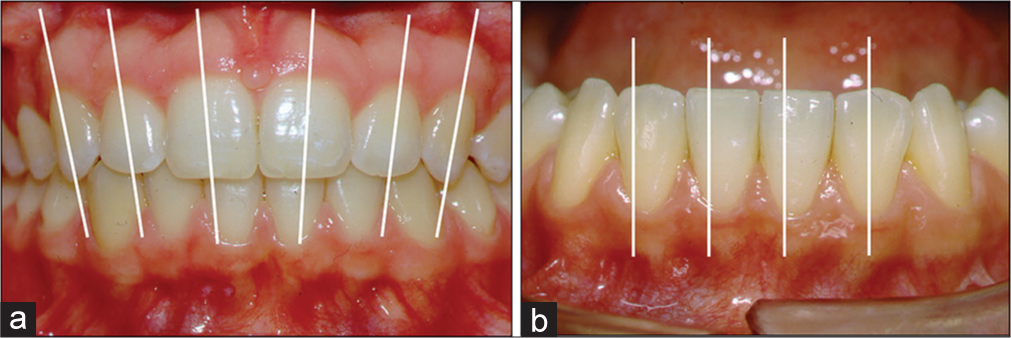 Figure 39
Figure 39- (a) Mesial distal inclinations of the upper anterior teeth. (b) Lower incisors in a mesial-distal inclination or in a vertical relationship
Lower incisors mesial-distal inclinations: Slightly to midline or vertical [Figure 39b]
Midline: Upper and lower dental midlines coincident with each other and with the face. It is accepted a deviation from 0 to 2, 5 mm to the face
Posterior upper torque-en mass: The buccolingual inclination of the maxillary and mandibular posterior teeth should be assessed using a flat surface that is extended between the occlusal surfaces of the right and left posterior teeth.[25] In the maxillary arch, the straight edge should contact the lingual cusps of the maxillary molars and premolars. The buccal cusps should be within 1 mm of the surface of the straight edge [Figure 40a and b][27]
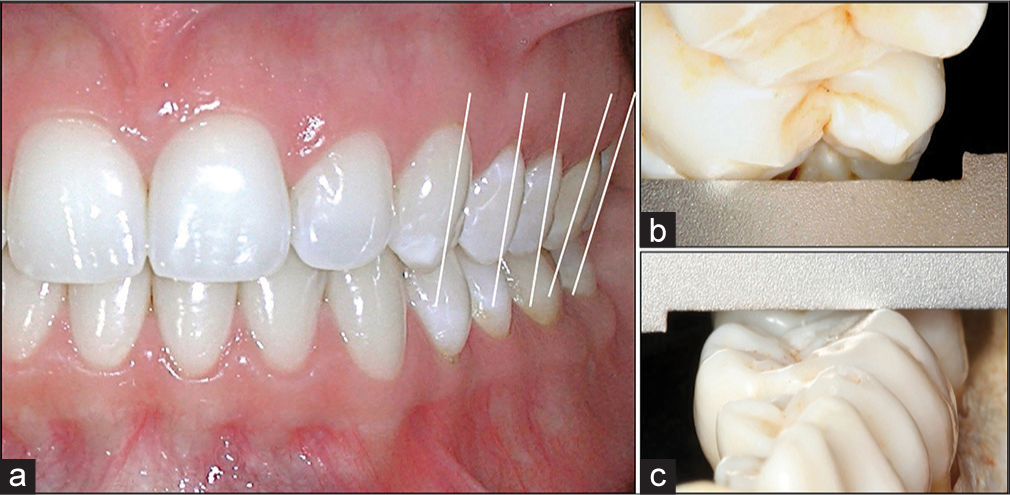 Figure 40
Figure 40- (a) Posterior upper torque en mass with canines, premolars and molars with the same inclination, or molars slightly more. (b) In the maxillary arch, the straight edge should contact the lingual cusps of the maxillary molars and premolars. The buccal cusps should be within 1 mm of the surface of the straight edge. (c) Progressive posterior lower torque. A straight edge should contact the buccal cusps of contralateral mandibular molars. The lingual cusps should be within 1 mm of the surface of the straight edge
Posterior lower torque-progressive. When positioned in this manner, a straight edge should contact the buccal cusps of contralateral mandibular molars. The lingual cusps should be within 1 mm of the surface of the straight edge [Figure 40c].[27]
Smile
-
Dental esthetics (from the checklist):
-
Lips at rest: From 15 to 30 years of age, lips at rest should be expose from 3 to 5 mm.[29]
Motta et al.[28] determine how much of the upper central incisor crowns are visible in Brazilian subjects with their lips at rest at different ages and sex. They conclude that older Brazilians display less of their upper central incisors and more of their lower central incisors than young Brazilians. Women show more of their upper incisors than men, while men display more of their lower central incisors than women [Figure 41].
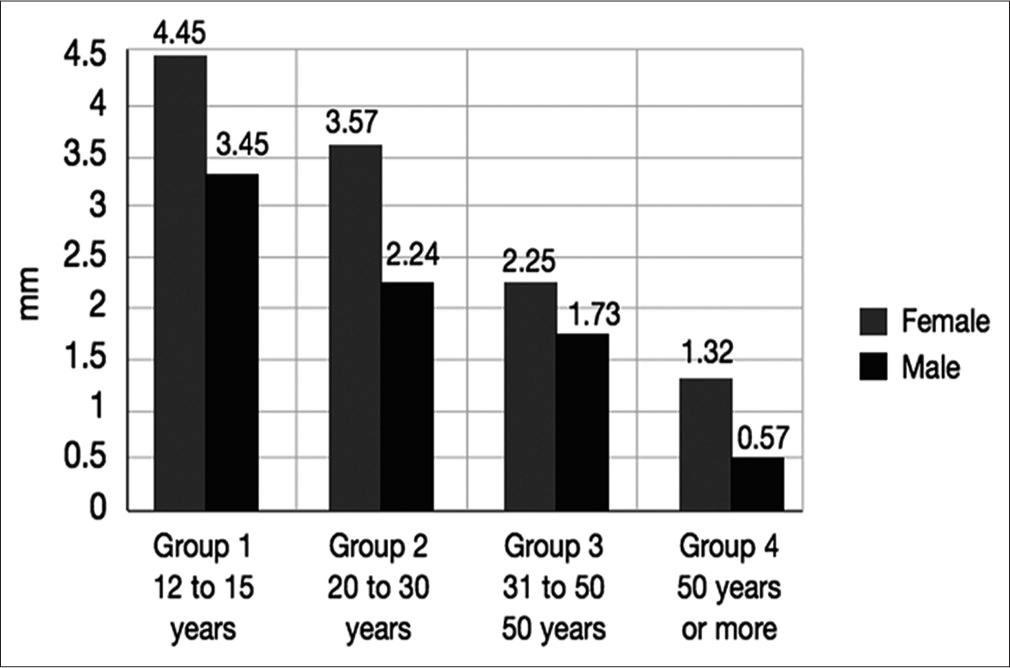 Figure 41
Figure 41- Display of the incisors as functions of age and sex
-
-
Smile (from the checklist):
Incisal edges of upper teeth-smile arch. Upper edges should be parallel to the contour of the lower lip. The lower teeth should follow the same line
Gingival outline and exposure: Symmetrical and parallel to the upper lip contour. Up to 1–2 mm of exposure [Figure 42]
 Figure 42
Figure 42- Gingival outline and exposure should by symmetrical and parallel to the upper lip contour and up to 1-2 mm of exposure. (a and b) The main complain was the gingival display on lateral. (c) After correction of the gingival contour. (d) That was performed with lingual appliance
Incisors display on smiling: 10–12 mm
Proportional shapes, positions, and sizes [Figure 43a-c]
 Figure 43
Figure 43- (a-c) Midline; mesiodistal inclinations; contact points; proportional shapes, positions, and sizes. (d) View in esthetic proportions decreasing from anterior to posterior, including at least 10 upper teeth
View in esthetic proportions: Decreasing from anterior to posterior horizontally [Figure 43d]. 100:60%.[30,31]
Improve the functional occlusion
The goals are [Figure 6]:
Reshape teeth anatomically
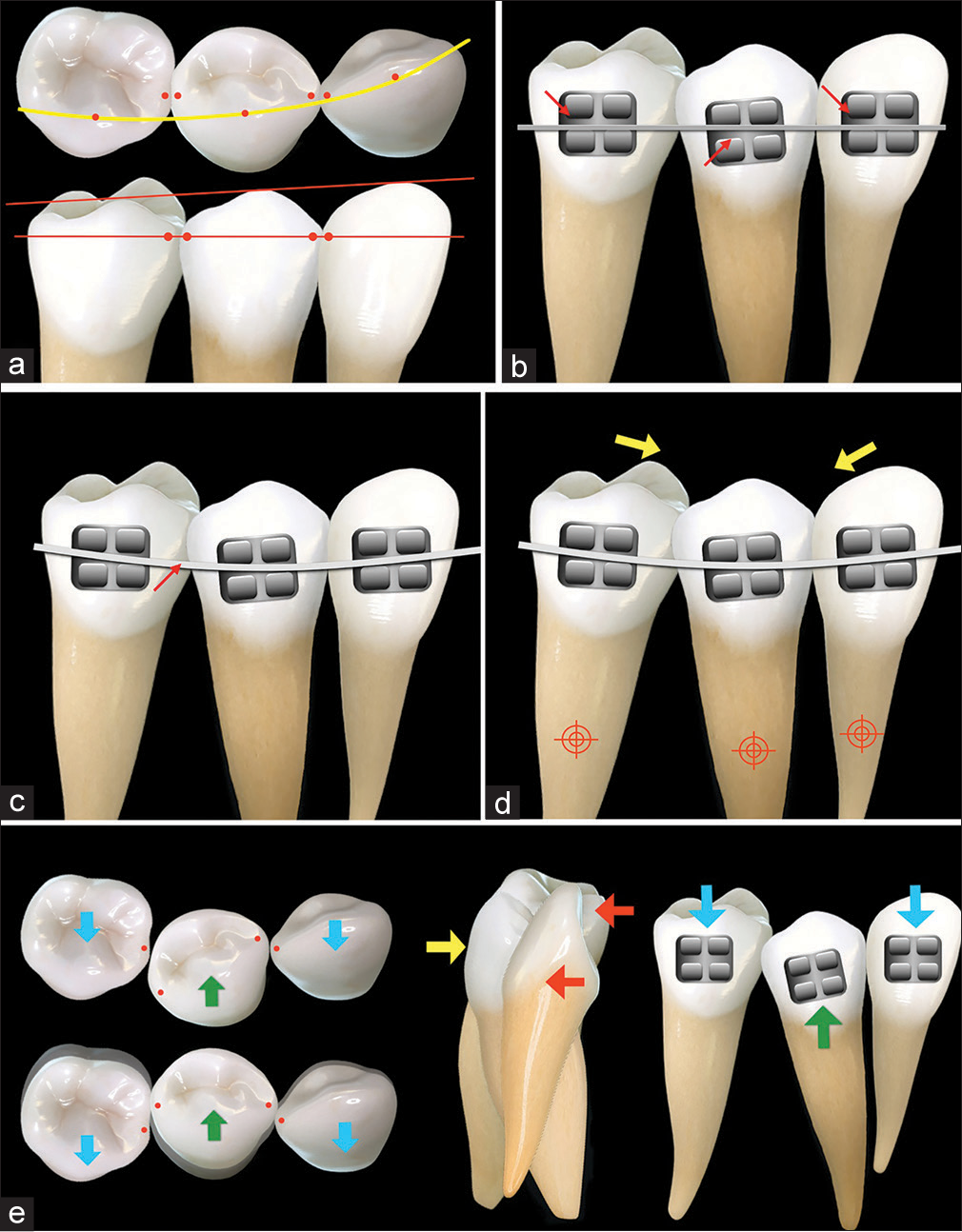
Incisal edges and embrasures: Slightly convex with well-defined embrasures. To perform this procedure follow these steps: (1) explain to the patient; (2) avoid overheating; (3) use low speed; (4) use a diamond bur; (5) look directly; (6) polish with thin discs; and (7) women have them more rounded [Figure 44].[17]

- Incisal edges should be slightly convex with well-defined embrasures. (a) At the end of orthodontic treatment, with irregular incisal edges. (b) After debonding. (c) After anatomical recontouring the incisal edges. (d) Shapes of diamond stones recommended for the contouring. (e) It is important to look the patient directly
The sequence of procedures should be to first do the edges looking frontally and then the interdental embrasures.
Reshape anatomically the marginal ridges and other anatomic alterations.
Plan the retention
There are tree situation to plan the retention in the lower arch: No retention, temporary retention, and permanent retention.
Those cases that require no retention are of anterior cross-bites corrected with adequate overjet and overbite [Figure 45][33]
 Figure 45
Figure 45- Cases that requires no retention: Anterior cross-bite corrected with adequate overjet and overbite. (a) Before treatment. (b) After treatment. (c) 6-year follow-up without retention
Temporary retention – Upper: Retain the plate with a circumferential clamp or wraparound with stainless steel wire 036. Lower: Retain in the normal or regular cases with a bonded cuspid to cuspid teeth with stainless steel wire 0.028”. In complex cases, such as adult or retreatment with rotation, bond multiple strands 0.020” in all lower six teeth, or even extended to first premolar teeth [Figures 46 and 47]
 Figure 46
Figure 46- Upper temporary retention: (a) a plate with circumferential clamp or “wraparound” with stainless steel wire 036”. (b) Multiple strands 0.020” bonded to keep the diastema closed
 Figure 47
Figure 47- (a and b) Lower retention in the normal or regular cases. Bonded cuspid to cuspid with stainless steel wire 0.028”. (c and d) In complex cases, such as adult or retreatment with rotation, bonded multiple strands 0.020” in all lower six teeth, or extended to first premolars teeth
Permanent retention: With a normal oral healthcare, it is possible to maintain a lower fixed retainer for many years, such as a case treated from 1978 to 1980 and with a 3-3 lower retainer in a 32-year follow-up [Figure 48].
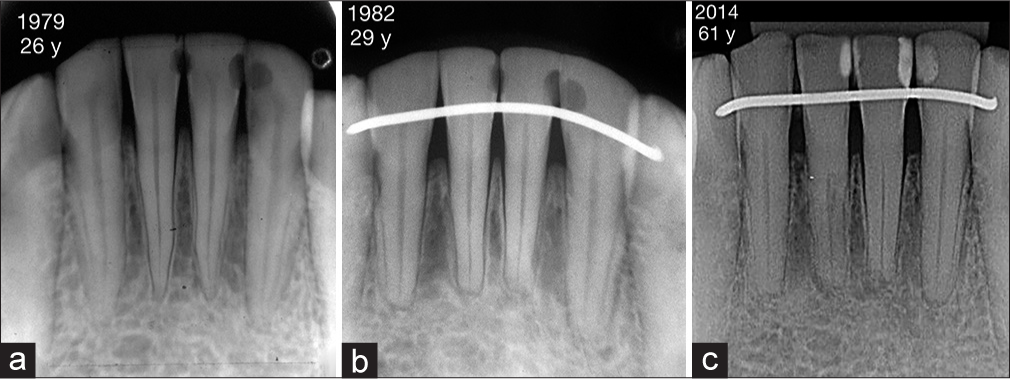 Figure 48
Figure 48- With a normal oral health care it is possible to maintain a lower fixed retainer for many years. (a) A patient at the beginning of treatment in 1979 with 26 years. (b) Lower fixed retainer bonded in 1982, with 29 years old. (c) A 3 - 3 lower retainer in 32 year follow-up
Plan the appliance removal
Before appliance removal, it might be necessary to:
Bond the lower retention one appointment before appliance removal, to test this bonded material [Figure 49a]
 Figure 49
Figure 49- Before appliance removal, it is necessary to: (a) lower retention placement one appointment before appliance removal; (b) elastics to adjust the occlusion always on hooks in the archwires; and (c) occlusal adjustment. Teeth reshaping is required due to preorthodontic contacts, lack of contacts during orthodontic, and genetics that change the anatomic form and do not allow adequate occlusal contacts. Check with a carbon paper and remove this first contact
Use elastics to adjust the occlusion. I prefer to adjust the posterior occlusion by replacing brackets and archwire bends. Then, if some occlusal adjustment is necessary in the anterior area, a last vertical elastic will be used by the patient in a square shape in hooks fixed on the archwires, never on teeth hooks [Figure 49b]
Total appliance removal in one session. If you decide to let one arch (upper or lower) until the next appointment, you will lose the natural adjustment of the occlusal contacts that occur taken advantage of increased thickening of the periodontal ligament
Occlusal adjustment: Teeth reshaping, which are required due to: preorthodontic contacts; lack of contacts during orthodontics; and genetics that change the anatomic form of the occlusion at that time and do not allow adequate occlusal contacts. Check with a carbon paper and remove this contacts first [Figure 49c].
Conclusions
Following this order of steps: (1) define clearly your goals; (2) have a checklist; (3) improve in bracket placement; (4) repositioning of brackets; (5) make adjustments in the archwires; (6) look at the face, teeth and smile, not the appliance; (7) improve the functional occlusion; (8) reshape teeth anatomically; (9) plan the retention; and (10) plan the appliance removal, it is possible to reach excellent finishing results in orthodontic treatments.
To achieve great results, it is crucial to keep in mind that in clinical orthodontic practice, it is important to clearly define your goals, to know the basics (foundations), have technical domain (training and repetition) and implement the plan. All those combined, the result will be inevitable: Success.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Common errors observed at the American board of orthodontics clinical examination. Am J Orthod Dentofacial Orthop. 2017;152:139-42.
- [Google Scholar]
- Functional Occlusion: From TMJ to Smile Design. St Louis: Mosby Elsevier; 2007.
- Evaluation of the vertical alterations of the upper second molars after the alignment and leveling phase using the MBT technique. Dental Press J Orthod. 2013;18:115-20.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Malocclusion of the Teeth (7th ed). Philadelphia: SS White; 1907.
- Clinical considerations on the vertical positioning of orthodontic accessories. Rev Dental Press Ortodontia Ortop Facial. 2000;5:45-51.
- [CrossRef] [Google Scholar]
- A method of finishing the occlusion. Am J Orthod Dentofacial Orthop. 1999;115:476-87.
- [CrossRef] [Google Scholar]
- Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116:346-51.
- [Google Scholar]
- A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J Orthod. 2004;31:132-7.
- [CrossRef] [PubMed] [Google Scholar]
- The OrthoCAD bracket placement solution. Am J Orthod Dentofacial Orthop. 2004;125:645-6.
- [Google Scholar]
- A comparison of accuracy in bracket positioning between two techniques – Localizing the centre of the clinical crown and measuring the distance from the incisal edge. Eur J Orthod. 2007;29:430-6.
- [Google Scholar]
- The effect of constant height bracket placement on marginal ridge levelling using digitized models. Eur J Orthod. 2010;32:100-5.
- [Google Scholar]
- Evaluation of the vertical accuracy of bracket placement with the Boone gauge. Am J Orthod Dentofacial Orthop. 2015;148:821-6.
- [Google Scholar]
- Normal torque of the Buccal surface of mandibular teeth and its relationship with bracket positioning: A study in normal occlusion. Braz Dent J. 2006;17:155-60.
- [Google Scholar]
- JCO/interviews Dr. Bjorn U. Zachrisson on excellence in finishing. Part 2. J Clin Orthod. 1986;20:536-56.
- [Google Scholar]
- Analysis of the torque capacity of a completely customized lingual appliance of the next generation. Head Face Med. 2014;10:4.
- [Google Scholar]
- Interview with an innovator: SureSmile chief clinical officer Rohit C. L. Sachdeva. Am J Orthod Dentofacial Orthop. 2010;138:231-8.
- [Google Scholar]
- Selecting custom torque prescriptions for the straight-wire appliance. Am J Orthod Dentofacial Orthop. 2013;143:S161-7.
- [Google Scholar]
- An evaluation of slot size in orthodontic brackets – Are standards as expected? Angle Orthod. 2004;74:450-3.
- [Google Scholar]
- Bracket slot and archwire dimensions: Manufacturing precision and third order clearance. J. Orthod. December. 2010;37:241-249.
- [CrossRef] [PubMed] [Google Scholar]
- Vertical accessories positioning in orthodontics fixed appliance. Rev Dent Press Ortodontia Ortop Facial. 2006;11:66-75.
- [CrossRef] [Google Scholar]
- Read the label before taking. Am J Orthod Dentofacial Orthop. 1987;91:442-4.
- [CrossRef] [Google Scholar]
- Cephalometrics as a clinical tool In: Kraus BS, Riedel RA, eds. Vistas in Orthodontics. Philadelphia: Lea & Febiger; 1962.
- [Google Scholar]
- Objetive grading system for dental cast and panoramic radiographs. Am J Orthod Dento Facial Orthop. 1998;114:589-99.
- [Google Scholar]
- Display of the incisors as functions of age and gender. Aust Orthod J. 2010;26:27-32.
- [CrossRef] [Google Scholar]
- Principles of cosmetic dentistry in orthodontics: Part 1. Shape and proportionality of anterior teeth. Am J Orthod Dentofacial Orthop. 2004;126:749-53.
- [CrossRef] [PubMed] [Google Scholar]
- Finishing procedures in orthodontics: Dental dimensions and proportions (microesthetics) Dental Press J Orthod. 2013;18:147-74.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of occlusal trauma on gingival recession and gingival clefts. J Indian Prosthodont Soc. 2013;13:7-12.
- [CrossRef] [PubMed] [Google Scholar]






