Translate this page into:
Principles of Orthognathic Surgical Correction of Skeletal Anterior Open Bite
Address for correspondence: Dr. Farhad B. Naini, Department of Orthodontics, Maxillofacial Unit, St George’s Hospital and Medical School, London, United Kingdom. E-mail: farhad.naini@yahoo.co.uk
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
This article describes the principles of orthognathic surgical correction of skeletal anterior open bite (AOB), including a description of the aetiological factors involved in the development of predominantly skeletal AOBs, description of the presenting diagnostic features, the principles of treatment planning, orthodontic preparation, and postoperative requirements.
Keywords
Anterior open bite
orthognathic surgery
skeletal
Introduction
Anterior open bite (AOB) may be defined as a vertical space between the maxillary and mandibular incisor teeth when the posterior teeth are in occlusion.[1] The etiology of the degree of incisor overbite may involve skeletal, and/or dental and/or environmental factors, which may combine to determine the degree of incisor overbite. However, the extent to which these various aetiological factors are responsible for the vertical discrepancy is variable. The dentofacial morphological relationships often point to the major component in the etiology though in many cases, the clinician may remain uncertain as to the degree of influence of each aetiological factor.[2]
If the primary etiology of an AOB is a hyperdivergent facial growth pattern, which refers to an excessive divergence of the maxillary, occlusal, and mandibular planes in relation to each other and to the anterior cranial base, the terms skeletal open bite[3] or apertognathia (Latin apertus: Open; Greek gnathos: Jaw) may be used.[4]
The potential for attempting to restrict vertical maxillary development in an adolescent, growing patient with vertical maxillary excess (VME) has been described in detail elsewhere.[5] However, there are three principal methods to surgically correct an AOB of primarily skeletal etiology in a non-growing adult patient:
-
Differential posterior impaction of the Le Fort I osteotomized maxilla
Rotation of the maxillary occlusal plane round the transverse axis with differential posterior impaction permits forward autorotation of the mandible to close an AOB. Orthodontic preparation requires an element of proclination of the maxillary incisors, as the effect of surgical posterior impaction is relative retroclination of the maxillary incisors. Therefore, the orthodontic preparation for this approach is significantly different to the maxillary segmental surgical approach described below. This approach is described in this paper.
-
Segmental impaction of the posterior maxilla
The Le Fort I osteotomized maxilla is vertically segmentalized either distal to the canines or distal to the lateral incisors. The posterior and anterior segments, which will have been preoperatively aligned and leveled independently, will be moved separately. The posterior segment is superiorly repositioned, allowing forward autorotation of the mandible to close the AOB, and the anterior segment is repositioned vertically to obtain the ideal maxillary incisor exposure in relation to the upper lip. This approach has been described in detail elsewhere.[6]
-
Isolated mandibular surgery
Anterior rotation (in the direction of mouth closing) of the distal segment of the mandible following a bilateral sagittal split osteotomy may be used to close some AOBs. This approach has been described in detail elsewhere.[7]
Ideally, the choice of procedure should be determined based on the diagnostic features of the individual patient.[1] For example, an obvious and potentially convenient vertical step in the maxillary occlusal plane between the anterior and posterior segments may be better approached with segmental surgery though surgeon preference for a technical option is also a factor.
Diagnosis and Etiology
Understanding the etiology of every malocclusion and dentofacial discrepancy is critical, but the significance of understanding the etiology of AOBs is more consequential, as it will have a direct bearing on the choice of treatment strategy and will fundamentally influence its potential stability.[1,6] It should be noted that an AOB is not a diagnosis per se, but a clinical sign that may be present in a number of dentofacial configurations, with an array of potential causes.
The various possible aetiological factors in the development of an AOB are presented in Table 1 though it should be remembered that the etiology may be multifactorial, involving several aetiological factors.[4]
| Etiology | Presenting features |
|---|---|
| Skeletal: Increased LAFH | Excessive increase in LAFH (usually due to posterior VME), with the incisors unable to erupt to such an extent that they fully compensate for the face height, resulting in an AOB |
| Usually correlated with an increased mandibular plane angle and increased gonial angle, but these are only a correlation, and depend on the posterior face height | |
| Skeletal: Reduced ramus height | Vertical deficiency in mandibular ramus height, leading to an increased anterior to posterior face height ratio, a steep mandibular plane angle, a clockwise rotation of the mandible and an AOB |
| Soft tissue: Tongue size, resting position and/or activity | Resting tongue position
|
Adaptive swallowing pattern
|
|
Endogenous tongue thrust
|
|
| Note: As the etiology of an AOB is due primarily to the activity of the tongue in this rare condition, the vertical skeletal height relationships may well be normal | |
| Nasorespiratory function and head posture | Postural changes to the head (extending the head back by tilting it around the transverse axis of rotation) due to partial nasal airway obstruction and excessive long-term mouth breathing allow downward and backward posturing of the mandible, downward positioning of the tongue, and overeruption of the posterior teeth in both dental arches. Such changes were previously assumed to be the main aetiological factors resulting in skeletal AOB in tall face individuals.[9-13] The facial appearance of such individuals was formerly, and erroneously, referred to as “adenoid facies”[14] |
| Note: It appears to be more likely that the skeletal pattern and vertical facial growth tendency are predominantly genetically determined, but that environmental influences may result in additional changes, perhaps in some cases exacerbating the effects, for example, worsening an AOB | |
| Habit: digit sucking | Non-nutritive sucking behavior is very common in the infant, who appears to derive comfort from the habit and is of little importance in the deciduous dentition |
| The intensity and prolonged duration into the permanent dentition are likely to cause dentoalveolar discrepancies: | |
| Pathological | Idiopathic condylar resorption
|
Neuromuscular conditions
|
|
Systemic conditions
|
|
| Traumatic | Bilateral condylar fractures, particularly in a growing patient, potentially leading to temporomandibular joint ankylosis |
| Iatrogenic | Poorly controlled extrusive orthodontic forces on the posterior dentition, leading to their extrusion, and thereby opening of the bite anteriorly |
AOB – Anterior open bite; VME – Vertical maxillary excess; LAFH – Lower anterior face height; SLE – Systemic lupus erythematosus
Presenting features
Lower anterior face height
In a patient with an average posterior face height (i.e., average mandibular ramus height), a skeletal AOB may occur due to a significant increase in the lower anterior face height (LAFH), often related to posterior VME. In such patients, the LAFH will be significantly greater than the midfacial height. If the incisor teeth are unable to erupt in relation to the increased LAFH, an AOB ensues [Figure 4].

- A forward resting tongue position may be evident with a patient in repose
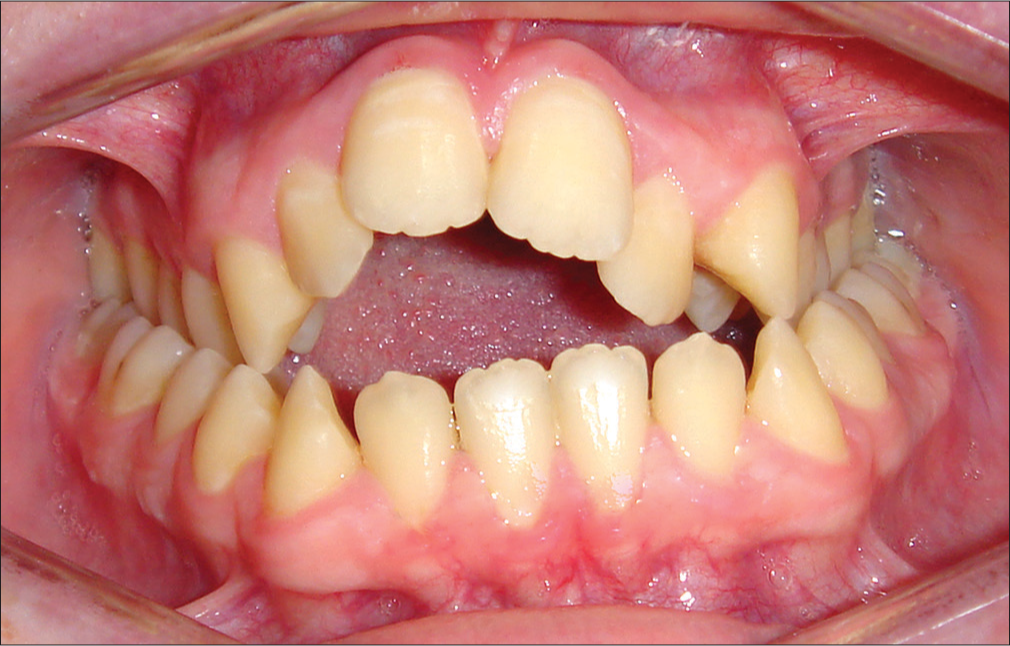
- Asymmetrical anterior open bite in a patient aged 17 years with a continued thumb sucking habit. Narrowing of the maxillary arch is common in such cases
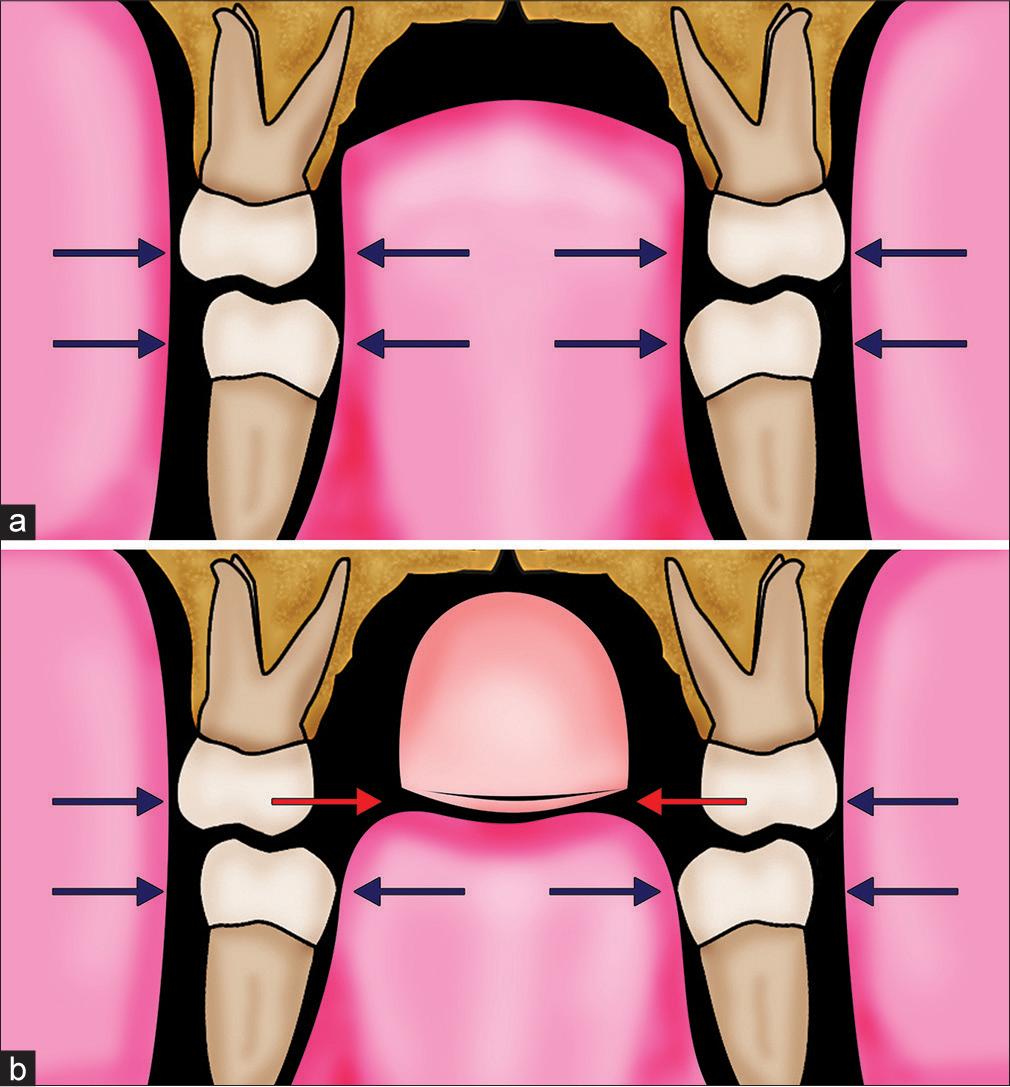
- (a) Schematic representation of the average patient, with the teeth in a zone of soft-tissue equilibrium between the pressure from the soft-tissue forces of the cheeks and tongue. (b) In a patient with a prolonged digit-sucking habit, the digit (e.g., thumb) displaces the tongue inferiorly. The excessive buccal forces from the cheek musculature due to forces generated by sucking pressure will be offset by those from the highly muscular tongue situated between the mandibular dentition but lead to narrowing of the maxillary dentition where they are unopposed. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
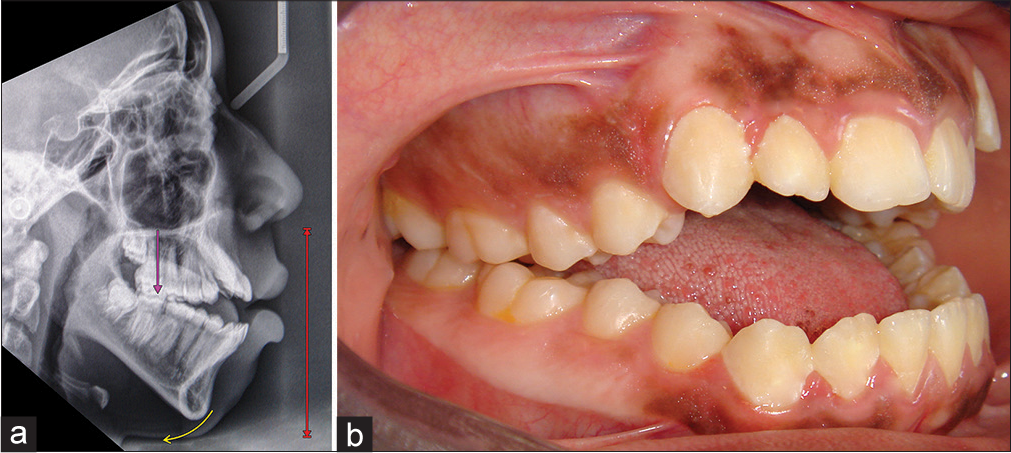
- (a and b) Skeletal anterior open bite due to increased lower anterior face height. The mandibular ramus height is average. There is posterior VME, which has led to a posterior rotation of the mandible, moving the chin downward, and backward relative to the face. There is an adaptive forward position of the tongue. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning, and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Anterior to posterior face height ratio
It is possible that a patient may present with an average LAFH, but significantly reduced posterior face height (i.e., reduced mandibular ramus height). Therefore, the anterior to posterior face height ratio will be significantly increased [Figure 5].
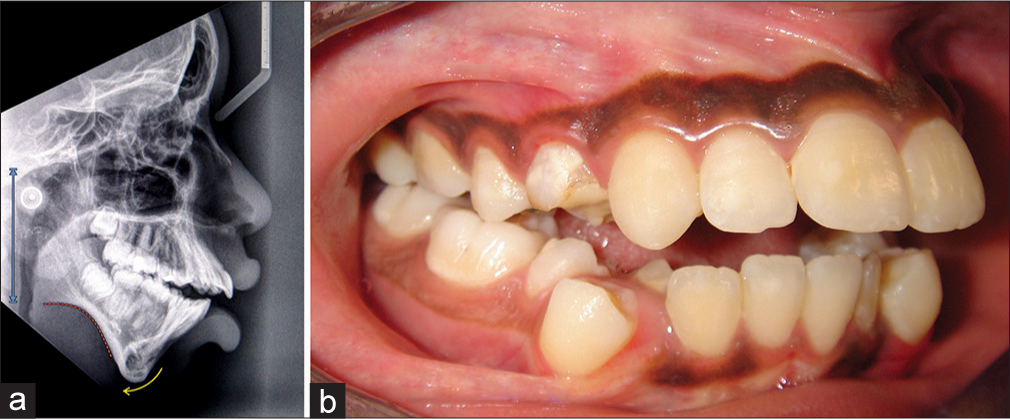
- (a and b) Skeletal anterior open bite due to reduced ramus height. The vertical position of the maxilla is average, as is the lower anterior face height. The mandible is rotated posteriorly, and there is a pronounced antegonial convexity in the morphology of the mandible. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission.)
Relative inclination of the maxillary, occlusal, and mandibular planes (Sassouni analysis)
In a well-proportioned face, the maxillary, occlusal, and mandibular planes should converge symmetrically toward an approximate area of intersection located near the occiput (back of the skull) [Figure 6a]. If either jaw is vertically disproportionate, its associated plane will not converge with the others. If the area of convergence of these planes is positioned in front of the occiput, towards the face, the planes will diverge anteriorly [Figure 6b]. This skeletal pattern is associated with markedly different anterior and posterior facial heights and correlates with an AOB tendency, which Sassouni classified as a “skeletal open bite.”[3,16]
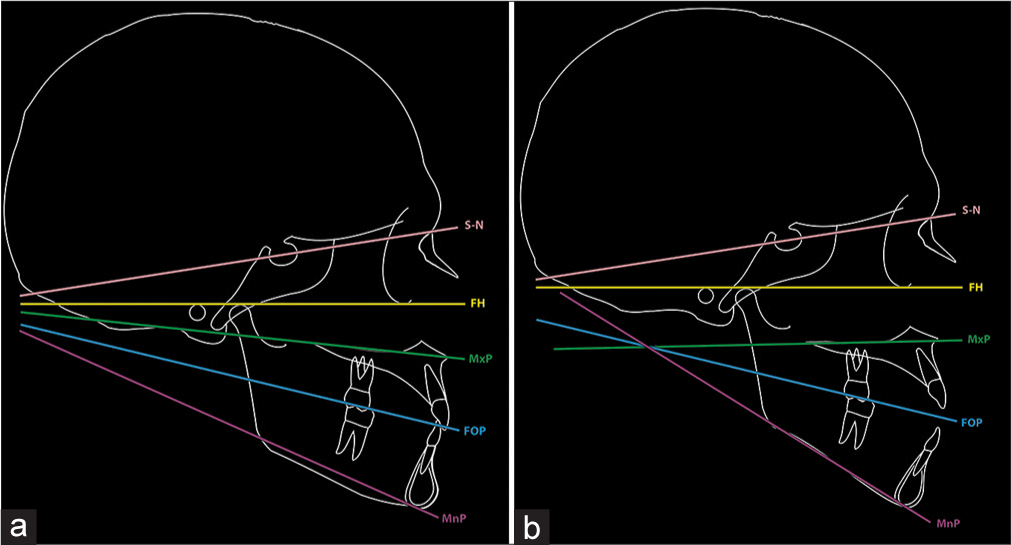
- (a) According to the Sassouni analysis, in a well-proportioned face, the horizontal facial planes should converge symmetrically toward an approximate area of intersection located near the occiput. If any part of the face is vertically disproportionate, its associated plane will not converge with the others. (b) If the area of convergence of the horizontal facial planes is positioned in front of the occiput, toward the face, the planes will diverge anteriorly; this skeletal pattern is associated with markedly different anterior and posterior facial heights and correlates with an anterior open bite tendency, termed a “skeletal open bite”. MxP – Maxillary plane; MnP – Mandibular plane; FOP – Functional occlusal plane; FH – Frankfurt plane; SN – Sella-nasion plane. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; reprinted with permission)
Pattern of rotational development of the jaws
The pattern of rotational growth of the jaws in relation to each other and the craniofacial complex has a direct influence on the morphological characteristics of vertical skeletal discrepancies and thereby to the development of AOBs of predominantly skeletal etiology.
Abnormal bimaxillary posterior rotational growth leads to the divergent rotational growth of the maxilla and mandible. The maxilla will be tilted down posteriorly, as will the maxillary occlusal plane, resulting in an anticlockwise rotation of the maxilla observed in the right profile view. A posterior (backward, clockwise) growth rotation of the mandible also results. This pattern of mandibular growth rotation may be indicated by Björk’s seven structural signs [Table 2 and Figure 7].[17]
| Structural signs | Backward (posterior) mandibular growth rotation | |
|---|---|---|
| 1 | Inclination of the condylar head | Backward |
| 2 | Curvature of the mandibular canal | Straight canal |
| 3 | Shape of the lower border of the mandible | Convex lower border and antegonial notch |
| 4 | Inclination of the mandibular symphysis (bony chin) | Backward inclination, reduced chin projection |
| 5 | Interincisal angle | Reduced |
| 6 | Intermolar and interpremolar angle | Reduced |
| 7 | LAFH | Increased |
LAFH – Lower anterior face height
![Björk’s seven structural signs, which may be used to indicate the pattern of posterior (backward) mandibular growth rotation [Explanation of the numbers - Table 2]. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)](/content/9/2017/7/4/img/APOS-7-157-g007.png)
- Björk’s seven structural signs, which may be used to indicate the pattern of posterior (backward) mandibular growth rotation [Explanation of the numbers - Table 2]. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Björk’s facial polygon is a useful method of analyzing the effects of various cranioskeletal angular relationships on the jaws in the sagittal and vertical planes.[18] An obtuse “saddle angle” formed between the anterior and middle cranial fossae may be found in patients with skeletal open bite, and this angle is set relatively early in life [Figure 8]. Richardson[19] compared the craniofacial morphology of 110 AOB individuals with the same number of deep overbite individuals (matched in respect of age and sex) and found that the LAFH was considerably greater, on average, in AOB cases compared with deep overbite. However, the difference could not be directly attributed to differences in linear values for Björk’s facial polygon but seemed to be related more to the obtuse gonial and articular angles, i.e., a question of cranioskeletal shape rather than size.
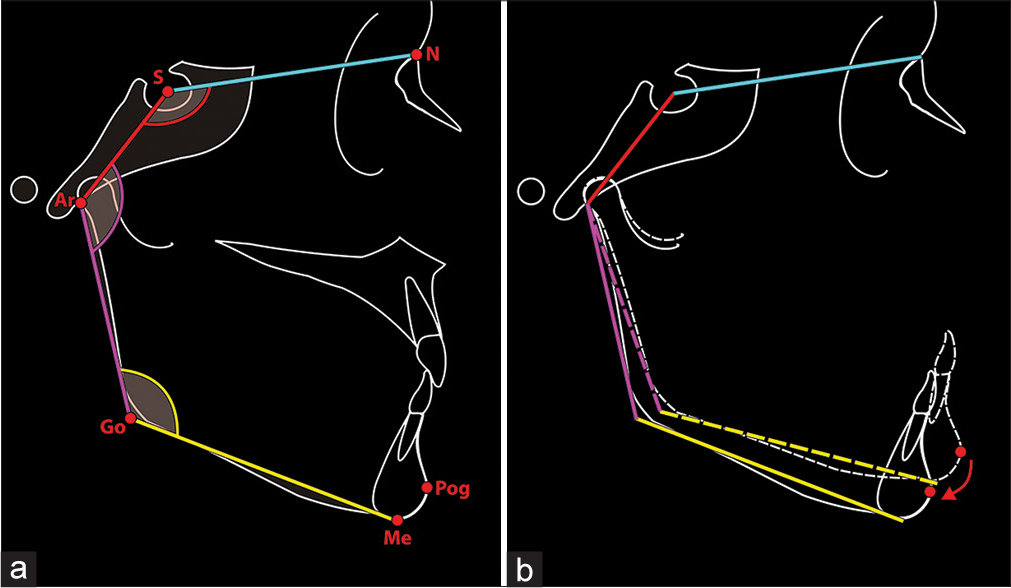
- (a) Björk’s polygon, demonstrating the saddle angle, articular angle, and gonial angle. (b) An increase in the articular angle will lead to downward and backward movement of the mandibular incisors (and chin) and potential opening of the bite. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011; used with permission)
Sagittal skeletal base relationship
Sagittal discrepancies may be primary but present with a skeletal AOB, for example, sagittal mandibular excess or deficiency due to mandibular macrognathia or micrognathia. Alternatively, or concomitantly, sagittal discrepancies may be secondary to the vertical skeletal growth pattern, for example, a normal mandible may rotate downward and backward in relation to posterior VME (Class I rotated to a Class II). Either way, posterior maxillary impaction will result in forward autorotation of the mandible, i.e., the position the mandible would have occupied had it not been for the posterior VME. The sagittal position of the mandible subsequently may be corrected by mandibular repositioning.
Upper lip-maxillary incisor relationship
The degree of maxillary incisor exposure is of paramount importance in diagnosis and treatment planning. In a skeletal AOB, the maxillary incisors may have reached their eruptive potential but have been unable to meet the opposing mandibular incisors due to the excessive increase in LAFH. Therefore, the maxillary incisor exposure in relation to the upper lip may be average or even increased. In such cases, as the maxillary incisors are already in a reasonable position relative to the upper lip, any extrusion of the maxillary incisors may appear very unsightly, as well as being prone to relapse. Preparatory orthodontics should aim at alignment without extrusion of the maxillary incisors, and the open bite will be closed by elevation of the posterior maxilla and subsequent forward autorotation of the mandible [Figure 9].
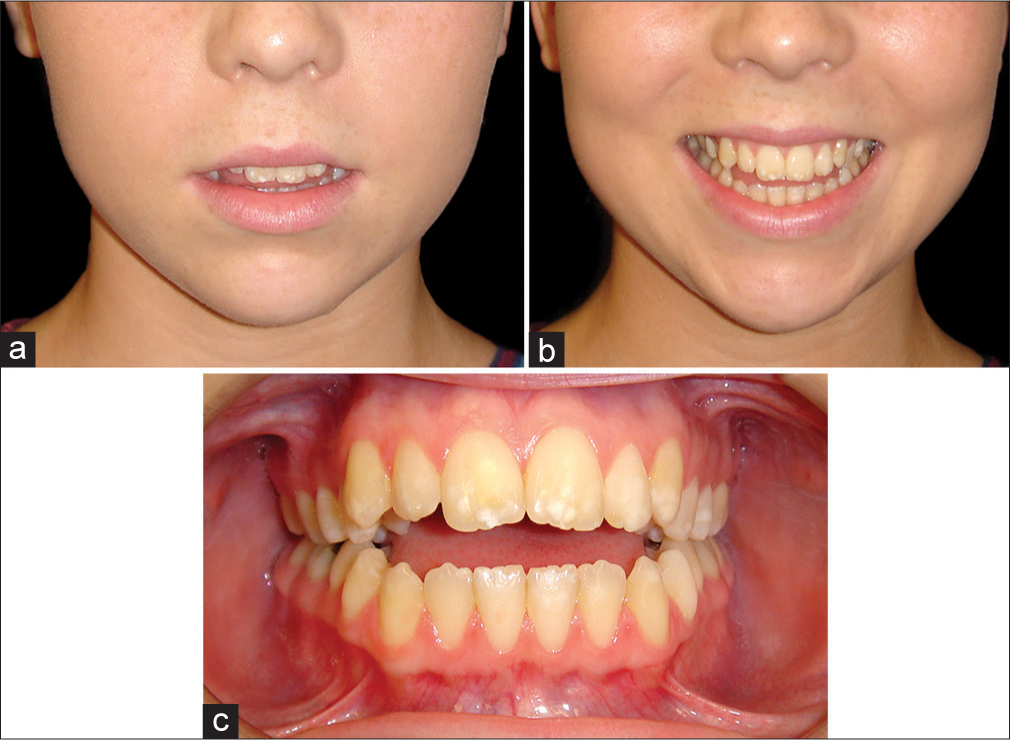
- (a and b) Example of a skeletal anterior open bite with adaptive tongue posture, with good lip-incisor relationship at rest and smiling. Therefore, the problem is entirely posterior vertical maxillary excess and posterior mandibular rotation. Lower anterior face height is slightly increased, and there is a mild incomplete lip seal. Preparatory orthodontic treatment should aim to maintain the lip-incisor relationship, and impact the posterior maxilla
Conversely, if there is a significant additional soft-tissue element to the etiology of a skeletal AOB, the forward resting tongue position may well have impeded the eruption of the maxillary incisors. In frontal view, the posterior maxillary dentition will be at an inferior level to the anterior dentition, and there will either be an increased sagittal curve to the maxillary arch or an obvious vertical step between the posterior and anterior maxillary dentition. The anterior dentoalveolar vertical maxillary deficiency due to the restrictive effect of the forward positioned tongue will often lead to a reduced maxillary incisor display or in extreme cases a “no tooth show” smile [Figure 10]. In such situations, a degree of leveling by extrusion of the maxillary incisors in the preparatory orthodontics is likely to remain stable postoperatively as the tongue will readapt to the new anterior dentolabial relationships. Alternatively, an anterior segmental maxillary setdown may be required in addition to posterior maxillary impaction.
- (a and b) Example of an anterior open bite with a significant soft tissue (tongue) etiology. Maxillary incisor exposure is reduced at rest and on smiling. An important treatment aim should be to increase the maxillary incisor exposure
Nasolabial angle
The upper and lower components of the nasolabial angle should be evaluated separately, as they vary independently [Figure 11].[20] In tall face patients with a skeletal AOB, particularly those with a Class II skeletal pattern, the nasolabial angle tends to be obtuse, and the upper lip posteriorly inclined [Figure 12].[21] The clinical relevance is that following a posterior maxillary impaction, there is likely to be a requirement for a maxillary advancement as well, otherwise there is risk of exacerbating an already obtuse nasolabial angle.
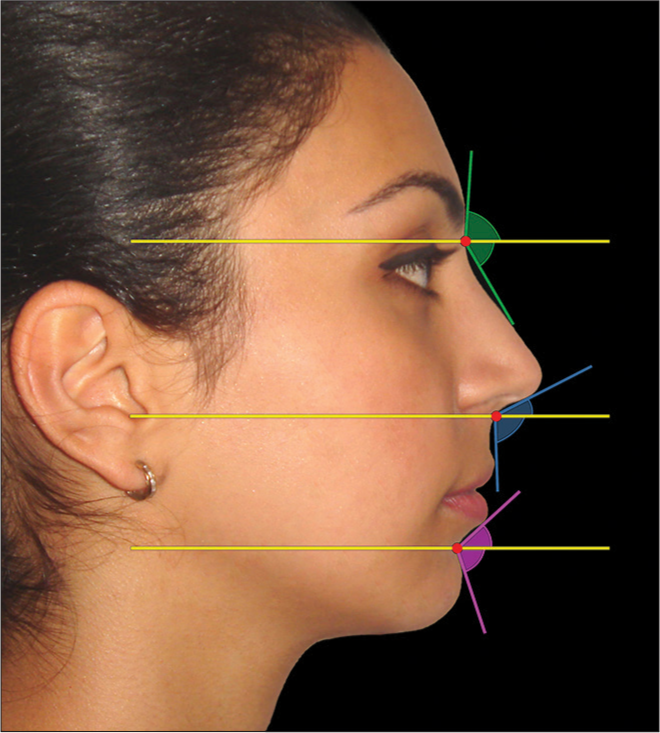
- Angular profile parameters may be visually separated into upper and lower components and a qualitative decision made as to whether they are obtuse, average, or acute. The patient should be in natural head position. The nasofrontal, nasolabial, and mentolabial angles are demonstrated separated into the upper and lower components by a true horizontal line. The nasolabial angle has an upper (columellar) component and a lower (upper lip) component. These two components may vary independently. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)

- A Class II patient with increased lower anterior face height and a skeletal anterior open bite. The nasolabial angle is obtuse and the upper lip posteriorly inclined
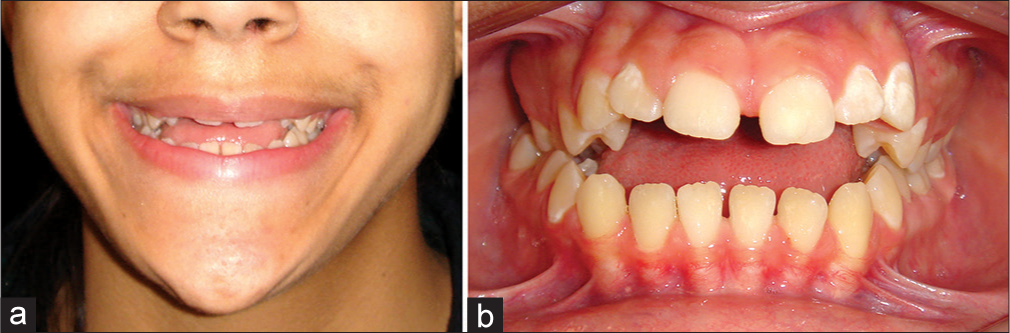
The tongue
The role of the tongue in the etiology of AOB must be a matter for consideration during diagnosis and treatment planning. If there is an abnormally large tongue, for example, in a Class III AOB patient [Figure 13], or abnormal tongue function, surgical correction of an AOB may be prone to relapse. If the tongue is significantly enlarged (e.g., Beckwith–Wiedemann syndrome) on clinical examination (true macroglossia), consideration may need to be given to tongue reduction surgery (reduction glossectomy) though this is uncommon. If required, a useful technique, described by Egyedi and Obwegeser,[22] involves the resection of an anterior V-shaped wedge and an oval midline excision from anterior to the vallate papillae.[1]

- (a and b) Female patient with severe Class III skeletal pattern and anterior open bite, and a large tongue
An AOB predominantly due to the action of the tongue is extremely rare. This so-called endogenous tongue thrust is associated with obvious sigmatism (lisping) and symmetrical AOB with bimaxillary dentoalveolar proclination, usually with a normal face height. This condition is likely to be due to an underlying abnormality in the neuromuscular control of the tongue and is thereby difficult to correct, and any treatment is likely to be highly unstable. However, in most patients with a part soft-tissue etiology to their AOB, the forward tongue position and atypical swallowing behavior are adaptive to the AOB, often secondary to a prolonged digit-sucking habit. Adaptive tongue postures and adaptive swallowing patterns will often readapt to the new dentolabial relationship following orthognathic surgery, and in general do not impose limitations on surgical correction of an AOB.
Principles in Planning the Surgical Correction of Skeletal Anterior Open Bite
The surgical correction of AOB includes patients whose treatment may involve a differential impaction of the maxilla. This includes cases of skeletal AOB and VME, with greater posterior than anterior vertical maxillary growth. The maxillary plane is canted down posteriorly. The treatment for such conditions involves Le Fort I downfracture of the maxilla and differential posterior maxillary impaction, i.e., moving the posterior maxilla superiorly more than the anterior maxilla, often referred to as a “posterior impaction.” The mandible may then autorotate forward, thereby helping to correct the LAFH. The vertical exposure of the maxillary incisors in relation to the upper lip may be correct or may require reduction. Alternatively, the anterior maxilla may need to be repositioned inferiorly if necessary.
The two most significant parameters in planning the surgical correction of an AOB are the maxillary incisor relationship to the upper lip (the “lip-incisor” relationship), and the LAFH. The correction of an AOB and the reduction in LAFH are both achieved by superior repositioning of the posterior maxilla and the subsequent forward autorotation of the mandible. The degree of posterior maxillary impaction required essentially will be dictated by the size of the AOB and the initial LAFH.[4]
Incisor inclination preparation for posterior maxillary impaction
In association with a differential posterior impaction of the maxilla, the maxillary incisors will retrocline. The amount of retroclination is important in surgical planning, as a compensatory degree of incisor proclination must be built into the preoperative orthodontic preparation, such that the maxillary incisors will return to their correct inclination with surgery.[23] If insufficient proclination is built into the preoperative orthodontics, the maxillary incisors will become excessively retroclined with surgery. Alternatively, if too much proclination is built into the preoperative orthodontics, or the degree of planned surgical posterior maxillary impaction is not achieved, then the incisors will remain somewhat proclined following surgery [Figure 14].
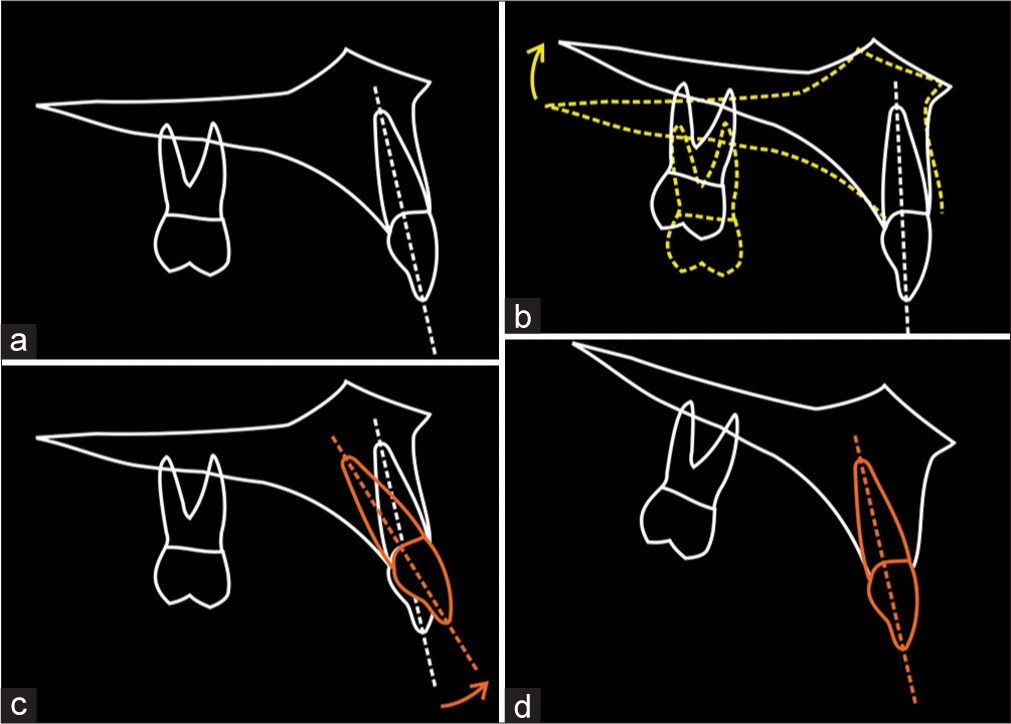
- Incisor inclination preparation for differential posterior maxillary impaction. (a) In the preoperative position, with the maxillary incisors at an average inclination. (b) In association with a differential posterior impaction of the maxilla, the maxillary incisors will retrocline. They are now excessively retroclined. (c) Therefore, a compensatory degree of incisor proclination must be built into the preoperative orthodontic preparation. (d) As such, the maxillary incisors will effectively retrocline as the maxilla rotates with the posterior impaction, thereby correcting their inclination with surgery. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
The amount of change in inclination of the maxillary incisors depends on the amount of differential posterior impaction of the maxilla. However, the ratio of both these variables also depends on the sagittal length of the maxilla, and the geometrical relationship between these three variables has been described [Figure 15].[23] The anatomical length of the maxilla is usually measured from anterior to posterior nasal spine. However, the effective length of the maxilla is from the maxillary incisors to the first molar cusp tip, from where the posterior impaction is usually measured. For example, a differential posterior impaction of 6 mm will lead to a retroclination of the maxillary incisors of almost 10° if the effective maxillary length is 35 mm, and 6° if the maxillary length is 55 mm. The greater the differential impaction and the shorter the length of the maxilla, the greater will be the change in inclination of the maxillary incisors.[23]
![Posterior maxillary impaction has a retroclining effect on the maxillary incisors. The effect is proportional to the amount of impaction (i) and the length of the maxilla (x). A formula has been described to calculate the amount of proclination that should be incorporated during preoperative orthodontic treatment.[23]. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)](/content/9/2017/7/4/img/APOS-7-157-g015.png)
- Posterior maxillary impaction has a retroclining effect on the maxillary incisors. The effect is proportional to the amount of impaction (i) and the length of the maxilla (x). A formula has been described to calculate the amount of proclination that should be incorporated during preoperative orthodontic treatment.[23]. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Orthodontic preparation for mandibular autorotation
The mandibular incisors usually will have been retroclined by the lower lip as the mandible rotated posteriorly during growth. In preparation for forward autorotation of the mandible, the mandibular incisors will need to be proclined such that their inclination effectively corrects with the mandibular autorotation [Figure 16].[24] This needs to be planned cephalometrically pretreatment and checked preoperatively.
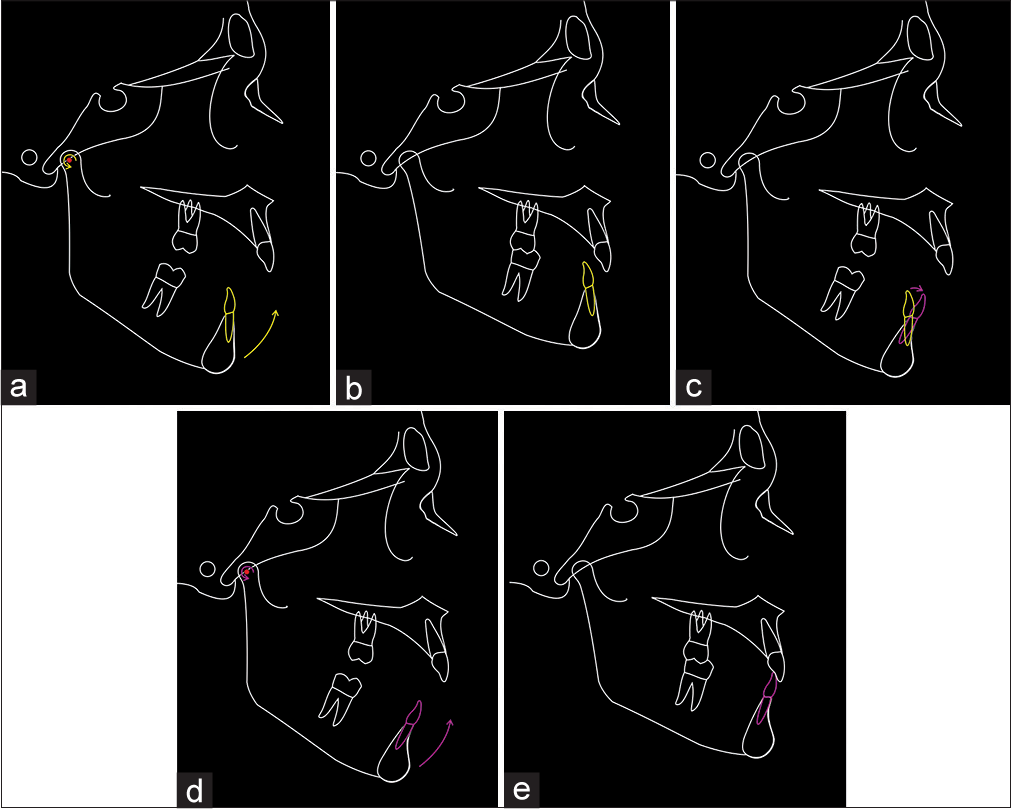
- Mandibular incisor inclination preparation for mandibular autorotation. (a) If the mandibular incisor inclination is not orthodontically prepared before forward mandibular autorotation, then (b) the incisor inclination will be incorrect following autorotation. (c) The mandibular incisor inclination has been orthodontically prepared (in this case by proclination). In this situation, the mandibular incisors may appear excessively proclined, but clinicians should be aware that this is their planned position. (d) With forward autorotation of the mandible, (e) the mandibular incisor inclination will be correct. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Planning the sagittal position of the mandible and chin
Finally, the autorotated sagittal position of the mandible and chin need to be considered, in addition to the dental-occlusal relationship. In the autorotated position, if the mandible is in a good sagittal position and the dental occlusion is acceptable, either no mandibular surgery or perhaps a relieving bilateral sagittal split osteotomy only will be required. Alternatively, the body of the mandible may need to be advanced or set-back in the sagittal plane to improve the facial aesthetic appearance and/or dental occlusion. Advancement or reduction genioplasty may also need to be considered depending on the morphology and prominence of the soft tissue chin and the morphology of the mentolabial fold. This may need to be considered as a secondary procedure.
The pterygomasseteric sling
Elongation of the mandibular ramus against the pterygomasseteric investing tissues (the so-called “pterygomasseteric sling”), in particular, the masseter and medial pterygoid muscles, should usually be avoided, due to the potentially high risk of postoperative relapse. Any rotation of the mandibular body around a pivot in the mandibular second or third molar region, downward posteriorly and upward anteriorly, may vertically stretch the musculofascial sling, the relapse of which leads to reoccurrence of an AOB. Mild AOBs (perhaps up to 4 mm, in the absence of excessive occlusal plane inclination) may be treated with such a rotation following a bilateral sagittal split osteotomy with rigid internal fixation, as long as certain precautions are taken.[7]
Orthodontic Preparation
Preparatory orthodontics has been described in detail elsewhere.[25] However, there are a number of specific points to consider in preparation for differential posterior maxillary impaction and subsequent mandibular autorotation.
Incisor inclination preparation
In preparation for maxillary posterior impaction and forward mandibular autorotation, the incisor teeth will need to be proclined to the appropriate extent, such that their inclinations will correct with the surgery, to achieve ideal incisor inclinations and an ideal interincisal angle after surgery.
Accurate planning will require careful clinical evaluation, cephalometric planning and model surgery to confirm the degree of desired movements. However, an approximate rule of thumb, which may aid preliminary chair side treatment planning, based on the formula already described above, and assuming an approximately average maxillary length, is that 1 mm posterior impaction leads to approximately 1.5° of maxillary incisor retroclination.[23]
Subsequently, the degree of required incisor proclination is calculated more accurately with pretreatment cephalometric planning, using a Ballard-type conversion [Figure 17]. With preadjusted edgewise bracket systems, much of the proclination of the incisors occurs due to the mesial angulation or “tip” in the canine brackets. This needs to be carefully controlled to obtain the desired preoperative incisor inclination.
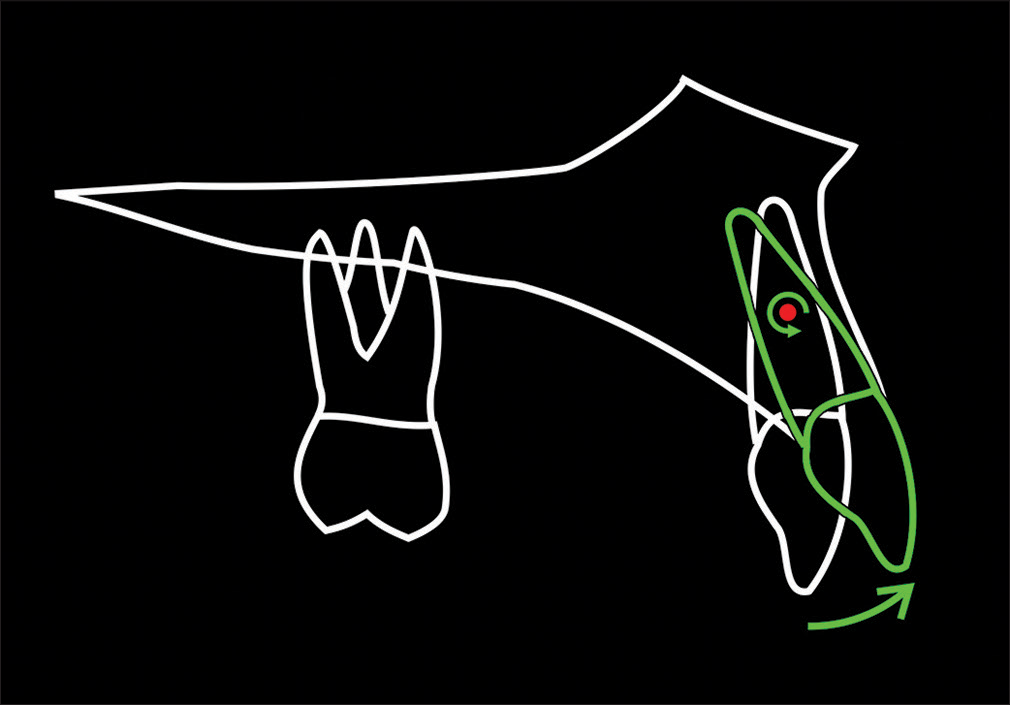
- Calculating the degree of required incisor proclination with pretreatment cephalometric planning, using a Ballard-type conversion. The incisor is rotated around the root centroid (center of rotation), located approximately one-half of the root length from the apex. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Leveling of the arches
There are three potential scenarios, based on the presenting features and thereby presumed etiology of the AOB.
Predominantly skeletal etiology with mild adaptive soft-tissue etiology
In the ideal situation, both the maxillary and mandibular occlusal planes will be leveled (flattened) in the preparatory orthodontic phase of treatment. Therefore, the maxillary posterior impaction will permit forward mandibular autorotation and a relatively good dental occlusion. This is possible if a predominantly skeletal AOB has some adaptive soft-tissue (tongue) etiology, which permits a small degree of maxillary incisor extrusion and thereby arch leveling preoperatively, without a risk of posttreatment relapse [Figure 18].
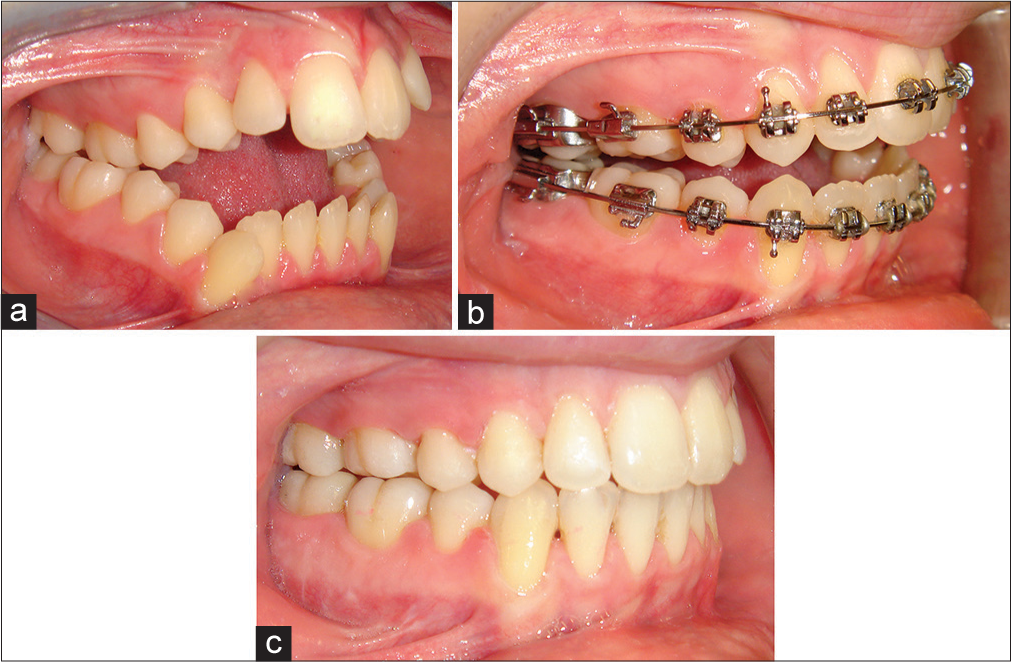
- Example demonstrating preoperative leveling (flattening) of the maxillary and mandibular dental arches. (a) Pretreatment view (b) Preoperative view (c) End of treatment view
Combined skeletal and soft tissue etiology
Alternatively, if there is a marked increased sagittal curve in the maxillary arch, it may be prudent to maintain the accentuated curve in the maxillary arch by placing a curve in the archwire though this will inevitably lead to a postoperative posterior open bite [Figure 19]. In such cases, preoperative orthodontic leveling of the maxillary arch may lead to excessive extrusion of the maxillary incisors, producing a relapse tendency. Relapse of the maxillary incisors in an apical direction when the orthodontic appliances are removed will tend to reopen the bite anteriorly. The alternative is to align and level the anterior and posterior segments independently and undertake segmental posterior impaction of the maxilla.
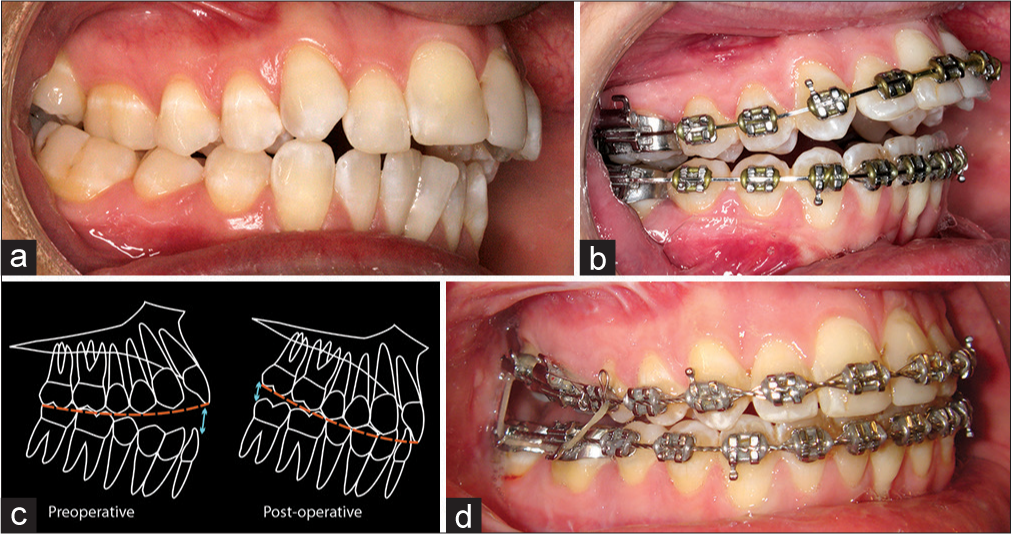
- (a) Pretreatment view, demonstrating an increased sagittal occlusal curve in the maxillary arch. (b) Preoperative view, demonstrating maintenance of the sagittal curve using an accentuated curve in the maxillary archwire. (c) Closure of the anterior open bite will result in a posterior open bite. (d) Postoperative view, demonstrating closure of the anterior open bite, but resultant posterior open bite. Flexible rectangular archwires may be placed, and posterior box elastics used to extrude the posterior maxillary molars and the level the arch. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Predominantly skeletal etiology
In a patient with a skeletal open bite without a soft-tissue element, there will often be an accentuated curve of Spee in the mandibular dental arch and a reverse curve in the maxillary arch. This is due to the incisors having erupted as far as possible in the unsuccessful attempt to meet the opposing incisors, compensating for an increased LAFH. In such cases, leveling of the dental arches should occur by some degree of intrusion of the incisor teeth. The postoperative relapse tendency of the intruded incisors will be for occlusal eruption, which will help to maintain the corrected incisor overbite.
Maxillary occlusal plane inclination and the smile curvature
The smile curvature, alternatively termed the smile arc, may be defined as the relationship of the curvature of the incisal edges of the maxillary anterior dentition (incisal edge curvature) to the curvature of the upper border contour of the lower lip (lower lip curvature) in a posed smile.[26] Differential posterior impaction of the maxilla following a Le Fort I osteotomy, which elevates the posterior maxilla relative to the anterior maxilla and thereby increasing the inclination of the maxillary occlusal plane, will tend to improve the smile curvature (smile arc) relationship [Figure 20].

- (a) Preoperative view, demonstrating a flat smile curvature (smile arc) relationship. (b) Following differential posterior impaction of the maxilla and the increase in the maxillary occlusal plane inclination, there is an improved smile arc relationship. (From: Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017; used with permission)
Transverse maxillary deficiency
In patients with a skeletal AOB, the tongue will often have a low position in the floor of the mouth, away from the palatal vault, which may exacerbate an already narrow maxilla. No more than approximately 4–5 mm of orthodontic maxillary arch expansion is possible without buccal flaring of the molar teeth and resultant postoperative occlusal problems, together with a relapse tendency of the expansion. As such, the pretreatment dental models may be hand articulated in a Class I occlusion to evaluate the approximate amount of maxillary expansion required, and consideration should be given to either preliminary surgically assisted rapid maxillary expansion, or alternatively a segmental approach to the maxillary surgery with concomitant expansion of the posterior segments, if significant maxillary expansion is required.
Surgical Technique
Le Fort I osteotomy of the maxilla and the step-by-step surgical technique of differential posterior impaction have been described in detail elsewhere.[1,27] The maxilla is exposed by the standard sublabial vestibular incision and subperiosteal dissection. A saw cut is made at the Le Fort I level from the zygomatic buttress forward to the piriform aperture. A back cut is then made from the buttress in a posterior direction to the pterygomaxillary fissure. In accordance with the preoperative planning, marks are made above this osteotomy line at the buttress and the piriform rim, which indicate the position of the upper osteotomy cut, and therefore, the amount of bone to be removed in the vertical dimension posteriorly and anteriorly [Figure 21]. Differential posterior impaction of the maxilla requires the removal of a tapering bone strip of appropriate width, greater posteriorly than anteriorly.
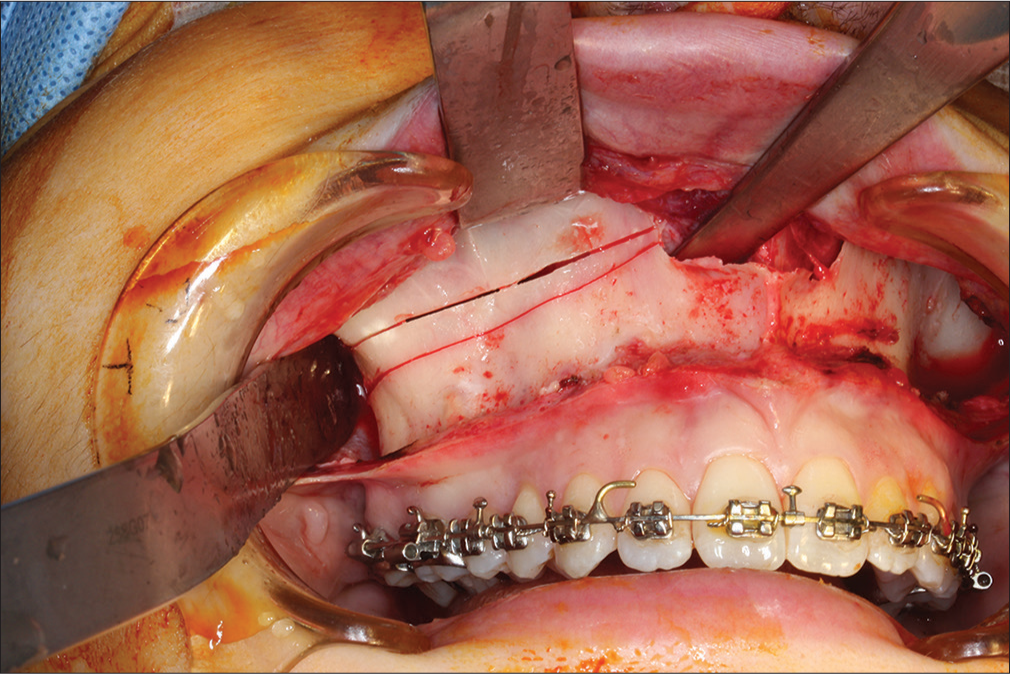
- The osteotomies are made such that removal of a tapering bone strip of appropriate width, greater posteriorly than anteriorly, will result in differential posterior impaction of the maxilla
Postoperative Orthodontics
Postoperative orthodontics has been described in detail elsewhere.[25] If the dental arches have been leveled (flattened) preoperatively, the dental occlusion should be relatively acceptable postoperatively, with only minor occlusal settling and finishing required. If an accentuated sagittal occlusal curve has been maintained in the maxillary dental arch and rectangular stainless steel archwire, there is likely to be an element of posterior open bite present postoperatively. The maxillary archwire should be replaced with a more flexible flat archwire (usually a rectangular braided stainless steel archwire), and posterior box elastics used to gradually extrude the posterior maxillary molars into occlusion.
If maxillary expansion has been achieved either preoperatively or intraoperatively, the expansion will need to be maintained in the postoperative period. A large dimension stainless steel maxillary archwire with some expansion is often enough though an auxiliary expanded archwire may be placed in the headgear tubes and overtied. On debonding of the appliances, a modified Hawley retainer with a midline expansion screw may be used, allowing some activation of expansion should this become necessary in the retention phase of treatment.
Conclusion
A significant AOB may be a significant functional and aesthetic concern for patients. The usual multifactorial etiology and range of relevant diagnostic factors and treatment planning concerns, as well as the diversity of surgical options available and potential long-term considerations regarding stability, make this one of the most challenging dentofacial deformities to treat. Inappropriate treatment will result in a compromised dentofacial aesthetic outcome and potentially a tendency to relapse to the pretreatment situation.
Further Reading
Naini FB, Gill DS, editors. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Surgical correction of anterior open bite: Differential posterior maxillary impaction In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Facial type In: Naini FB, ed. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
- [Google Scholar]
- The maxilla and midface In: Naini FB, ed. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
- [Google Scholar]
- Orthognathic surgery: Preliminary consideration In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Surgical correction of skeletal anterior open bite: Segmental maxillary surgery In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Surgical treatment of anterior open bite with mandibular osteotomies In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1-132.
- [Google Scholar]
- Effects of adenoidectomy on mode of breathing, size of adenoids and nasal airflow. ORL J Otorhinolaryngol Relat Spec. 1973;35:283-302.
- [CrossRef] [PubMed] [Google Scholar]
- “The relation between nasorespiratory function and dentofacial morphology”. Am J Orthod. 1983;83:443-4.
- [Google Scholar]
- Posture of the head, the hyoid bone, and the tongue in children with and without enlarged tonsils. Eur J Orthod. 1990;12:458-67.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular and maxillary growth after changed mode of breathing. Am J Orthod Dentofacial Orthop. 1991;100:1-18.
- [Google Scholar]
- Nasal obstruction and facial growth: The strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop. 1998;113:603-11.
- [CrossRef] [Google Scholar]
- Risk factors for post-orthognathic condylar resorption: A review. World J Orthod. 2008;9:21-5.
- [Google Scholar]
- Cephalometry and cephalometric analysis In: Naini FB, ed. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
- [Google Scholar]
- The face in profile: An anthropological X-ray investigation on Swedish children and conscripts. Sven Tandlak Tidskr. 1947;40(5B)
- [Google Scholar]
- A cephalometric investigation of skeletal factors in anterior open bite and deep overbite. Rep Congr Eur Orthod Soc. :159-71.
- [Google Scholar]
- Regional aesthetic analysis: The nose In: Naini FB, ed. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
- [Google Scholar]
- The aesthetic impact of upper lip inclination in orthodontics and orthognathic surgery. Eur J Orthod. 2015;37:81-6.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between maxillary length, differential maxillary impaction, and the change in maxillary incisor inclination. Am J Orthod Dentofacial Orthop. 2003;124:526-9.
- [Google Scholar]
- Principles of orthognathic treatment planning In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Preparatory and postoperative orthodontics: Principles, techniques and mechanics In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]
- Smile aesthetics In: Naini FB, ed. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell; 2011.
- [Google Scholar]
- Le Fort I osteotomy and maxillary advancement In: Naini FB, Gill DS, eds. Orthognathic Surgery: Principles, Planning and Practice. Oxford: Wiley-Blackwell; 2017.
- [Google Scholar]






