Translate this page into:
The effect of various oral hygiene products on the microbial flora in patients undergoing orthodontic treatment
Address for correspondence: Dr. Preeti Chauhan, 433, Nangla Battu Road, Prabhat Nagar, Meerut, Uttar Pradesh, India. E-mail: drpreetichauhan@gmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context
Orthodontic devices lead to significantly greater plaque accumulation and gingival inflammation resulting in a change of gingival flora from cocci and rods to motile organisms like spirochetes.
Aims
The aim was to study the effect of various oral hygiene products on the microbial flora in patients undergoing orthodontic treatment.
Materials and Methods
The microbial composition of 40 patients, divided into four groups of 10 patients each, was evaluated. Group I patients were prescribed nonfluoridated dentifrice which act as the control group, Group II patients were given fluoridated dentifrice while in Group III and Group IV fluoridated mouth rinse and cetylpyridinium chloride mouth rinse, respectively, along with nonfluoridated toothpaste was prescribed. The plaque sample was collected at the start of orthodontic treatment, after 30 days, 60 days and 90 days for all the patients. The microscopic slides were prepared and observed under dark field microscopy at the magnification of ×1000 and microbes were classified as cocci, spirochetes, fusiforms, filaments, and rods.
Results
After applying analysis of variance and Tukey honest significant difference test, it was observed that after 30 days, only the proportion of filaments was found to be significantly higher in Group I. After 60 days, Group I had significantly lower proportion of cocci and a higher proportion of rods as compared to other groups. After 90 days, Group I had significantly higher count of rods, filaments, fusiforms, and spirochetes as compared to Groups III and IV.
Conclusion
Less amount of the microbial shift to the pathogenic organisms was seen in the patients in whom mouthwashes along with tooth brushing were prescribed.
Keywords
Cetyl pyridinium chloride mouthwash
cocci
filaments
fluoridated mouthwash
fluoridated toothpaste
fusiforms
nonfluoridated toothpaste
rods
spirochetes
INTRODUCTION
Orthodontic devices on the buccal and lingual surfaces of teeth upset the deflective role of the gingiva.[1] Banded patients have greater plaque accumulation and gingival inflammation.[2]
In healthy gingival crevice, flora consists mostly of Gram-positive facultative anaerobic cocci and rods.[3] Progress to destructive periodontitis leads to increase in Gram-negative facultative anaerobes and motile organisms like spirochetes.[4] Current chemotherapeutic approaches oral hygiene aim to modify the oral microflora to promote healthy tissues.
This study is carried out to determine whether these products aid in maintaining better oral hygiene as compared to the regular methods in orthodontic patients undergoing fixed mechanotherapy.
MATERIALS AND METHODS
Ethics
The study is ethically approved by Institutional Ethical Committee, Maharishi Markandeshwar University, Mullana, Ambala as Project No: IEC-77.
Forty subjects with different types of malocclusion requiring fixed orthodontic treatment were chosen among the patients.
The inclusion criteria were:
All the patients had malocclusion which requires fixed mechanotherapy
All the subjects were in good health and had not been prescribed any antibiotics during the 3 months preceding the study.
The patients were randomly selected into four groups (10 patients each) Table 1:
Brand name: Colgate Palmolive India Ltd in Gurgaon, Delhi.
At the beginning of the study, each patient was given full mouth prophylaxis and was instructed in the modified bass brushing technique.
A sterilized periodontal curette was introduced through the sulcus or pocket orifice as far apically as possible, and the bacterial contents were removed from the facial surface of maxillary molars [Figures 1 and 2]. Plaque samples were processed for dark field examination according to the method of Listgarten and Hellden.[5]

- Periodontal curette introduced through the sulcus or pocket orifice before the start of orthodontic treatment

- Periodontal curette introduced through the sulcus or pocket orifice during orthodontic treatment
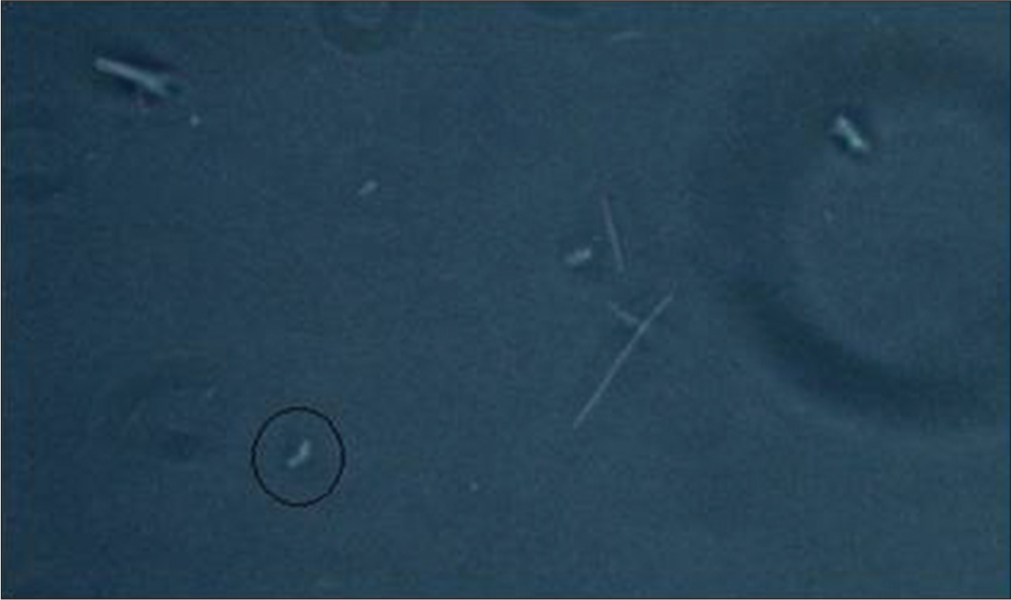
The sample, immediately after removal, was suspended in a sterile 0.85% sodium chloride solution containing 1% gelatin by vigorously agitating the tip of the instrument in the solution. Bacterial sample was dispersed in 0.1-0.3 ml of solution obtained from single surfaces. In order to minimize clumping and the loss of bacterial motility, sample was prepared, and the examination was completed within 1-2 h of their collection. The bacterial suspension was dispersed just prior to the examination by aspirating and expelling the fluid three times through a disposable tuberculin syringe equipped with a 23-gauge needle. Special care was taken to avoid excessive bubbling of air during the dispersion. One drop of the suspension was applied to a microscopic slide, and coverslipped. The slide was examined by dark field microscopy at a magnification of ×1000 under oil immersion of Nikon 80i Eclipse microscope. The bacteria were observed and classified on a morphologic basis as cocci [Figure 3], spirochetes [Figure 4], fusiforms [Figure 5], filaments [Figure 6], and rods [Figure 7]. Hundred bacteria from fields selected at random were classified into five morphological categories.[5]
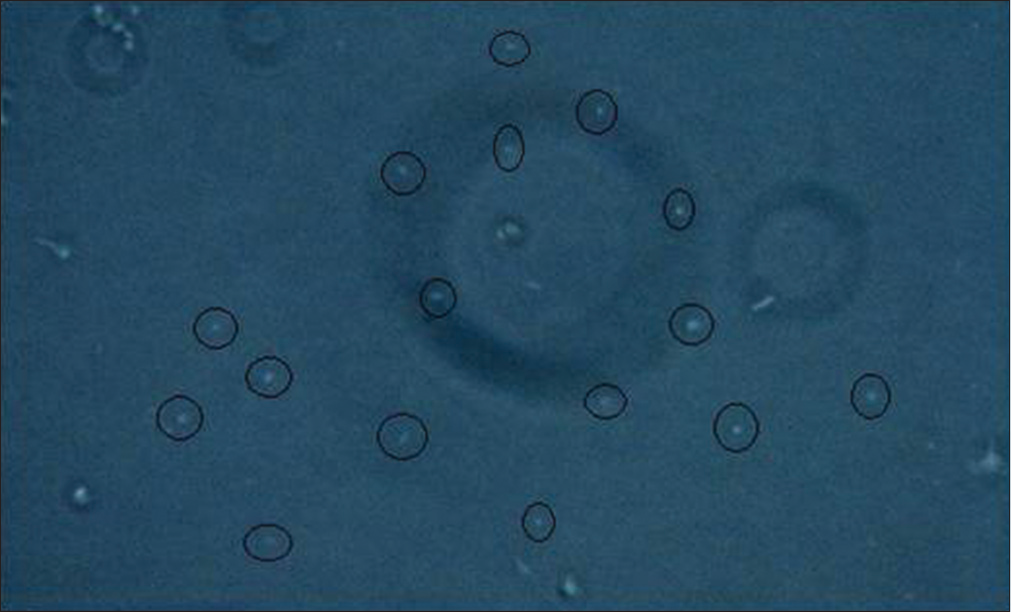
- Dark field microscopic view (at ×1000) coccoid cells
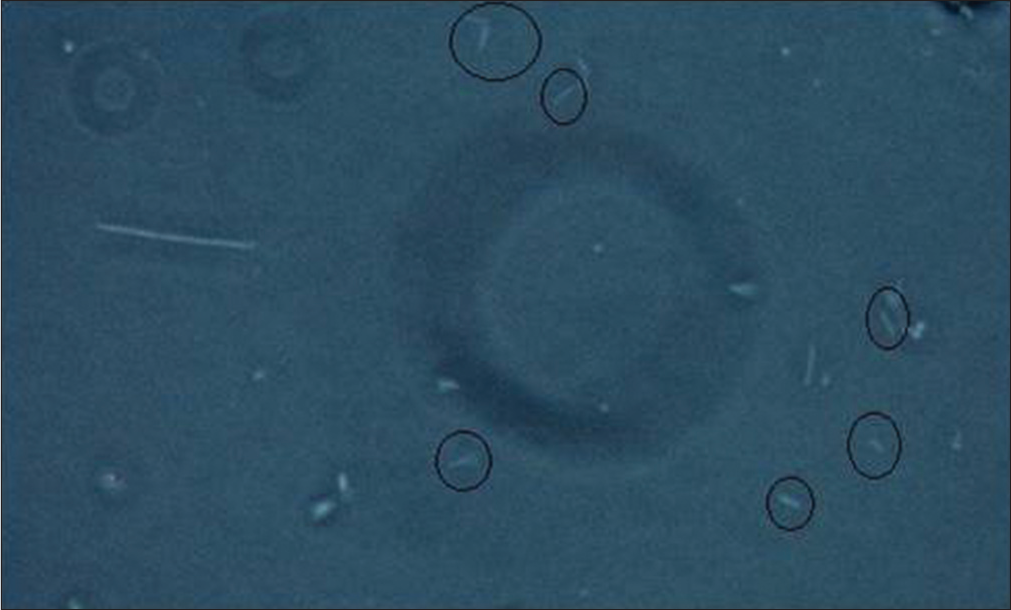
- Dark field microscopic view (at ×1000) rods
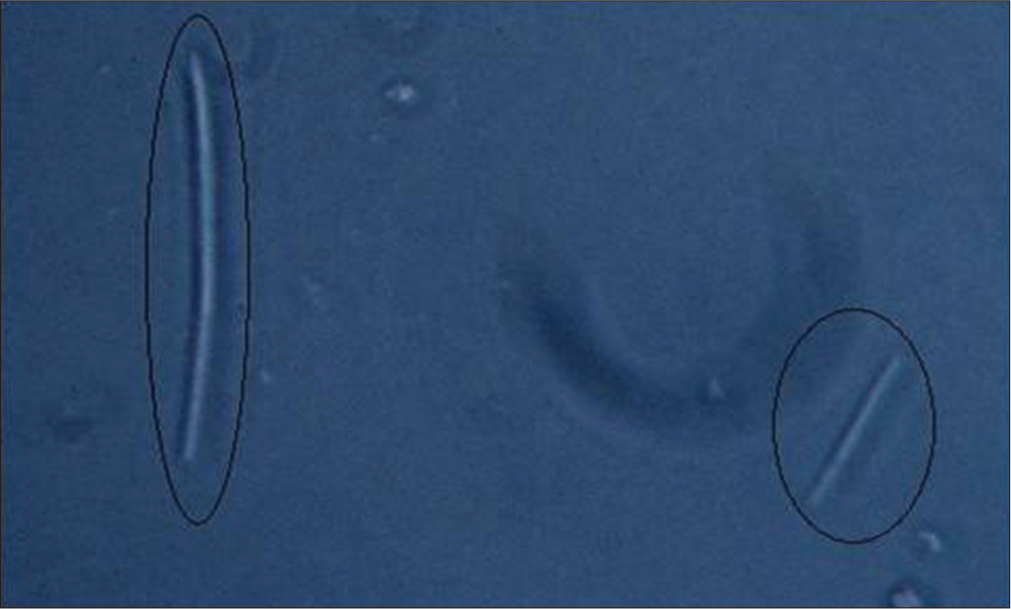
- Dark field microscopic view (at ×1000) filaments
- Dark field microscopic view (at ×1000) fusiforms

- Dark field microscopic view (at ×1000) spirochetes
After baseline examination, the orthodontic treatment was initiated. Fixed appliance was placed on the teeth. Bacteriologic dark field examination was carried out at 30, 60, and 90 days interval after the beginning of orthodontic treatment in all the groups.
The statistical analysis was done using Statistical Package for Social Sciences Version 15.0 statistical analysis software manufactured by SPSS Inc., 233 South Walker Drive, Chicago in 2006.
RESULTS
| Group | Oral hygiene products used | Sample size |
|---|---|---|
| Group I (control group) | Nonfl uoridated toothpaste (Colgate Super Shakti Dental Cream) | 10 |
| Group II | Fluoridated toothpaste (Colgate Total toothpaste (triclosan 0.3% w/w, sodium fl uoride EP 0.32% w/w (1450 ppm F))) | 10 |
| Group III | Nonfl uoridated toothpaste with fl uoridated mouthwash (Colgate Phos-Flur mouthwash (sodium fl uoride 0.044% w/v)) | 10 |
| Group IV | Nonfl uoridated toothpaste with CPC mouthwash (Colgate Plax mouthwash (CPC 0.05% w/w)) | 10 |
CPC - Cetyl pyridinium chloride
At the start of the treatment, the plaque sample was taken and observed under dark field microscopy. The mean microbial profile of the patients enrolled in different groups was analyzed [Table 2].
After 30 days, the mean microbial profile of patients in different groups showed that cocci comprised the maximum proportion in all the groups with the mean value of 80.30 ± 9.25 in Group I, 83.90 ± 3.70 in Group II, 86.00 ± 7.18 in Group III, and 86.10 ± 3.57 in Group IV followed by rods which had maximum mean value of 14.30 ± 14.85 in Group I and minimum value of 8.70 ± 4.32 in Group III then were filaments which had minimum count of 3.90 ± 1.20 in Group IV and maximum of 6.70 ± 2.45 in Group I. Fusiforms and spirochetes comprised of the minimum proportion of 0.00 ± 0.00 and 0.20 ± 0.42 in Group IV, respectively. After applying Tukey honest significant difference (HSD) test, it was observed that except for difference between Group I and IV for proportion of filaments (P < 0.05), none of the between group differences were found to be significant statistically. The proportion of filaments was found to be significantly higher in Group I as compared to Group IV (P < 0.05).
At day 60, the comparison of mean value for microbial profile of patients in different groups showed that although cocci comprised of the maximum proportion (64.10 ± 17.85 in Group I, 76.50 ± 5.28 in Group II, 84.10 ± 6.14 in Group III, and 84.50 ± 4.50 in Group IV) in all the groups followed by fusiforms (1.80 ± 1.99 in Group I, 0.60 ± 0.84 in Group II, 0.70 ± 0.95 in Group III, and 0.40 ± 0.52 in Group IV) while spirochetes (2.30 ± 1.77 in Group I, 1.70 ± 1.34 in Group II, 1.50 ± 1.43 in Group III, and 1.20 ± 1.14 in Group IV) comprised the minimum proportion.
Tukey HSD test showed that Group I (P < 0.05) had significantly lower proportion of cocci as compared to Group II and very highly significant lower proportion of cocci as compared to Group III and Group IV (P < 0.001). Group I had significantly higher proportion of rods as compared to Groups III and IV (P < 0.05) and highly significant higher proportion of filaments as compared to Groups III and IV (P < 0.001). None of the other differences were significant statistically.
| Microbe | Group I | Group II | Group III | Group IV | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Cocci | 91.70 | 4.62 | 89.10 | 3.31 | 89.20 | 3.58 | 89.40 | 2.01 |
| Rods | 5.10 | 2.42 | 7.90 | 2.51 | 7.10 | 2.60 | 8.00 | 2.16 |
| Filaments | 3.00 | 1.49 | 2.90 | 1.91 | 3.10 | 1.37 | 2.40 | 1.58 |
| Fusiforms | 0.50 | 1.27 | 0.00 | 0.00 | 0.20 | 0.63 | 0.00 | 0.00 |
| Spirochetes | 0.30 | 0.95 | 0.10 | 0.32 | 0.40 | 0.70 | 0.20 | 0.42 |
SD - Standard deviation
| Micobes at day 90 | Sum of squares | Df | Mean square | F | Signifi cant |
|---|---|---|---|---|---|
| Cocci 90 | |||||
| Between groups | 4539.400 | 3 | 1513.133 | 16.948 | <0.001 |
| Within groups | 3214.200 | 36 | 89.283 | ||
| Total | 7753.600 | 39 | |||
| Rods 90 | |||||
| Between groups | 1010.200 | 3 | 336.733 | 11.552 | <0.001 |
| Within groups | 1049.400 | 36 | 29.150 | ||
| Total | 2059.600 | 39 | |||
| Filaments 90 | |||||
| Between groups | 742.475 | 3 | 247.492 | 10.446 | <0.001 |
| Within groups | 852.900 | 36 | 23.692 | ||
| Total | 1595.375 | 39 | |||
| Fusiforms 90 | |||||
| Between groups | 25.875 | 3 | 8.625 | 8.193 | <0.001 |
| Within groups | 37.900 | 36 | 1.053 | ||
| Total | 63.775 | 39 | |||
| Spirochetes 90 | |||||
| Between groups | 47.000 | 3 | 15.667 | 9.625 | <0.001 |
| Within groups | 58.600 | 36 | 1.628 | ||
| Total | 105.600 | 39 | |||
The mean values for microbial profile of patients in different groups at day 90 showed that cocci count was maximum in Group III (81.80 ± 7.28) and minimum in Group I (55.70 ± 15.36). Rods were maximum in Group I (22.60 ± 9.14) and minimum in Group III (10.10 ± 4.31). Filaments were also maximum in Group I (15.20 ± 7.98) and minimum in Group IV (0.60 ± 0.70) while count of fusiforms and spirochetes was also maximum in Group I (2.50 ± 1.35 and 3.80 ± 1.03, respectively). Count of fusiforms was minimum in Group IV (0.60 ± 0.70) whereas count of spirochetes was minimum in Group III (1.20 ± 1.23).
The Tukey HSD test also showed that cocci are very highly significant in Group I as compared to Group III and Group IV (P < 0.001). Group II has significantly less proportion of cocci as compared to Group I (P < 0.05) and significantly more proportion as compared to Group III and Group IV (P < 0.05) Figure 8. For rods, Group I had significantly higher count as compared to Group II (P < 0.01) and highly significant higher count as compared to Groups III and IV (P < 0.001) Figure 9. The proportion of filaments was significantly higher in Groups I and II. Group I had very highly significant values of filaments as compared to Groups III and IV (P < 0.001). Group II also had significantly higher count of filaments as compared to Groups III and IV (P < 0.05) Figure 10.
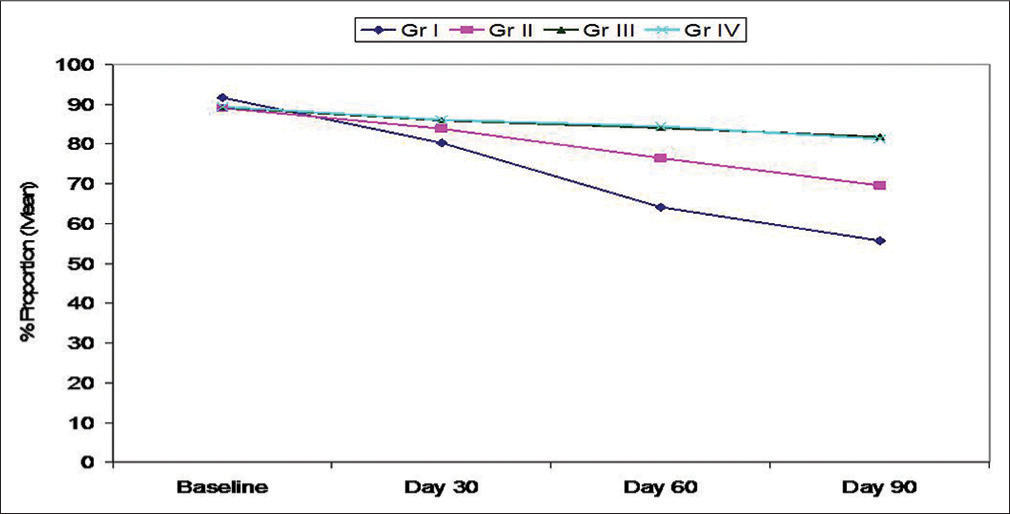
- Pattern of change in proportion of cocci at different follow-up intervals
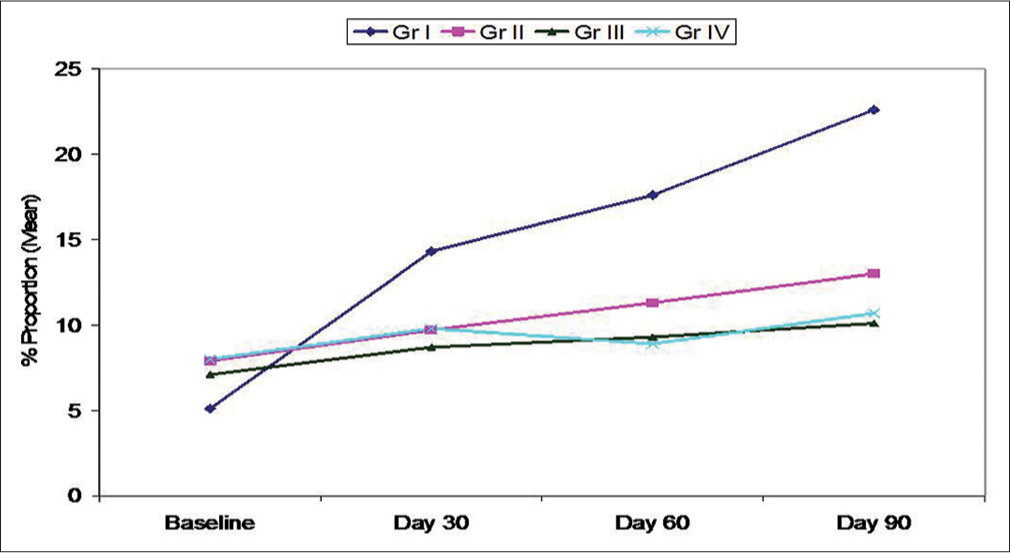
- Pattern of change in proportion of rods at different follow-up intervals
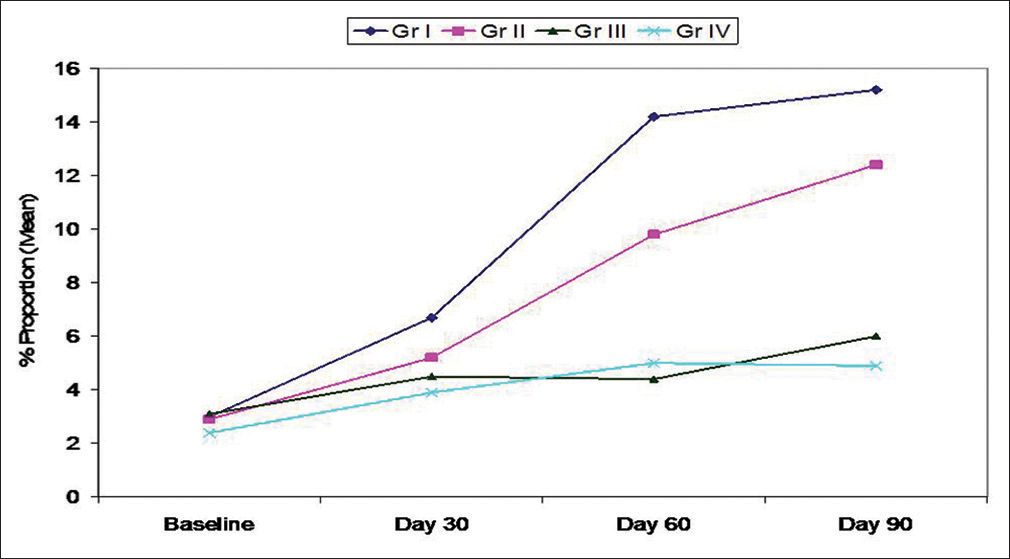
- Pattern of change in proportion of filaments at different follow-up intervals
For fusiforms, Group I had significantly higher count as compared to Groups III and IV (P < 0.05) while Group II had significantly higher count as compared to Group IV (P < 0.05) Figure 11. The proportion of spirochetes was significantly higher in Groups I and II as compared to Groups III and IV (P < 0.05). Group I had highly significant difference in spirochetes count as compared to Groups III and IV (P < 0.01 Figure 12) [Table 3].
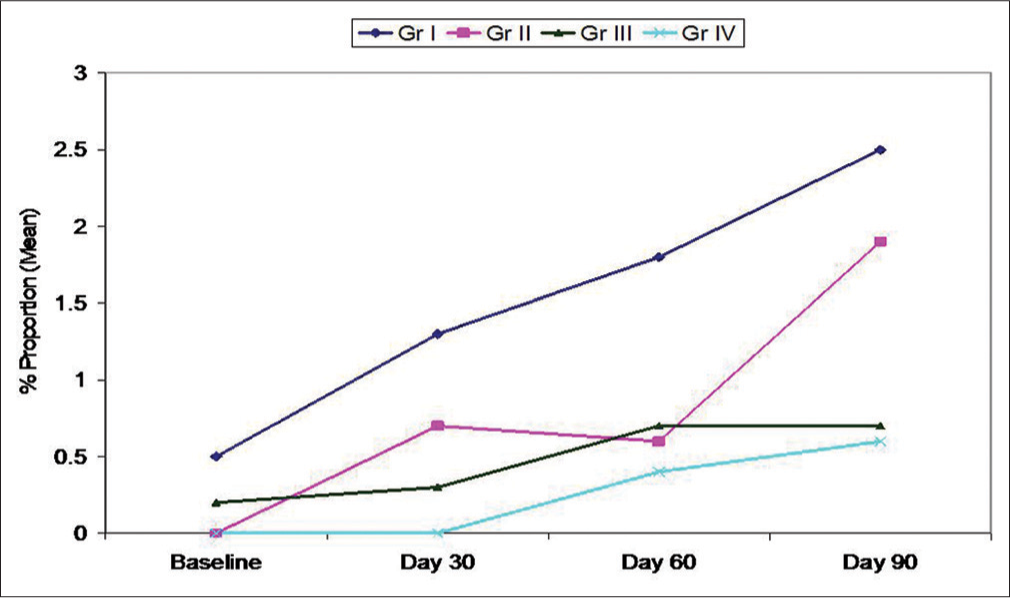
- Pattern of change in proportion of fusiforms at different follow-up intervals
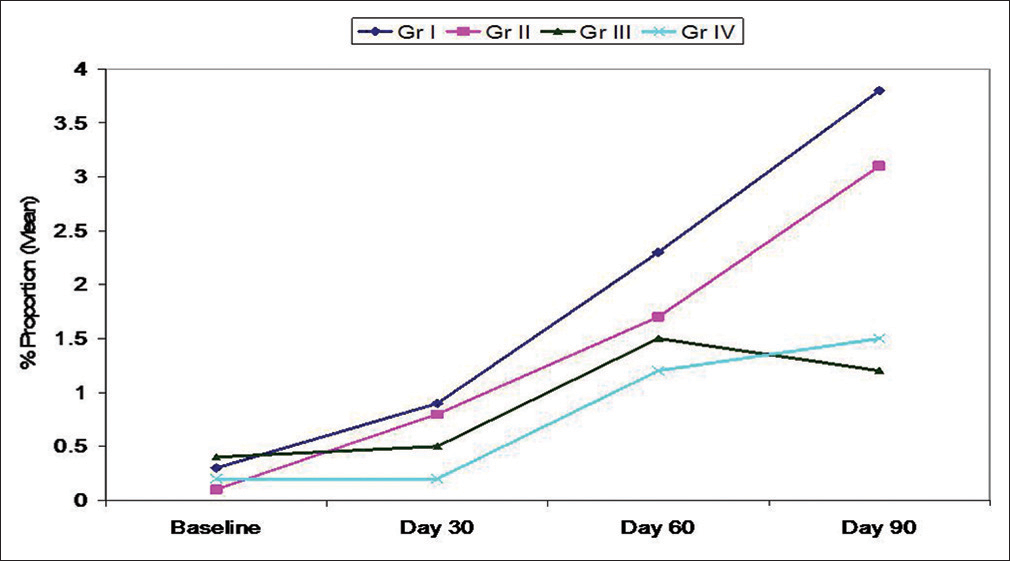
- Pattern of change in proportion of spirochetes at different follow-up intervals
DISCUSSION
Orthodontic treatment with fixed appliances alters the oral environment, increases the plaque amount, changes the composition of the flora, and complicates the cleaning for the patient. Gingivitis and enamel decalcification around fixed appliances are frequent side effects when preventive measures have not been implemented.[20,21,24]
Kim et al. find that the placement of orthodontic appliances affects the subgingival microbial composition, increasing the prevalence of periodontopathogens, especially in the molar region.[6] Corbett et al. and Balenseifen et al. also found significantly higher levels of Streptococcus mutans in banded orthodontic patients with an increase of plaque pH, carbohydrate content, and microbial populations.[7,8] There are many studies which also showed the detrimental effects of plaque accumulation around orthodontic brackets and bands leading to change in microbial flora. Therefore, an effective oral hygiene is essential for patients undergoing orthodontic treatment. The various oral hygiene methods used by the dentists are brushing, flossing, and mouth rinsing.[3,4,9-13]
A healthy periodontium appears to be associated with scant microbial flora located almost entirely supragingivally and are comprised mainly of Gram-positive coccal forms. Progress to destructive periodontitis coincides with the dominance of the Gram-negative facultative anaerobes and the presence of increasing numbers of motile organisms such as spirochetes and filaments.[4]
The current study was designed to test the efficacy of different oral hygiene products commonly used by the orthodontists to improve the oral health of their patients with fixed mechanotherapy. All the patients in this study, when analyzed had a similar kind of microbial profile which comprised of the maximum proportion of cocci (mean proportion 89-91%) followed by rods (mean proportion 5-8%) then filaments (mean proportion 2.4-3%). Fusiforms and spirochetes comprised of the minimum percentage of 0-0.5%.
In the study done by Listgarten and Hellden in 1978, the coccoid cells were more predominant at normal sites (74.3% vs. 22.3%), while at diseased sites motile rods were more frequent (12.7% vs. 0.3%), as well as curved rods (7% vs. 0%), small spirochetes (12.6% vs. 1.1%), medium-sized spirochetes (18.5% vs. 0.5%), and large spirochetes (6.7% vs. 0.2%).[5]
In Group II, fluoridated toothpaste was prescribed to maintain oral hygiene of the patients. The presence of fluoride ions causes a disturbance in the bacterial enzyme systems. There was a reduction in the number of cocci from 89.1% to 69.6% at day 90. There was an increase in a number of rods which was 7.9% at the start of the treatment to 9.7% after 30% at day 60 and 13% at day 90. Filaments also increased from 2.9% to 12.4% at day 90. Similar kind of increase was seen in fusiforms which was 0% at the baseline and then increased to 1.9% after 90 days. 0.1% of spirochetes were present at the start of orthodontic treatment which increased to 0.8% at day 30, to 1.7% at day 60, and 3.1% at day 90. The increase seen in the proportion of rods, filaments, fusiforms, and spirochetes was significant statistically (P < 0.01).
The patients in Group III were prescribed a fluoridated mouthwash along with nonfluoridated toothpaste. There was a mild reduction in the number of cocci from 89.2% to 81.8% at day 90. The proportion of rods increased from 7.1% to 8.7% after 30 days, to 9.3% after 60 days and further to 10.1% after 90 days. Filament also increased from 3.1% to 4.5% at day 30, to 6% at day 90. The increase seen in fusiforms and spirochetes was not significant statistically (P > 0.05).
In Group IV, in addition to normal oral hygiene measures with nonfluoridated toothpaste a cetylpyridinium chloride (CPC) mouthwash was prescribed to maintain oral hygiene. CPC is an antimicrobial agent that damages cells by interacting with bacterial membranes.[3] In our study, after using CPC mouthwash there was a shift in the microbial flora which showed a reduction in cocci from 89.4% to 81.3% after 90 days. There was an increase in the count of rods from 8% to 10.7% after 90 days of the start of orthodontic treatment. Filaments also increased from 2.4% to 5% after 60 and 90 days. Similar increase was seen in fusiforms from 0% to 0.6% and spirochetes from 0.2% to 1.5% in 90 days.
Thus, it was seen that there was an overall increase in all organisms except cocci over the period of our study which was highly significant (P < 0.001). Since cocci are considered to be the healthy flora, they showed a decrease in the proportion while the other microbes which are considered to have high pathogenic potential showed a significant increase over a period of 90 days.
Huser et al. found that initially in the test group, that is, in which orthodontic bands were placed, the bacterial flora was composed almost exclusively of cocci. Spirochetes or rods were detected in extremely low numbers. At day 47, after the placement of bands, they observed a significant increase in the percentage of spirochetes, motile rods, filaments, and fusiforms; conversely, noted a decrease in cocci (P < 0.01).[14]
Akande et al. concluded that CPC containing mouthwash reduced oral microbial load counts when used as an adjunct to normal oral hygiene procedures. At the same time, they also suggested that the inhibitory power of CPC on oral microbes is greater than phenol- and triclosan-containing mouthwashes. But according to our results, CPC mouthwash is less effective in controlling the negative microbial shift in dental plaque as compared to fluoride containing mouthwash.[15]
Cummins and Creeth suggested that the clinical efficacy of an antiplaque agent is characterized by a combination of intrinsic antibacterial activity and good oral retention properties.[16] A review done by Domenick T Zero showed that in addition to the inherent properties of a fluoride dentifrice product, biological, and behavioral factors can modify its antiplaque and anticaries effectiveness. The “application” phase and the “retention” phase are the main determining factor s. The fluoride mouth rinses can lead to higher levels of oral fluoride retention than fluoride dentifrice.[17] Charles et al. and Gunsolley had done a comparative study on efficacy of mouth rinse and dentifrice and concluded mouthwash used along with a dentifrice produced a significantly greater benefit in reducing plaque. In this study also mouth rinses, whether fluoridated or CPC mouthwash, along with tooth brushing proved to be more effective as compared to the use of fluoridated toothpaste alone.[18,19,22,23,25]
Looking at the results of our study, we can safely say that the mouth rinses along with good brushing technique with nonfluoridated toothpaste are more effective in maintaining good oral hygiene of the patients. Among the mouth rinses, fluoridated mouth rinse seems to be more effective as compared to the mouth rinse containing CPC.
Therefore, we can conclude that tooth brushing alone is not good enough in maintaining oral hygiene of the patients undergoing orthodontic treatment and a mouthwash need to be prescribed to maintain an effective oral hygiene. Hence, according to our study, fluoride mouthwash with normal oral hygiene measures is the most beneficial for orthodontic patients and it should be prescribed to all the patients to maintain an effective oral hygiene during the course of orthodontic treatment.
References
- Microbiological aspects of the chemical control of plaque and gingivitis. J Dent Res. 1992;71:1431-8.
- [Google Scholar]
- Professional prophylaxis and its effect on the periodontium of full-banded orthodontic patients. Am J Orthod Dentofacial Orthop. 1987;91:321-7.
- [Google Scholar]
- Effects of orthodontic bands on microbiologic and clinical parameters. Am J Orthod Dentofacial Orthop. 1990;97:213-8.
- [Google Scholar]
- Changes in gingiva and gingival flora with bonding and banding. Angle Orthod. 1987;57:271-8.
- [Google Scholar]
- Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J Clin Periodontol. 1978;5:115-32.
- [Google Scholar]
- Microbiologic changes in subgingival plaque before and during the early period of orthodontic treatment. Angle Orthod. 2012;82:254-60.
- [Google Scholar]
- Comparison of Streptococcus mutans concentrations in non-banded and banded orthodontic patients. J Dent Res. 1981;60:1936-42.
- [Google Scholar]
- Plaque, caries level and oral hygiene habits in young patients receiving orthodontic treatment. Community Dent Health. 2010;27:133-8.
- [Google Scholar]
- Periodontal condition in orthodontically treated and untreated individuals. I. Loss of attachment, gingival pocket depth and clinical crown height. Angle Orthod. 1973;43:402-11.
- [Google Scholar]
- The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44:127-34.
- [Google Scholar]
- Studies of fluoride retention by oral soft tissues after the application of home-use topical fluorides. J Dent Res. 1992;71:1546-52.
- [Google Scholar]
- Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;100:35-7.
- [Google Scholar]
- Efficacy of an alcohol-free CPC-containing mouthwash against oral multispecies biofilms. J Clin Dent. 2011;22:187-94.
- [Google Scholar]
- Efficacy of different brands of mouth rinses on oral bacterial load count in healthy adults. Afr J Biomed Res. 2004;7:125-8.
- [Google Scholar]
- Delivery of antiplaque agents from dentifrices, gels, and mouthwashes. J Dent Res. 1992;71:1439-49.
- [Google Scholar]
- Dentifrices, mouthwashes, and remineralization/caries arrestment strategies. BMC Oral Health. 2006;6(1):S9.
- [Google Scholar]
- Comparative efficacy of an antiseptic mouthrinse and an antiplaque/antigingivitis dentifrice. A six-month clinical trial. J Am Dent Assoc. 2001;132:670-5.
- [Google Scholar]
- A meta-analysis of six-month studies of antiplaque and antigingivitis agents. J Am Dent Assoc. 2006;137:1649-57.
- [Google Scholar]
- Does oral health counseling effectively improve oral hygiene of orthodontic patients. European Journal of Pediatric Dentistry. 2012;13:181-6.
- [Google Scholar]
- effect of three different motivational techniques on oral hygiene and gingival health of patients undergoing multibracketed orthodontics. The Angle Orthodontist. 2011;81:884-8.
- [Google Scholar]
- Effects of combined application of antimicrobial and fluoride varnishes in orthodontic patients. Am J Orthod Dentofacial Orthop. 2001;120:28-35.
- [Google Scholar]
- Effectiveness of an Essential Oil Mouthrinse in improving oral health in orthodontic patients. Angle Orthod. 2008;78:294-8.
- [Google Scholar]
- Appropiate oral hygiene motivation method for patients with fixed appliances. Angle Orthod. 2007;77:1085-9.
- [Google Scholar]
- Interspace/interdental brushes for oral hygiene in orthodontic patients with fixed appliances. Cochrane Database of Systemic Reviews (3)
- [Google Scholar]






