Translate this page into:
What is the most effective technique and composite for bonding aligner attachments to primary enamel?

*Corresponding author: Serpil Çokakoğlu, Department of Orthodontics, Pamukkale University, Faculty of Dentistry, Denizli, Turkey. serpilcokakoglu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Çokakoğlu S, Nalçacı R, Tozlu M, Altıntaş SH. What is the most effective technique and composite for bonding aligner attachments to primary enamel? APOS Trends Orthod. 2024;14:35-41. doi: 10.25259/APOS_57_2023
Abstract
Objectives:
This in vitro study evaluated the shear bond strength (SBS) of aligner attachments bonded to primary teeth with different techniques and composites.
Material and Methods:
Eighty attachments were prepared using five composites: An aligner composite (GC aligner connect [GAC]), two flowable restorative composites (G-aenial universal injectable and Estelite universal super low flow), and two one-step orthodontic composites integrated with primer (GC ortho connect flow and GC ortho connect). Aligner and restorative composites were applied with self- or total-etch (SE or TE) modes of universal adhesive (G-Premio Bond). Self-adhering composites integrated with primer were applied after acid etching. Excessive composites were removed with tungsten carbide burs after the polymerization of resin attachments. All primary teeth were exposed to thermocycling. Bond strength was determined with a universal testing machine. Remnant resin attachment was scored with the resin attachment remnant index. Kruskal–Wallis, Mann–Whitney, and Chi-square tests were used for statistical analyses.
Results:
The self-etching technique demonstrated lower SBS values compared to total-etching and self-adhering groups regardless of composite type. The highest SBS was found with aligner composite (GAC) and the total-etching technique. Self-adhering composites showed sufficiently high SBS values comparable with GAC and TE bonding techniques. The amount of remnant attachment was significantly higher in the total-etching and self-adhering groups compared to SE bonding with GAC (P < 0.05).
Conclusion:
Self-adhering orthodontic composites can be preferred to simplify the bonding of aligner attachments to primary enamel after acid etching.
Keywords
Aligner
Attachment
Bonding
Primary teeth
INTRODUCTION
The increasing popularity of clear aligner treatment (CAT) has led to developments for young patients. In 2019, the Invisalign First clear aligners were launched as innovative orthodontic appliances for children between the ages of 6 and 12 years. When children still have most of their primary teeth, Phase 1 treatment can be an alternative as early as ages 6–10. Phase 2 treatment is usually required when all permanent teeth have erupted. Early interventions with CAT in children focus on problems such as molar rotation, dentoalveolar construction, space loss, posterior crossbite, open bite, midline asymmetry, crowding, and molar sagittal malocclusions.[1] In addition, clear aligner therapy is used in the early treatment of dental anterior crossbites.[2] From a clinical point of view, aligners have been proposed as an alternative to traditional slow maxillary expanders.[3,4] Lombardo et al.[5] reported significant morphological modifications in the upper arch form with the alignment of anterior teeth compared to rapid maxillary expander treatment.
In recent years, mandibular advancement with CAT has been used for retrognathic Class II malocclusion patients with late mixed to permanent dentition.[6] Considering the goal of the functional treatment, aligners provide better control of the upper anterior teeth position.[7] In addition to esthetic and comfort advantages, significant modifications of gingival contour have resulted in better smile harmony with the Invisalign First system.[8] Undoubtedly, most aligner companies will continue to announce various alternatives, and they will be used increasingly for children and adolescents in the near future.
According to a recent systematic review, aligner attachments are required to increase the treatment efficiency and 3D control of tooth movement during CAT process.[9] In a recent study, Yaosen et al.[10] stated that patient-related risk factors causing attachment loss can be prevented. Based on this, operator-related factors should be minimized to provide adequate attachment bond strength. Therefore, it is particularly important to select a proper composite material with good bonding performance. However, limited data are available in the literature regarding this issue. Barreda et al.[11] reported significant differences in the surface wear of a micro-hybrid type of highly viscous composite. In another study, aligner fitting with conventional bulk-fill composite was improved as compared to flowable resins.[12] In addition, Weckmann et al.[13] confirmed the highest precision using a high-viscous composite with a two-phase procedure and a low-viscous composite with a direct procedure without perforation in the template reservoir. To the best of our knowledge, only one study has assessed the bond strengths of aligner attachment using both a low-viscosity flowable and two high-viscosity composites on permanent teeth. Consequently, a relatively lower bond strength with the shortest chair time was reported when flowable composite was used with the total-etching technique.[14]
With the increasing demand for CAT, attachment bonding requires adhesion protocols for primary as well as permanent teeth. Considering the difficulties in salivary control and isolation in uncooperative pediatric patients who are supposed to be non-compliant during bonding of aligner attachments, the need to decrease the number of bonding steps required for resin materials and techniques is crucial in clinical practice. In this regard, the use of self-adhering composites integrated with primer and different techniques with various flowable composites may be questionable for the bonding of aligner attachments to primary teeth.
The purpose of this in vitro study was to evaluate the effectiveness of different flowable composites with universal adhesive (self- or total-etch [SE or TE] mode) and self-adhering composites after acid etching in the bonding of aligner attachments to primary enamel. The remnant amount of aligner attachment was also investigated. The null hypothesis of this study was that there would be no differences in the bond strength and remnant amount of aligner attachments when different composites and techniques were used on primary teeth.
MATERIAL AND METHODS
Sample size calculation
This study was approved by the Ethics Committee of Pamukkale University (25.05.2021/10). The sample size calculation was performed using G*Power software (version 3.1.9.7; Franz Faul, Kiel University, Kiel, Germany) to achieve a statistical power of 80% with a significance level of 5%, taking into account an effect size of 0.50. The required attachment size was calculated as 72 for eight groups. A sample of 10 teeth per group was included in this study design.
Sample selection and study groups
This study was performed on 80 extracted primary molars with no caries or enamel defects on vestibular surfaces. All teeth were stored in a thymol solution until the test procedure was carried out. The teeth were randomly divided into eight study groups according to the technique and composite used for attachment bonding:
Group TE + GC aligner connect (GAC): TE bonding with orthodontic aligner composite
Group TE + G-aenial universal injectable (GUI): TE bonding with universal restorative flowable composite
Group TE + Estelite universal super low flow (ESFL): TE bonding with supra-nano restorative flowable composite
Group SE + GAC: SE bonding with orthodontic aligner composite
Group SE + GUI: SE bonding with universal restorative flowable composite
Group SE + ESFL: SE bonding with supra-nano restorative flowable composite
Group GC ortho connect flow (GOCF): Acid etching with self-adhering flowable orthodontic composite
Group GC ortho connect (GOC): Acid etching with self-adhering orthodontic composite.
Attachment preparation and bonding procedure
The primary molars were inserted into the phantom models to produce aligner templates. Once the models were created, they were scanned with a scanner, and STL data were sent to the aligner manufacturer (Marmara, İstanbul, Turkey) to fabricate the templates for attachment placement. The horizontal rectangular beveled attachments were prepared with dimensions of 3 mm in width, 2 mm in height, and 0.25 mm in depth toward the distal and 1.25 mm in depth toward the mesial side of primary teeth, and then positioned on vestibular surfaces with the Nemocast software. The study models were produced with a 3D printer (Anycubic Photon Mono X, Shenzhen, China), and thermoplastic material (Erkodur) of 0.8 mm thickness was used to prepare the aligner templates.
Before the bonding procedure, the enamel surfaces were cleaned with fluoride-free paste at low speed and then washed and air-dried. When acid etching was required, 37% phosphoric acid (Pulpdent Corporation, Watertown, MA, USA) was applied for 30 s and then washed and air-dried until a chalky surface was observed. Universal bonding agent (G-Premio Bond, GC Corp., Tokyo, Japan) was used in the TE or SE mode when it was necessary to use a primer.
The aligner (GAC), universal flowable restorative (GUI), supra-nanofilled flowable restorative (ESFL), and two one-step orthodontic (GC Ortho Connect Flow and GC Ortho Connect) composites were used in this study. Self-adhering composites were applied without primer after acid etching. The composites were tested based on the manufacturer of each composite, as shown in [Table 1], with one exception — a self-adhering flowable orthodontic composite.[15]
| Material | Manufacturer | Composition |
|---|---|---|
| GAC | GC Corp, Tokyo, Japan (filler ratio not available) | 4,4’-isopropylidenediphenol, ethoxylated and 2-methylprop-2-enoic acid, (octahydro-4,7-methano-1H-indenediyl) bis (methylene) bismethacrylate, 2,2-dimethyl-1,3-propanediyl bismethacrylate, 1,3,5-Triazine-2,4,6-triamine, polymer with formaldehyde, titanium dioxide, 2,2’-ethylenedioxydiethyl dimethacrylate, UDMA, Butylated hydroxytoluene, 2-(2H-benzotriazol-2-yl)-p-cresol, diphenyl (2,4,6-trimethylbenzoyl) phosphine oxide, 6-tert-butyl-2,4-xylenol |
| GUI | GC Corp, Tokyo, Japan | Dimethacrylate monomers, Barium glass, silica 69% wt |
| ESFL | Tokuyama Dental Co., Tokyo, Japan | Bis-GMA, Bis-MPEPP, TEGDMA, UDMA, Supra-nano spherical filler 70% wt |
| GOCF | GC Corp, Tokyo, Japan (filler ratio not available) | Bisphenol A ethoxylate dimethacrylate, barium monoxide, diurethane dimethacrylate, mixture of isomers, α-Alumina, diboron trioxide, 2-propenoic acid, benzoic acid, 4-(dimethylamino), phenol, silane amine, phosphine oxide, silica[13] |
| GOC | GC Corp, Tokyo, Japan (filler ratio not available) | 4,4’-Isopropylidenediphenol, ethoxylated and 2-methylprop-2-enoic acid, 7,7,9-trimethyl-4, 13-dioxo-3, 14-dioxa-5, 12-diazahexadecane-1, 1–6 diylbismethacrylate, methacryloyloxydecyl dihydrogen phosphate, 6-tert-butyl-2,4-xylenol |
GAC: GC aligner connect, GUI: G-aenial universal injectable, ESFL: Estelite universal super low flow, GOCF: GC ortho connect flow, GOC: GC ortho connect
The flowable composites were loaded into each hollow of the attachment template using its thin tip syringe, while a thicker dispensing tip was used for self-adhering orthodontic composite due to its viscosity. When the composite was loaded, it was fully adapted onto the teeth, and gentle pressure was applied around each attachment with a metallic spatula. Finally, resin attachments were light-cured using LED polymerization light (VALO, Ultradent Products Inc., South Jordan, USA) according to the manufacturers’ recommendations. Finally, the excessive composites were removed with tungsten carbide burs. Finally, the excessive composites were removed with tungsten carbide burs with the aid of black light lens.
Thermal cycling and shear bond strength (SBS) test
After the bonding procedure, each primary tooth was separated from its phantom model and inserted into autopolymerizing acrylic blocks. Then, the specimens were kept in distilled water for 24 h. The thermocycling process was carried out between 5°C and 55°C with a dwell time of 30 s at 1000 cycles. The micro-SBS testing unit was used at a crosshead speed of 0.1 mm/min to evaluate the bond strength of the aligner attachment prepared on primary teeth.
Assessment of remnant resin attachment
After SBS test, the amount of remnant resin attachment was scored under stereomicroscopy (Olympus, SZ61, Munster, Germany) at 20× magnification according to the “resin attachment remnant index (RARI)” as follows: 0: No resin attachment on the surface, 1: <25% of the resin attachment left on the surface, 2: More than 25% and <50% of the resin attachment left on the surface, 3: More than 50% of the resin attachment left on the surface, and 4: Surface damage [Figure 1].
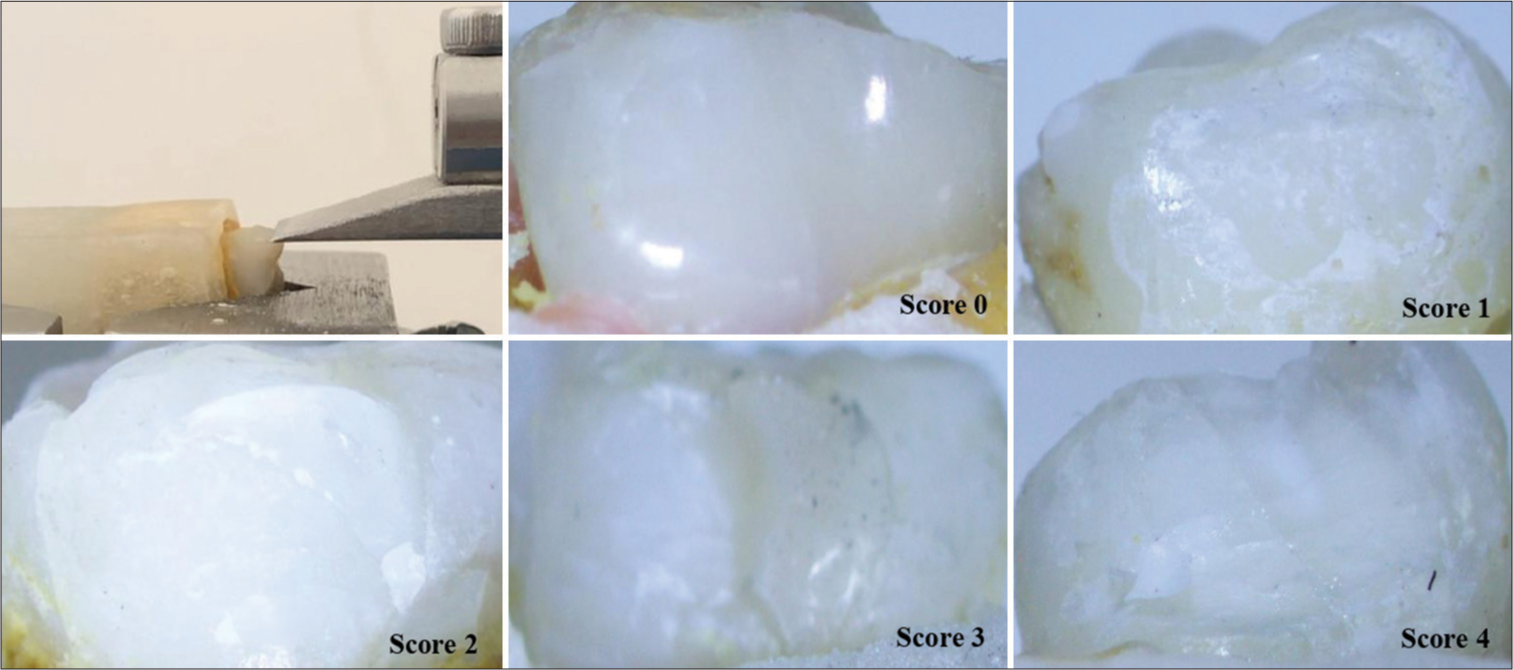
- The shear bond strength test and resin attachment remnant index scores.
Statistical analysis
The data were analyzed with SPSS software (version 21.0, SPSS Inc., Chicago, IL, USA). The Shapiro–Wilk test was used to determine the normality of the distribution. The Kruskal– Wallis and Mann–Whitney U-tests were used to compare the bond strength values. The RARI scores were analyzed using Chi-square analysis. The statistical significance level was set at P < 0.05.
RESULTS
Bond strength
The lowest SBS was found in the self-etching bonding technique with the aligner composite, while the highest SBS was in the TE bonding technique with the same composite, as shown in [Table 2]. The SBS results were demonstrated as box plots in [Figure 2]. There were significant differences between the groups in terms of SBS values (P < 0.05). The SE bonding technique with aligner composite showed significantly lower SBS values than the other groups, except for restorative universal composite. Self-adhering and total-etching composites demonstrated similar SBS values, irrespective of their different types.
| n | Mean±SD | Median | Min-max | P | |
|---|---|---|---|---|---|
| Total-etching composites | |||||
| Group TE+GAC | 10 | 23.04±3.40a | 24.35 | 7.70–38.21 | 0.001* |
| Group TE+GUI | 10 | 22.93±3.11a | 23.13 | 6.12–38.37 | |
| Group TE+ESFL | 10 | 19.77±2.78ad | 23.15 | 6.10– 28.91 | |
| Self-etching composites | |||||
| Group SE+GAC | 10 | 8.82±1.15b | 8.50 | 4.13–15.61 | |
| Group SE+GUI | 10 | 12.58±1.52bde | 12.64 | 7.20–19.95 | |
| Group SE+ESFL | 10 | 13.41±0.69cdf | 13.98 | 9.25–15.49 | |
| Self-adhering composites | |||||
| Group GOCF | 10 | 22.77±2.31a | 23.92 | 8.72–30.90 | |
| Group GOC | 10 | 21.09±3.64aef | 20.24 | 6.78–38.92 |
TE: Total-etch, SE: Self-etch, GAC: GC aligner connect, GUI: G-aenial universal injectable, ESFL: Estelite universal super low flow, GOCF: GC ortho connect flow, GOC: GC ortho connect, SBS: Shear bond strength. *Kruskal–Wallis test. Different letters show significant differences between groups based on Mann–Whithey U-test, SD: Standard deviation

- The shear bond strength values of study groups.
Amount of remnant resin attachment
No resin attachment remained on primary enamel surfaces in the SE bonding group with aligner composite, as shown in [Table 3]. One specimen for each score is demonstrated in [Figure 1]. According to the remnant amount of resin attachment, there were significant differences between the groups (P = 0.026, P < 0.05). The amount of remnant attachment was significantly higher in the total-etching and self-adhering groups compared to the SE bonding group with aligner composite (P < 0.05). Moreover, the remnant amount of adhesive was significantly higher in the TE bonding group with aligner composite than in the self-etching groups (P < 0.05). Similar findings were found for the TE bonding group with supra-nano restorative flowable composite, as shown in [Table 3].
| RARI scores | ||||||
|---|---|---|---|---|---|---|
| 0 (%) | 1 (%) | 2 (%) | 3 (%) | 4 (%) | P | |
| Total-etching composites | ||||||
| Group TE+GACA | 3 (30) | 3 (30) | 2 (20) | 0 (0) | 2 (20) | 0.026* |
| Group TE+GUIAC | 5 (50) | 3 (30) | 1 (10) | 1 (10) | 0 (0) | |
| Group TE+ESFLA | 3 (30) | 5 (50) | 0 (0) | 2 (20) | 0 (0) | |
| Self-etching composites | ||||||
| Group SE+GACB | 10 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Group SE+GUIBCD | 7 (70) | 3 (30) | 0 (0) | 0 (0) | 0 (0) | |
| Group SE+ESFLBCE | 8 (80) | 2 (20) | 0 (0) | 0 (0) | 0 (0) | |
| Self-adhering composites | ||||||
| Group SE+GOCFADE | 4 (40) | 6 (60) | 0 (0) | 0 (0) | 0 (0) | |
| Group GOCADE | 6 (60) | 2 (20) | 0 (0) | 1 (10) | 1 (10) | |
| Total | 46 (57.5) | 24 (30) | 3 (3.75) | 4 (5) | 3 (3.75) | |
TE + GAC: Total-etch + GC aligner connect, TE + GUI: Total-etch + G-aenial universal injectable, TE + ESFL: Total-etch + Estelite universal super low flow; SE+GAC: Self-etch + GC aligner connect, SE + GUI: Self-etch + G-aenial universal injectable, SE+ ESFL: Self-etch + Estelite universal super low flow, SE+ GOCF: Self-etch +GC ortho connect flow, GOC: Ortho connect flow, RARI: Resin attachment remnant index. The same letters show no significant differences.. *P<0.05
DISCUSSION
During attachment bonding, efforts to reduce sensitivity and chair time depend on decreasing the number of bonding steps; however, simplified procedures, such as eliminating acid etching for permanent teeth, lead to undesirable decreases in the bond strength.[16,17] Given recent improvements in materials, instead of using a conventional (three-step) technique, orthodontic bonding was performed with self-adhering composites without the need for a primer application. It achieved acceptable bond strengths, taking into consideration the advantages of saliva isolation and moisture control, and saved both time and money.[18-21] Further, universal adhesives seemed to be a viable alternative for the bonding of orthodontic attachments.[22] Although many alternatives are available, G-Premio Bond is a universal, eight-generation bonding agent with multi-mode etching.
Recently, the SE mode of this universal adhesive was recommended for attachment bonding with the use of a specially formulated aligner composite.[23] In this context, a better understanding of different composites and knowledge of adhesion protocols were considered essential for preparing proper aligner attachments on primary enamel. Further, there was no available data regarding this issue. Therefore, this was the first study that compared different flowable composites combined with TE or SE modes of universal adhesive and self-adhering orthodontic adhesives in terms of bonding effectiveness. Based on our results, statistical differences were found in SBS values and RARI scores. The null hypothesis was rejected.
According to the SBS results, the composites with the SE mode of universal adhesive showed significantly lower bond strength than flowable (GUI) and aligner composites when used with the TE mode of universal adhesive. The aligner composite, when used with a self-etching technique, demonstrated a pronounced decrease in the SBS compared to both total-etching and self-adhering composites. In accordance with these findings, the simplification of the bonding procedure with self-etching systems decreased the bond strength compared to the total-etching technique.[24] Cerone et al.[25] reported that the SE mode of universal adhesives resulted in inadequate SBS values for orthodontic brackets. The present study revealed that acid etching should be considered an important step during the bonding of aligner attachments to primary enamel for the aforementioned two composites because greater bond strength was observed after acid etching and it improved the bonding mechanism to primary enamel by increasing surface roughness.[26] This situation could be favorable when stronger aligner attachment bond strength is required in clinical practice. At that point, Estelite composite was slightly different from the other restorative resins because no statistical difference was found in terms of total- and self-etching techniques. The spherical fillers and particle size, with an average of 200 nm, could have contributed to these differences by improving the mechanical and flow properties of the supra-nanofilled flowable composite. However, the SBS value (~14 MPa) obtained with Estelite was considered inadequate for primary teeth.
The SBS results clearly indicated that an evaluation of remnant amounts of resin attachment or enamel damage was necessary after the detachment to achieve a better understanding of bonding effectiveness. Although there would be no attachment debonding, as in the bracket, the measurement of remnant amounts of attachment would give us an idea of the bonding strength. At present, there is no method to assess the remnant clear aligner attachment on the tooth’s surface. With this in mind, we developed RARI based on the original description by Artun and Bergland[27] and used it in the present study. The obtained data supported the idea that RARI would be useful for future studies.
According to RARI scores, self-etching bonding with different composites showed less remnant resin attachment. Moreover, no resin attachment remained on the enamel surfaces when the aligner composite was used with the self-etching technique, supporting the lowest bond strength. When the same composite was used with the total-etching technique, the highest SBS value approached the critical value (~40 MPa), which exceeded the cohesive strength of enamel.[28] The detachment resulted in surface damage. Similar SBS results were observed with the universal flowable restorative composite (GUI) and TE bonding techniques, apart from one exception of no enamel damage. In fact, in clinical practice, the aligner attachments are left on the primary teeth or are usually removed with a carbide bur after the treatment. Considering that the attachment prepared on primary teeth would not be subject to the same debonding force as in a bracket, the observed enamel fractures were considered clinically insignificant in the present study.
The self-adhering orthodontic composites provided SBS results similar to total-etching composites but with the advantage of time savings. In addition, the risk of saliva contamination was reduced with the exclusion of the primer application, and there was no risk of exposure to unpolymerized monomers. The RARI findings revealed that the behavior of self-adhering orthodontic adhesives was not significantly different when compared to total-etched composites during the detachment. This could be a result of the surface roughness that may have allowed the penetration of primer-integrated composites into the porous enamel surfaces. This explanation was in accordance with the findings of lower SBS values with less resin attachment left on enamel surfaces, which indicated a weaker bond strength in the enamel and composite interfaces.
The major limitation of this study was that the bonding results were not perfectly reflective of clinical practice, although the test procedure aimed to imitate intraoral conditions. Another limitation was that there was no available data to allow an evaluation of aligner attachment bond strength prepared on primary teeth. Thus, comparing the results with the previous studies was not possible. The present findings should be regarded as preliminary. The future studies will be necessary to confirm the efficacy of aligner and self-adhering composites in clinical conditions.
CONCLUSION
Within the limitations of this study, one of the following alternatives can be recommended for the bonding of aligner attachments to primary teeth:
Orthodontic aligner composites or restorative composites can be used in the total-etching mode of universal adhesive
Self-adhering orthodontic composites may be preferred to reduce the number of bonding steps.
Ethical approval
This study was approved by the Ethics Committee of Pamukkale University (25.05.2021/10).
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Interceptive treatment with invisalign(®) first in moderate and severe cases: A case series. Children (Basel). 2022;9:1176.
- [CrossRef] [PubMed] [Google Scholar]
- Indication of clear aligners in the early treatment of anterior crossbite: A case series. Dental Press J Orthod. 2020;25:33-43.
- [CrossRef] [PubMed] [Google Scholar]
- Maxillary expansion with clear aligners in the mixed dentition: A preliminary study with invisalign® first system. Eur J Paediatr Dent. 2021;22:125-8.
- [Google Scholar]
- Upper arch dimensional changes with clear aligners in the early mixed dentition: A prospective study. J Orofac Orthop. 2023;84:33-40.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the upper arch morphological changes after two different protocols of expansion in early mixed dentition: Rapid maxillary expansion and invisalign(®) first system. Life (Basel). 2022;12:1323.
- [CrossRef] [PubMed] [Google Scholar]
- Align Technology. Mandibular Advancement. Available from: https://info.aligntech.com/MA. 22 [Last accessed on 2022 Sep 19]
- [Google Scholar]
- Mandibular advancement with clear aligners in the treatment of skeletal Class II. A retrospective controlled study. Eur J Paediatr Dent. 2021;22:26-30.
- [Google Scholar]
- Gingival margins' modifications during orthodontic treatment with invisalign first(®): A preliminary study. Children (Basel). 2022;9:1423.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of composite attachments on orthodontic clear aligners therapy: A systematic review. Materials (Basel). 2022;15:533.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors of composite attachment loss in orthodontic patients during orthodontic clear aligner therapy: A prospective study. Biomed Res Int. 2021;2021:6620377.
- [CrossRef] [PubMed] [Google Scholar]
- Surface wear of resin composites used for invisalign® attachments. Acta Odontol Latinoam. 2017;30:90-5.
- [Google Scholar]
- Scanning electron microscopy analysis of aligner fitting on anchorage attachments. J Orofac Orthop. 2019;80:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of attachment bonding protocol on precision of the attachment in aligner treatments. J Orofac Orthop. 2020;81:30-40.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of three composite materials in bonding attachments for clear aligners. Orthod Craniofac Res. 2021;24:520-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anti-microbial and remineralizing properties of self-adhesive orthodontic resin containing mesoporous bioactive glass. Materials (Basel). 2021;14:3550.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontic bonding with self-etching primer and self-adhesive systems. Eur J Orthod. 2011;33:276-81.
- [CrossRef] [PubMed] [Google Scholar]
- Inadequate shear bond strengths of self-etch, self-adhesive systems for secure orthodontic bonding. Dent Mater J. 2012;31:947-53.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of one-step orthodontic adhesive on microleakage and bracket bond strength: An in vitro comparative study. Int Orthod. 2020;18:366-73.
- [CrossRef] [PubMed] [Google Scholar]
- Single-component orthodontic adhesives: Comparison of the clinical and in vitro performance. Clin Oral Investig. 2021;25:3987-99.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of shear bond strength of a primer incorporated orthodontic composite resin: An in-vitro study. Cureus. 2022;14:e24088.
- [CrossRef] [Google Scholar]
- Comparison of microleakage and shear bond strength of ribbon and twisted wire retainers bonded on human mandibular incisors with two different types of adhesives with and without primer: An in-vitro study. Int Orthod. 2022;20:100693.
- [CrossRef] [PubMed] [Google Scholar]
- The performance of universal adhesives on orthodontic bracket bonding. Eur J Gen Dent. 2021;10:19-24.
- [CrossRef] [Google Scholar]
- Available from: https://www.gc.dental/ortho/en-US/products/alignerconnect# accessed on 2022 Sep 20
- Self-etching adhesives: Review of adhesion to tooth structure part I. SADJ. 2004;59:413, 415-7, 419
- [Google Scholar]
- Bond strength of universal self-etch 1-step adhesive systems for orthodontic brackets. J Can Dent Assoc. 2019;85:j6.
- [CrossRef] [Google Scholar]
- The enamel surface and bonding in orthodontics. Semin Orthod. 2010;16:37-48.
- [CrossRef] [Google Scholar]
- Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333-40.
- [CrossRef] [PubMed] [Google Scholar]
- Ultimate tensile strength of tooth structures. Dent Mater. 2004;20:322-9.
- [CrossRef] [PubMed] [Google Scholar]







