Translate this page into:
Presurgical Nasoalveolar Molding in a 4-day-old Infant with Unilateral Cleft Lip, Alveolus, and Palate Deformity
Address for correspondence: Dr. Abin Mathew, Department of Orthodontics, Coorg Institute of Dental Sciences, Coorg, Virajpet, Karnataka, India. E-mail: abinz143@gmail.com
This article was originally published by Wolters Kluwer and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction
A four day old male infant was referred to our department. Infant’s mother complained of an opening over lip and difficulty in feeding and desires to get it corrected. On clinical examination patient showed complete unilateral cleft lip, alveolus and palate deformity towards the left side.
Methods
On the initial visit, lip taping using 1/4inch 3M Steri-strip was applied and instructions were given to parents about lip taping, and advised to continue lip taping for 2 weeks. Initial impressions were taken to fabricate the Presurgical nasoalveolar molding appliance. Intraoral molding plate was made to approximate the maxillary segments. Nasal stent was added to correct the nose deformity. Presurgical impressions were made.
Results
Under this pre surgical treatment, the cleft alveolus reduced in size from 13mm to 3mm at the alveolar ridge and palate, respectively. The nasal wing was lifted considerably.
Conclusion
Pre-surgical nasoalveolar moulding helped to reduce the cleft gap, improve the arch form, approximate lip segments and distinctly improve the morphology of the nose by correcting flattened nasal wings. This aforementioned correction not only enabled better aesthetic results after surgery but also reduced tissues tension and scar formation post-surgery.
Keywords
Cleft lip
cleft palate
presurgical nasoalveolar molding
Introduction
The most common congenital malformation is cleft of the lip, alveolus, and palate (CLAP). Approximately in India, out of 24.5 million births per year, the birth prevalence of clefts is amid 27,000 and 33,000 clefts.[1]
Grayson and Cutting in 1988 combined the concept of presurgical orthopedics and presurgical treatment of the cleft lip nasal deformity and developed the concepts of presurgical nasoalveolar molding (PNAM), which combined a nasal molding stent with a passive, presurgical molding appliance in treating cleft lip and palate in infants.[2]
The primary aim of PNAM is reduction in soft-tissue and cartilaginous deformities to facilitate surgical soft-tissue repair in optimal conditions under minimal tension to minimize scar formation.[3,4,5]
PNAM has become one of the important components in the management of cleft of the lip, alveolus, and palate (CLAP) as it solves most of the problems associated with CLAP. PNAM aids in alignment and approximation of the alveolar cleft segments, to correct the malposition of the nasal cartilage and reduce soft-tissue deformity by correcting the nasal tip, alar base, and the position of philtrum and columella. PNAM produces an overall improvement in the esthetics of the nasolabial complex in cleft patients while minimizing the extent of the surgery and the overall number of further surgical procedures. This clinical report describes Figueroa-modified PNAM technique for an infant with complete unilateral cleft lip, palate, and alveolus deformity, showing significant reduction in cleft defect size and improved anatomy and topography of deformed surrounding soft tissues.
Case Report
A 4-day-old infant (male) was referred to our department. The patient’s mother complained of an opening over the lip and difficulty in feeding and desired to get it corrected. On clinical examination, the patient showed complete unilateral cleft lip, alveolus and palate deformity toward the left side. The patient weighed 3 kg when checked on the initial visit [Figure 1a-d].

- (a-d) Prenasoalveolar molding photos
After a thorough evaluation, nasoalveolar molding (NAM) therapy was planned for the patient. The parents were counseled properly about the procedure, duration, and prognosis of treatment, and their active involvement during the PNAM process was explained. On the initial visit, primary impression was made using a wax sheet dipped and softened in mild warm water, then primary cast was poured, and a special tray was fabricated using acrylic resin to take the secondary impression. On the first visit itself, lip taping was done using 3M™ Steri-Strip™. A base tape was placed and a hydrocolloid type bandage, was placed over the cheeks. It serves as a barrier between the retention tapes and the cheeks to minimize tissue irritation. Instructions were given to parents about lip taping and were advised to continue lip taping for 2 weeks [Figure 2a-g].

- (a-g) Primary impression with soft wax, special tray fabricated, and lip taping
After 2 weeks, secondary impression of the intraoral cleft defect was made using an elastomeric material in the infant’s acrylic special tray. While making secondary impression, the baby was fully conscious and kept in his mother’s lap with head facing downward and the mother’s hands supporting the baby’s chest and lap region to avoid any aspiration of liquid or impression material.
Traditional Figueroa NAM requires weekly or biweekly adjustments to remove acrylic resin from the palatal plate to narrow the alveolar gap; these frequent adjustments create a burden for patients living far from a hospital. To minimize this burden, we developed a modified NAM technique with an active palatal plate where the cleft alveolus is free to approximate physiologically with the pressure exerted by the plate. In the cleft region of the cast, undercuts were blocked out with utility wax. The molding appliance was then fabricated with self-cure hard clear acrylic resin. A retentive button was fabricated with the same material and placed in the anteroinferior cleft region of the molding plate at an angle of 45° to the imaginary occlusal plane. A well-finished and polished molding plate was inserted into the infant’s mouth on the same day to promote feeding as that was one of the chief complaints of the infant’s mother. Small orthodontic elastics of 0.25” diameter were added to the loops of adhesive tapes (0.25” ×4”). The elastics were placed over the retentive button, and the adhesive tape was pulled and secured to the base tape on the infant’s cheek. The elastics were pulled approximately twice their resting diameter. The activation force can vary depending on the stage of the treatment and the clinical judgment [Figure 3a-h].

- (a) Heavy-bodied silicone material impression with tray, (b) impression showing cleft size, (c) cast poured showing cleft size of 13 mm, (d) cleft area blocked out with wax, (e) molding appliance fabricated with self-cure hard clear acrylic resin, (f-h) Lip taping and nasoalveolar molding plate without nasal stent given on the same day
After 2 months, the NAM plate was modified with bilobed nasal stent with a projection of acrylic supported by round stainless steel wire of 0.036G in the shape of swan neck, which was attached to the plate. Nasal stent was inserted passively into the nostril and covered with a thin veneer of soft acrylic to apply positive elastic pressure. This pressure aids to lift the collapsed nostril and in molding the nasal tissue. During follow-up visits, the molding plate as well as the nasal stent was modified by serial addition and subtraction of soft acrylic to get the desired shape of nostril, ala of nose, and to approximate the alveolar segment in a desired anatomy. The plate was activated by selective removal of hard acrylic resin from the region where the movement of bone was needed; at the same time, a soft denture liner was incorporated in the region where bone is required to be moved to close the cleft defect. The patient was evaluated at an interval of 2 or 3 weeks and the appliance was activated as per requirement. On each appointment, the infant’s weight was checked that showed a progressive good amount of increase of weight which indicated that NAM plate improved feeding. At the end of NAM, there was reduction in the alveolar cleft from 13 to 3 mm and the columella was lengthened and repositioned from an oblique position into an upright position, which resulted in improved nasal alar cartilage symmetry. The contour of the nostril on the cleft side resembles the nostril on the unaffected side and the infant weighed 9 kg [Figure 4a-g].
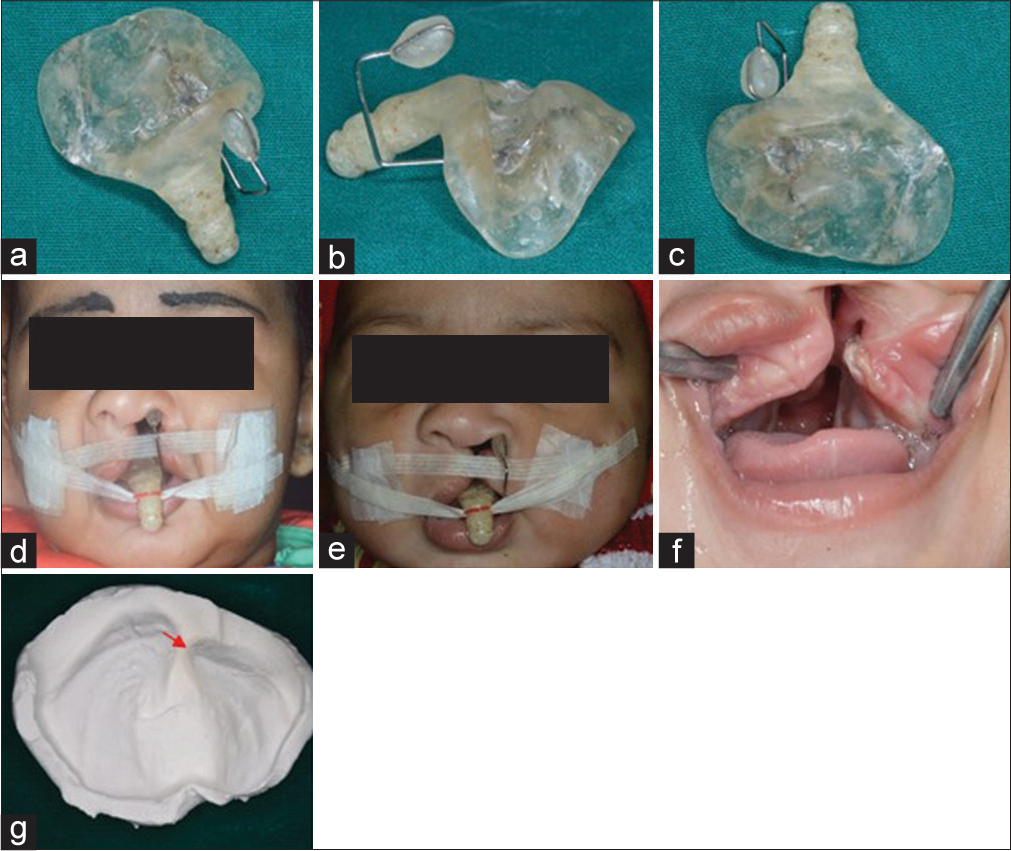
- (a-d) Nasoalveolar molding plate with nasal stent, extraoral picture with nasoalveolar molding plate having stent, (e) extraoral postnasoalveolar molding, (f) intraoral, (g) cast postnasoalveolar molding with reduced cleft size to 3 mm
After 5 months, lip surgery was performed. On 3-week follow-up postlip surgery, there is reduction in bi-alar width and lengthening of columella after molding [Figure 5a-f].

- (a and b) After 5 months, lip surgery was performed, (c-f) on 3-week follow-up postlip surgery, there is reduction in bi-alar width and lengthening of columella after molding
Discussion
At present, there are three different PNAM techniques routinely used, namely Grayson’s technique, Figueroa’s technique, and Liou’s technique.
Grayson’s technique
A passive-type orthopedic appliance is used together with taping of the lip for premaxillary and alveolar molding. The protruding premaxilla is molded first into a proper position. When the alveolar gap is approximated and the arch is aligned, a nasal molding device is added to the orthopedic appliance to increase the columellar length as well as to reshape the alar dome. A nonsurgical lip adhesion is performed by placing tape across the upper lip. The tape aids in the closure of the clefts, decreases the width of the base of the nose, and helps to approximate the lip.[6,7]
Figueroa’s technique
Alveolar molding and nasal molding are performed simultaneously using an acrylic plate with rigid acrylic nasal extension. Rubber bands are connected to the acrylic plate for gentle retraction of the premaxillary backward. A soft resin ball attaching to the acrylic plate across the prolabium is sometimes used to maintain the nasolabial angle.[8]
Liou’s technique
The NAM device is composed of a dental plate, two nasal components for nasal molding, and several micropore tapes for premaxillary retraction. Denture adhesive (Poligrip, Australia) keeps the dental plate on the maxillary lateral segments. The nasal components are made up of 0.028” stainless steel wire projecting forward and upward bilaterally from the anterior part of the dental plate. The top portion contains a soft resin molding bulb that fits underneath the nasal cartilages for nasal molding. Micropore tapes are placed across the cleft lips and prolabium to minimize the alveolar cleft and retract the premaxilla. At the same time, they pull both alar bases medially. Retraction of the premaxilla and lengthening of the columella are performed at the same time. The columella is lengthened and stretched by pulling on the premaxillary backward. The nasal tip is kept at the same height while the premaxilla is pulled back. Rather than pushing forward, the soft resin molding bulbs basically support the nasal cartilages and nasal tip.[9] NAM techniques require regular patient follow-up with an interval of 1–2 weeks.
Grayson’s technique approximates the alveolar cleft before the nasal molding. Both Figueroa’s and Liou’s methods achieve nasal and alveolar molding at the same time. Grayson’s technique, with emphasis on approximating the alveolar clefts before nasal molding, achieves the best preoperative nasal shape symmetry and skeletal base balance. However, it is also the most expensive and time-consuming method. Figueroa’s and Liou’s techniques of performing alveolar and nasal molding at the same time are simpler and less expensive methods.
The technique of NAM followed by us was a modified version of traditional Figueroa NAM method so that the frequent adjustments can be avoided which often lead to poor support of parents toward NAM therapy, also wherein alveolar and nasal molding are done at the same time. The rationale behind this was the acquired maternal estrogen before birth results in decrease in elasticity and increase in plasticity of cartilages. It has been assessed by Matsuo et al. that the temporary plasticity of nasal cartilage is believed to be caused by high levels of maternal hyaluronic acid, a component of the proteoglycan intercellular matrix, which is found circulating in the infant for several weeks after birth.[2,4] Advantages of NAM are the ability to guide the alveolar segments to a more normal position prior to surgery and reduction of the cleft gap facilitates the primary gingivoperiosteal closure of cleft defect because there is a greater probability that a complete osseous bridge formation will happen when cleft width is reduced. The combined action of NAM plate and nonsurgical lip approximation with lip taping results in a predictable correction of the nasal, alveolar, and soft-tissue deformities. As a result under surgical repair, the lip and nose heal under minimal tension with no or minimal scar formation.
There are few serious complications associated with NAM. The most common is irritation of the oral mucosal or gingival tissue. Intraoral tissues may ulcerate from pressure or rubbing. Common areas of breakdown are the frenum attachments, the anterior premaxilla, and the posterior fauces as the molding plate is retracted. The infant should be checked at each visit, and the molding plate should be properly relieved in all areas that are exerting excessive pressure. The intranasal lining of the nasal tip can become inflamed if too much force is applied by the upper lobe of the nasal stent. Notching along the alar rim can occur if the lower lobe is not positioned or shaped correctly. The area under the horizontal prolabium band can become ulcerated if the band is too tight.
The most common area of soft-tissue irritation is the cheeks. The tapes should be removed slowly and carefully to avoid skin irritation. Tape removal solvents or warm water can facilitate the removal of tapes. If the tissue remains irritated, a skin barrier such as DuoDerm® or Tegaderm™ can be used as a base on which the tape-elastic retraction system can be attached. It is sometimes recommended that aloe vera gel be applied to the cheeks when changing tapes. Poor compliance by the parents can cause loss of valuable treatment time.
At the conclusion of our modified method of NAM therapy, we observed increase in nostril height and columellar angle and decrease in intersegmental distance, bi-alar width, and nostril width.
Conclusion
PNAM, when used prior to primary surgical lip repair, will give psychological reassurance to parents and child, enhance surgical outcome, reduce the need for revision surgeries in the future, and also reduce the overall cost of treatment. A well-executed PNAM process by a committed team of dentists and surgeons supported by good compliance of the parents and child may prove to be a boon for (CLAP) cleft lip, alveolus andpalate child. Results of PNAM are promising for a child with CLAP, hence are encouraged to be used promptly after the birth and continued till further specific corrective surgeries are performed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology-clinical profi le of cleft lip and palate among children in India and its surgical consideration. J Surg. 2013;2:45-51.
- [Google Scholar]
- Reduced need for alveolar bone grafting by presurgical orthopedics and primary gingivoperiosteoplasty. Cleft Palate Craniofac J. 1998;35:77-80.
- [CrossRef] [Google Scholar]
- Presurgical nasoalveolar orthopedic molding in primary correction of the nose, lip, and alveolus of infants born with unilateral and bilateral clefts. Cleft Palate Craniofac J. 2001;38:193-8.
- [CrossRef] [PubMed] [Google Scholar]
- Presurgical orthopedics for cleft lip and palate In: Aston SJ, Beasley RW, Thorne CH, eds. Grabb and Smith’s Plastic Surgery (5th ed). Philadelphia: Lippincott-Raven; 1997. p. :237-44.
- [Google Scholar]
- Long Term Study of Midface Growth in Unilateral Cleft Lip and Palate Patients Following Gingivoperiosteoplasty. Chapel Hill: American Cleft Palate Craniofacial Association; 1999.
- Nonsurgical correction of congenital auricular deformities in the early neonate: A preliminary report. Plast Reconstr Surg. 1984;73:38-51.
- [CrossRef] [Google Scholar]
- Preoperative columella lengthening in bilateral cleft lip and palate. Plast Reconstr Surg. 1993;92:1422-3.
- [Google Scholar]
- Orthodontics in cleft lip and palate management In: Mathes SJ, Hentz UR, eds. Plastic Surgery (2nd ed). Philadelphia, PA: Saunders; 2006. p. :271-310.
- [Google Scholar]
- Progressive changes of columella length and nasal growth after nasoalveolar molding in bilateral cleft patients: A 3-year follow-up study. Plast Reconstr Surg. 2007;119:642-8.
- [Google Scholar]






